| Bell's mania | |
|---|---|
| Other names | Delirious mania |
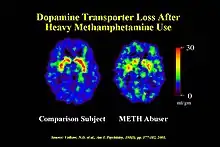 | |
| The hypothesized cause of Bell's mania is said to be abnormally elevated levels of extracellular dopamine. | |
| Specialty | Behavioral neurology, psychiatry |
| Symptoms | Hyperactivity, hyperthermia, delirium, disruption in psychomotor activities, emotional liability, fear, panic, aggression, violence, sensory dysfunction, death |
| Causes | Dysfunction of dopaminergic transporters, anomalous activation of the dorsal anterior cingulate, right inferior frontal cortical regions, excited hyperdopaminergic mechanism |
| Risk factors | Psychostimulant users and abusers, patients with drug withdrawal, undiagnosed/untreated psychiatric patients, people with severe manic episodes, sleep deprived individuals, people with medical history of neurological and physiological conditions |
| Differential diagnosis | Bipolar disorder, acute schizophrenia, catatonia, delirium |
| Treatment | Rapid sedation, intramuscular ketamine injections, electroconvulsive therapy, blood tests, regulation of body temperature. |
| Medication | Benzodiazepines, antipsychotic medication, ketamine injections, dantrolene |
Bell's mania, also known as delirious mania, refers to an acute neurobehavioral syndrome.[1] This is usually characterized by an expeditious onset of delirium, mania, psychosis, followed by grandiosity, emotional lability, altered consciousness, hyperthermia, and in extreme cases, death.[1] It is sometimes misdiagnosed as excited delirium (EXD) or catatonia due to the presence of overlapping symptoms.[2][3] Pathophysiology studies reveal elevated dopamine levels in the neural circuit as the underlying mechanism.[4][5] Psychostimulant users as well as individuals experiencing severe manic episodes are more prone to the manifestation of this condition.[6] Management solutions such as sedation and ketamine injections have been discussed for medical professionals and individuals with the condition. Bell's mania cases are commonly reported in countries like the United States and Canada and are commonly associated with psychostimulant use and abuse.[4]
Clinical features
The majority of Bell's mania cases studied are triggered by psychostimulant drug usage or preexisting medical or neurological conditions, which impedes the apprehension of this syndrome.[7] Hence at present, there is still no scientific consensus on the clinical features of Bell's mania. Researchers are currently working on varying case studies to derive common clinical characteristics. Some frequent signs and symptoms include acute onset of delirium, mania or psychosis.[8][3] Patients with Bell's mania have fluctuating severity of symptoms over time with altered consciousness and emotional lability.[9][6][10] They tend to be excited, agitated, paranoid, delusional and alarmed.[6][3][10] They display impulsive, hostile and destructive behavior towards others that can last for hours to days, as well as unexpected physical strength.[1] Catatonic symptoms such as grimacing, echopraxia, negativism, echolalia and stereotypy are often present.[11] Impaired concentration, memory loss, disorientation, insomnia, auditory and visual hallucinations are additional symptoms that follow.[6][10] There are shifts from having loud and disorganized speech to mutism.[6] Some typical physiological signs include hyperthermia, tachycardia, hypertension, and hyperventilation.[12]
Diagnosis
This condition is currently not recognized as a diagnosable issue by psychiatric journals such as the Diagnostic and Statistical Manual of Mental Disorders-IV[3] by the American Psychiatric Association or the tenth revision of the International Statistical Classification of Diseases and Related Health Problems by World Health Organization (WHO).[3]
Physical examination
When examined, patients with Bell's mania fail to recall names, recent experiences and are poorly oriented for location, date, and time.[12] Moreover, their blood pressure and respiratory rate are increased.[13] Additionally, mental status examination using questionnaires[13] and three diagnostic tests are taken, including drawing a clock-face,[14] The Face-Hand test[15] and Hidden figures tests.[16] Patients with Bell's mania tend to make obvious mistakes in these tests, for instance drawing a clock-face with incorrect numbering or missing clock hands.[14]
Differential diagnosis
Upon acute onset of the symptoms, an instant investigation for a toxic or systemic cause is undertaken.[12] Prominence of thought disorder, grandiosity and delusional ideation, and catatonic signs indicates the diagnosis of acute schizophrenia, bipolar disorder and catatonia respectively.[12] Diagnostic complications arise as these signs are also often the notable feature of Bell's mania.[8] With the cause undetermined, Bell's mania diagnosis is usually justified with the presence of both mania and delirium regardless of the catatonic symptoms.[12]
Distinguishing between Bell's mania and catatonia
Bell's mania and catatonia are regarded as "overlapping syndromes",[16] making differential diagnosis essential when catatonic signs are observed.[12] Thus, researchers must distinguish between excited catatonia and Bell's mania, and among malignant catatonia, excited catatonia, and neuroleptic malignant syndrome (NMS).[12] When catatonic features are prominent, it is diagnosed as excited catatonia and when absent or subtle, it is identified as Bell's mania.[12] Alternatively, the presence of delirium is recognized as the discerning factor. A difference between the two is that catatonia is viewed from a movement aspect, whereas delirium from consciousness.[7]
Nevertheless, a formal set of diagnostic criteria is required to distinguish between Bell's mania and catatonia.[11] Failure to diagnose Bell's mania appearing as catatonia could lead to deleterious consequences and, in worse cases, death.[1][8]
Pathophysiology
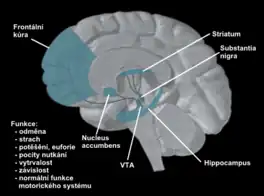
Dopamine is the primary neurotransmitter involved in the pathophysiology of Bell's mania.[3] Elevated dopamine levels in the neural circuit concerned with neuropsychiatric disorders are postulated to be responsible for the manic and psychosis symptoms and other signs, including fluctuations in body temperatures and fear.[17] Increased extracellular dopamine levels can be caused by low levels of dopaminergic transporters, sensitization of postsynaptic dopaminergic receptors, and dopamine transporters dysfunction.[6]
Role of genetics and signaling pathways
Mania is a prominent symptom of both bipolar disorder and Bell's mania. Hence, studying bipolar patients can provide insight into the pathophysiology of this Bell's mania. PET scans of manic patients illustrate anomalous activation of the dorsal anterior cingulate, right inferior frontal cortical regions.[6] Manic symptoms exacerbate with increasing anterior cingulate activation, which is posited to be associated with escalating dopamine transmission in the nucleus accumbens.[3]
Dopamine transporter regulates the reuptake of dopamine to keep the synaptic dopamine levels within normal range.[6] Hence, the elevation of such transporter levels in the striatum decreases neurotransmission.[18] Genetic studies have hypothesized a relationship between low transporter protein levels and the gene for dopamine transporter in bipolar affective patients.[6]
Stimulant elicited responses
Sensitization of postsynaptic dopaminergic receptors
External sources contributing to the hypothesized hyperdopaminergic mechanism include psychostimulants like cocaine.[6] These substances provoke behavioral changes similar to mania.[19] In chronic users, drug sensitization occurs which induces increased neurotransmission and modified protein expression within the mesolimbic dopamine neurons. Adaptations in dopamine transporters is further triggered causing behavioral sensitization.[20] This phenomenon is not distinct to drug abuse but also other psychomotor stimulants such as stress.[6]
Dopaminergic transporters dysfunction
Dopaminergic transporters dysfunction is caused by acute mania of bipolar disorder, psychostimulant use, and environmental stress. It is suggested to be common mechanism in excited delirium (EXD).[6] EXD is commonly observed in psychostimulant abusers as these drugs directly impact the dopaminergic transporters, increasing the extracellular dopamine levels.[21][6]
Amplified excitation of the dopaminergic systems can induce extreme fear and magnify both approach and avoidance behaviors.[6] The hyperdopaminergic state triggers aggression, agitation and psychomotor excitement.[6] Additionally, CNS dopamine signaling is active in heart rate, respiration and body temperature regulation.[22] Dopamine imbalance can hence result in hyperthermia, tachycardia, hyperventilation, hypertension and sleep disturbance symptoms.[6][3]
Risk Factors
Given that hyperdopaminergic state is postulated to be the underlying mechanism of Bell's Mania, people prone to dopamine imbalance, sensitization and low levels of dopamine transporters are susceptible.[6] Furthermore, this syndrome is usually precipitated from prevailing neurological and physiological conditions.[12] Hence, those at risk include
- Psychostimulant users and abusers[6]
- Patients who are drug withdrawal states or are non-compliant with psychotropic drugs[6][11]
- Undiagnosed/ untreated psychiatric patients[23][6]
- People with severe manic episodes[12][6]
- Sleep deprivation which can trigger and even worsen acute manic episodes[6]
- People with medical history of neurological and physiological conditions[12]
Treatment and Management
Whilst the scope of Bell's Mania is extensively studied, there remain some significant challenges that need to be solved with respect to treatment and management.[3]
Recognition
Over the course of time the significance of this syndrome has been increasingly recognized in correspondence to the manner of death, specifically because the anatomic cause of death is hard to define during autopsy. Recent studies have elicited neurochemical imbalances[24] resulting in autonomic hyperactivity and increase in dopamine levels in the victims.[3] Emergency personnel need to recognize these symptoms promptly to avoid the individual from spiraling into metabolic acidosis, rhabdomyolysis, multiorgan failure and ultimately death. In light of the clinical findings, some treatments have been described which include effective sedation, followed closely by external cooling, monitoring medical complications and the administration of intravenous (IV) fluids.[3]

Rapid Sedation
One management technique is rapid sedation in view of the unpredictable aggressive nature of the patient with Bell's Mania, especially if the symptoms that need to be handled are associated with the causes like dopamine regulation. Turning off the catecholamine cascade and rapidly sedating the patient using several sedatives like Benzodiazepines or Neuroleptics[25] can help. Several studies also point at the increased effectiveness of combination of two or more sedatives in the treatment of hyper agitated patients.[26][27]
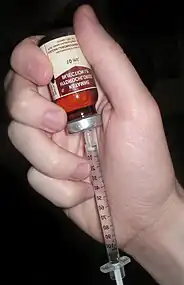
Intramuscular Ketamine Injections
Patients with Bell's mania may not have optimum time for the sedatives to start showing effect. Due to this fact, electroconvulsive therapy[1] and Intramuscular Ketamine injections[3] are alternative solutions that have been proposed. With an onset time of 30 seconds to 4 minutes ketamine proves to be more effective than Benzodiazepines.[28] Although adult data on the use of Ketamine on patients isn't readily available, a study by Strayer et al.[29] concluded that the use of ketamine for controlling the hyperactivity was reliable and can further facilitate other management techniques with fewer side effects.[30]
Other Preventative Measures
Along with sedation techniques, a few other prevention and protection measures can decrease fatal outcomes, some of which are:
- management of catecholamine cascade,
- basic medical monitoring of bodily functions,
- blood tests,
- physical examination and
- rapid cooling of the body temperature.[3]
The urgency and medical severity of the condition needs to be given impetus in terms of handling patients with Bell's Mania. Due to the homologous nature of this syndrome with malignant hyperthermia (MH) and neuroleptic malignant syndrome (NMS),[31] Dantrolene[32] is also a probable treatment route owing to its swift acidosis correction. Although more research is needed in correspondence to the cause and consequences of this disease, the significance of the behavioral and physical symptoms need to be given importance to provide medical institutions as well the constabulary the necessary information to respond to Bell's Mania appropriately.
Epidemiology
The first case of Bell's Mania was observed by medical examiners during the cocaine epidemic[33][6] in countries like the United States of America and Canada with some other cases being related to police brutality and restraint.[34] The term Bell's Mania was first coined to describe the clinical condition with a 75% mortality rate.[6] The prevalence of this condition ranges from 15% to 25% in the society and, is not an infrequent occurrence.[11]
History
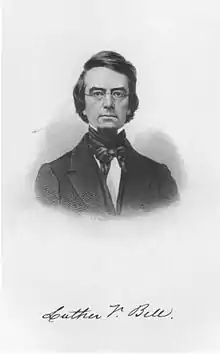
First mention of Bell's Mania
Bell's Mania is a syndrome with unexplained etiology which was first explained by American psychiatrist Luther Bell in the 1850s after observing institutionalized psychiatric patients. The first clinical reports and descriptions of people with acute exhaustive mania and delirium were provided by a few psychiatrists in the United States of America, France and the United Kingdom.[6] The description of the symptoms seemed to be quite similar to that of patients with schizophrenia (hallucinations and delirium) however additional hyperactivity, heightened arousal, and altered sleep cycle was also reported in patients with Bell's Mania.[6]
First Appearance of Related Symptoms
The suggestive symptoms of this disorder were first observed in the 19th century, out of which some of the most significant ones are the onset of aggression, bizarre behavior, violence, excessive shouting, panic, paranoia and increase in body temperature.[4] In 1934, Stauder described a series of acute onset of psychomotor agitation in young people with no history of physical or psychological disturbances.[35] He termed this description as Lethal Catatonia. Other reasons for the manifestation of Bell's Mania, points at the use of stimulant drugs in excessive amounts and also psychiatric diseases like depression or schizophrenia.[12][36]
In 1985, Bell's Mania was first mentioned in a definitive manner using the term Excited Delirium (EXD). Prior to that year, most cases of death by cocaine intoxication[37] during the cocaine epidemic that happened in a sudden manner. This involved the exposure to highly toxic amounts of the drug due to the bursting of cocaine packets being carried within the body by "body stuffers".[38] In the same year a series of observations were made by Welti and Fishbain regarding psychosis, cardiorespiratory arrest and sudden death[39] in individuals with cocaine addiction. Since the law enforcement were often called to contain violent behavior exhibited by these individuals. It was speculated that police brutality might be the underlying cause of the misshapen. Upon medical review of the cases related to the use of batons, pepper sprays and restraint methods[38] did not disclose any autonomic cause behind the death, albeit problems like cardiac diseases and trauma was excluded from the extensive evaluation.[38][4][5]
See also
References
- 1 2 3 4 5 Bobo, William V.; Murphy, Michael J.; Heckers, Stephan H. (May 2009). "Recurring episodes of Bell's mania after cerebrovascular accident". Psychosomatics. 50 (3): 285–288. doi:10.1176/appi.psy.50.3.285. ISSN 1545-7206. PMID 19567770.
- ↑ Emergency Medical Service. ALUNA. doi:10.36740/emems. S2CID 7546377.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Takeuchi, Asia; Ahern, Terence L.; Henderson, Sean O. (February 2011). "Excited Delirium". Western Journal of Emergency Medicine. 12 (1): 77–83. ISSN 1936-900X. PMC 3088378. PMID 21691475.
- 1 2 3 4 Wetli, Charles V.; Fishbain, David A. (1985-07-01). "Cocaine-Induced Psychosis and Sudden Death in Recreational Cocaine Users". Journal of Forensic Sciences. 30 (3): 873–880. doi:10.1520/jfs11020j. ISSN 0022-1198. PMID 4031813.
- 1 2 Ruttenber, A. James; Lawler-Heavner, Janet; Yin, Ming; Wetli, Charles V.; Hearn, W. Lee; Mash, Deborah C. (1997-01-01). "Fatal Excited Delirium Following Cocaine Use: Epidemiologic Findings Provide New Evidence for Mechanisms of Cocaine Toxicity". Journal of Forensic Sciences. 42 (1): 25–31. doi:10.1520/jfs14064j. ISSN 0022-1198. PMID 8988571.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 Mash, Deborah C. (2016). "Excited Delirium and Sudden Death: A Syndromal Disorder at the Extreme End of the Neuropsychiatric Continuum". Frontiers in Physiology. 7: 435. doi:10.3389/fphys.2016.00435. ISSN 1664-042X. PMC 5061757. PMID 27790150.
- 1 2 Lee, Bo-Shyan; Huang, Si-Sheng; Hsu, Wen-Yu; Chiu, Nan-Ying (2012-06-21). "Clinical features of delirious mania: a series of five cases and a brief literature review". BMC Psychiatry. 12: 65. doi:10.1186/1471-244X-12-65. ISSN 1471-244X. PMC 3503657. PMID 22716018.
- 1 2 3 JACOBOWSKI, NATALIE L.; HECKERS, STEPHAN; BOBO, WILLIAM V. (January 2013). "Delirious Mania". Journal of Psychiatric Practice. 19 (1): 15–28. doi:10.1097/01.pra.0000426324.67322.06. ISSN 1538-1145. PMID 23334676. S2CID 10286031.
- ↑ Wetli, C.V. (2005), "Excited Delirium", Encyclopedia of Forensic and Legal Medicine, Elsevier, pp. 276–281, doi:10.1016/b0-12-369399-3/00311-6, ISBN 978-0-12-369399-0, retrieved 2021-04-01
- 1 2 3 Karmacharya, Rakesh; England, Mary Lou; Öngür, Dost (2008-08-01). "Delirious mania: Clinical features and treatment response". Journal of Affective Disorders. 109 (3): 312–316. doi:10.1016/j.jad.2007.12.001. ISSN 0165-0327. PMID 18191210.
- 1 2 3 4 Cordeiro, Catarina R.; Saraiva, Rodrigo; Côrte-Real, Beatriz; Pestana, Pedro Câmara; Andrade, Gabriela; Fernandes, Elsa; Castanheira, LÃ-gia; Martins, and Paulo (2020-04-09). "When the Bell Rings". The Primary Care Companion for CNS Disorders. 22 (2). doi:10.4088/PCC.19l02511. PMID 32286746. S2CID 215758935.
- 1 2 3 4 5 6 7 8 9 10 11 12 Fink, Max (1999). "Delirious mania". Bipolar Disorders. 1 (1): 54–60. doi:10.1034/j.1399-5618.1999.10112.x. ISSN 1399-5618. PMID 11256658.
- 1 2 Bipeta, Rajshekhar; Khan, Majeed A. (2012-11-12). "Delirious Mania: Can We Get Away with This Concept? A Case Report and Review of the Literature". Case Reports in Psychiatry. 2012: 720354. doi:10.1155/2012/720354. PMC 3502817. PMID 23198239.
- 1 2 "The Clock Drawing Test", Quick Cognitive Screening for Clinicians, Abingdon, UK: Taylor & Francis, 2003, doi:10.4324/9780203427170_chapter_4, ISBN 978-0-203-44696-6, retrieved 2021-04-01
- ↑ Patten, S. B.; Lamarre, C. J. (November 1989). "The face-hand test: a useful addition to the psychiatric physical examination". Psychiatric Journal of the University of Ottawa. 14 (4): 554–556. ISSN 0702-8466. PMID 2813636.
- 1 2 KAHN, ROBERT L.; POLLACK, MAX; FINK, MAX (1960-05-01). "Figure-Ground Discrimination After Induced Altered Brain Function". Archives of Neurology. 2 (5): 547–551. doi:10.1001/archneur.1960.03840110061007. ISSN 0375-8540. PMID 14404003.
- ↑ Cipriani, Andrea; Barbui, Corrado; Salanti, Georgia; Rendell, Jennifer; Brown, Rachel; Stockton, Sarah; Purgato, Marianna; Spineli, Loukia M; Goodwin, Guy M; Geddes, John R (October 2011). "Comparative efficacy and acceptability of antimanic drugs in acute mania: a multiple-treatments meta-analysis". The Lancet. 378 (9799): 1306–1315. doi:10.1016/S0140-6736(11)60873-8. PMID 21851976. S2CID 25512763.
- ↑ Ashok, A. H.; Marques, T. R.; Jauhar, S.; Nour, M. M.; Goodwin, G. M.; Young, A. H.; Howes, O. D. (May 2017). "The dopamine hypothesis of bipolar affective disorder: the state of the art and implications for treatment". Molecular Psychiatry. 22 (5): 666–679. doi:10.1038/mp.2017.16. ISSN 1476-5578. PMC 5401767. PMID 28289283.
- ↑ Silverstone, Trevor; Wells, Brian; Trenchard, Esther (February 1983). "Differential dose-response effects of dexamphetamine sulphate on hunger, arousal and mood in human volunteers". Psychopharmacology. 79 (2–3): 242–245. doi:10.1007/BF00427820. ISSN 0033-3158. PMID 6405435. S2CID 22272809.
- ↑ Kalivas, PW; Duffy, P (1993-01-01). "Time course of extracellular dopamine and behavioral sensitization to cocaine. I. Dopamine axon terminals". The Journal of Neuroscience. 13 (1): 266–275. doi:10.1523/jneurosci.13-01-00266.1993. ISSN 0270-6474. PMC 6576317. PMID 8423473.
- ↑ Penders, Thomas M.; Gestring, Richard E.; Vilensky, Dmitry A. (November 2012). "Intoxication Delirium following Use of Synthetic Cathinone Derivatives". The American Journal of Drug and Alcohol Abuse. 38 (6): 616–617. doi:10.3109/00952990.2012.694535. ISSN 0095-2990. PMID 22783894. S2CID 207428569.
- ↑ Mann, S. C.; Boger, W. P. (September 1978). "Psychotropic drugs, summer heat and humidity, and hyperpyrexia: a danger restated". American Journal of Psychiatry. 135 (9): 1097–1100. doi:10.1176/ajp.135.9.1097. ISSN 0002-953X. PMID 29501.
- ↑ Vilke, Gary M.; DeBard, Mark L.; Chan, Theodore C.; Ho, Jeffrey D.; Dawes, Donald M.; Hall, Christine; Curtis, Michael D.; Costello, Melissa Wysong; Mash, Deborah C.; Coffman, Stewart R.; McMullen, Mary Jo (November 2012). "Excited Delirium Syndrome (ExDS): Defining Based on a Review of the Literature". The Journal of Emergency Medicine. 43 (5): 897–905. doi:10.1016/j.jemermed.2011.02.017. PMID 21440403.
- ↑ Richter, Diethelm W.; Mironov, Sergej L.; Büsselberg, Dietrich; Lalley, Peter M.; Bischoff, Anne M.; Wilken, Bernd (June 2000). "Respiratory Rhythm Generation: Plasticity of a Neuronal Network". The Neuroscientist. 6 (3): 181–198. doi:10.1177/107385840000600309. ISSN 1073-8584. S2CID 85237863.
- ↑ Seitz, Dallas P.; Gill, Sudeep S.; van Zyl, Louis T. (2007-01-15). "Antipsychotics in the Treatment of Delirium". The Journal of Clinical Psychiatry. 68 (1): 11–21. doi:10.4088/jcp.v68n0102. ISSN 0160-6689. PMID 17284125.
- ↑ Bieniek, Sherrie A.; Ownby, Raymond L.; Penalver, Alberto; Dominguez, Roberto A. (1998-01-02). "A Double-Blind Study of Lorazepam versus the Combination of Haloperidol and Lorazepam in Managing Agitation". Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 18 (1): 57–62. doi:10.1002/j.1875-9114.1998.tb03827.x. ISSN 0277-0008. PMID 9469682. S2CID 24505811.
- ↑ Battaglia, John; Moss, Sue; Rush, John; Kang, Jasbir; Mendoza, Ricardo; Leedom, Liane; Dubin, William; McGlynn, Charles; Goodman, Lowell (July 1997). "Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study". The American Journal of Emergency Medicine. 15 (4): 335–340. doi:10.1016/s0735-6757(97)90119-4. ISSN 0735-6757. PMID 9217519.
- ↑ Green, Steven M; Rothrock, Steven G; Lynch, Elizabeth L; Ho, Matthew; Harris, Troy; Hestdalen, Rodney; Hopkins, G.Alan; Garrett, Wayne; Westcott, Kelli (June 1998). "Intramuscular Ketamine for Pediatric Sedation in the Emergency Department: Safety Profile in 1,022 Cases". Annals of Emergency Medicine. 31 (6): 688–697. doi:10.1016/s0196-0644(98)70226-4. ISSN 0196-0644. PMID 9624307.
- ↑ Strayer, Reuben J.; Nelson, Lewis S. (November 2008). "Adverse events associated with ketamine for procedural sedation in adults". The American Journal of Emergency Medicine. 26 (9): 985–1028. doi:10.1016/j.ajem.2007.12.005. ISSN 0735-6757. PMID 19091264.
- ↑ Melamed, Eitan; Oron, Yahav; Ben-Avraham, Ron; Blumenfeld, Amir; Lin, Guy (October 2007). "The combative multitrauma patient: a protocol for prehospital management". European Journal of Emergency Medicine. 14 (5): 265–268. doi:10.1097/mej.0b013e32823a3c9b. ISSN 0969-9546. PMID 17823561. S2CID 1197543.
- ↑ "Neuroleptic Malignant Syndrome: A Rare, Dangerous Effect of Antipsychotic Drugs". WebMD. Retrieved 2021-04-10.
- ↑ Allam, S.; Noble, J. S. (April 2001). "Cocaine-excited delirium and severe acidosis". Anaesthesia. 56 (4): 385–386. doi:10.1046/j.1365-2044.2001.01976-24.x. ISSN 0003-2409. PMID 11284850. S2CID 35080299.
- ↑ "The Crack Epidemic - The History of Crack Cocaine - Drug-Free World". Foundation for a Drug-Free World. Retrieved 2021-05-24.
- ↑ Stratton, Samuel J.; Rogers, Christopher; Brickett, Karen; Gruzinski, Ginger (May 2001). "Factors associated with sudden death of individuals requiring restraint for excited delirium". The American Journal of Emergency Medicine. 19 (3): 187–191. doi:10.1053/ajem.2001.22665. ISSN 0735-6757. PMID 11326341.
- ↑ Stauder, K. H. (December 1934). "Die tödliche Katatonie". Archiv für Psychiatrie und Nervenkrankheiten. 102 (1): 614–634. doi:10.1007/bf01813829. ISSN 0003-9373. S2CID 38213417.
- ↑ Pollanen, Michael S; Smith, Charles R; Chiasson, David A; Cairns, James T; Young, James (April 2002). "Fatal child abuse-maltreatment syndrome". Forensic Science International. 126 (2): 101–104. doi:10.1016/s0379-0738(02)00008-7. ISSN 0379-0738. PMID 12084484.
- ↑ Fishbain, David A.; Wetli, Charles V. (October 1981). "Cocaine intoxication, delirium, and death in a body packer". Annals of Emergency Medicine. 10 (10): 531–532. doi:10.1016/s0196-0644(81)80010-8. ISSN 0196-0644. PMID 7283219.
- 1 2 3 Wetli, Charles V. (March 1987). "Fatal Cocaine Intoxication". The American Journal of Forensic Medicine and Pathology. 8 (1): 1–2. doi:10.1097/00000433-198703000-00001. ISSN 0195-7910. PMID 3578198.
- ↑ Wetli, Charles V.; Fishbain, David A. (1985-07-01). "Cocaine-Induced Psychosis and Sudden Death in Recreational Cocaine Users". Journal of Forensic Sciences. 30 (3): 873–880. doi:10.1520/JFS11020J. PMID 4031813.
Further reading
- Bell, Luther V. (October 1849). "On a Form of Disease resembling some advanced stages of mania and fever, but so contradistinguished from any ordinarily observed or described combination of symptoms, as to render it probable that it may be an overlooked and hitherto unrecorded malady: by Luther V. Bell, M. D., Physician and Superintendent of the McLean Asylum for the Insane, Somerville, Mass". American Journal of Psychiatry. 6 (2): 97–127. doi:10.1176/ajp.6.2.97. ISSN 0002-953X.