Ovarian tissue cryopreservation is cryopreservation of tissue of the ovary of a female.
Indications
Cryopreservation of ovarian tissue is of interest to women who want fertility preservation beyond the natural limit, or whose reproductive potential is threatened by cancer therapy,[1] for example in hematologic malignancies or breast cancer.[2] It can be performed on prepubertal girls at risk for premature ovarian failure, and this procedure is as feasible and safe as comparable operative procedures in children.[3]
Procedure
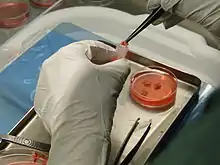

The procedure is to take a part of the ovary and carry out slow freezing before storing it in liquid nitrogen whilst therapy is undertaken. Tissue can then be thawed and implanted near the fallopian, either orthotopic (on the natural location) or heterotopic (on the abdominal wall),[2] where it starts to produce new eggs, allowing normal conception to take place.[4] A study of 60 procedures concluded that ovarian tissue harvesting appears to be safe.[2] A study has also concluded that culturing a thawed fetal ovarian tissue for a few days before transplanting can be beneficial to the development of follicles.[5]
Strips of cortical ovarian tissue can also be cryopreserved, but it must be re-implanted into the body to allow the encapsulated immature follicles to complete their maturation. In vitro maturation has been performed experimentally, but the technique is not yet clinically available.[6] With this technique, cryopreserved ovarian tissue could possibly be used to make oocytes that can directly undergo in vitro fertilization.[6]
Potential for Pregnancy
Women with malignant diseases that undergo treatment utilizing irradiation or gonadotoxic drugs, have an increase probability of losing ovarian function resulting in infertility. The ovarian cortical tissue harbors majority of the ovarian pool of follicles. Once a patient is cured from their malignant disease, the tissue can be thawed and then transplanted for the possibility of restoring ovarian function. Following auto-transplantation, patients showed resumption of ovarian activity to include the first menstruation at 14 to 25 weeks, and follicular development 8 to 21 weeks.[7]
Risk of cancer recurrence
For autotransplantation of cryopreserved ovarian tissue in cancer survivors, metastases have been repeatedly detected in ovarian tissue obtained from patients with leukemia, as well as in one patient with Ewing sarcoma.[8] Ovarian tissue autotransplantation may pose a risk of cancer recurrence in patients with colorectal, gastric and endometrial cancer.[8] However, no metastases have been detected in ovarian tissue from lymphoma and breast cancer patients who have been undergoing ovarian tissue cryopreseration.[8]
History
The first transplant of cryopreserved ovarian tissue was performed in New York by Kutluk Oktay in 1999, but it did not restore menstrual cycles to the patient. In 2004 Jacques Donnez in Belgium reported the first successful birth from frozen tissue using a protocol developed in Roger Gosden’s laboratory, where Oktay had studied.
In 1997 samples of ovarian cortex were taken from a woman with Hodgkin's lymphoma and cryopreserved by slow freezing (Planer, UK) for banking in liquid nitrogen. The patient had premature ovarian failure after chemotherapy. In 2003, after freeze-thawing, orthotopic autotransplantation of ovarian cortical tissue was done by laparoscopy and five months after reimplantation regular ovulatory cycles were reinitiated. Eleven months after re-implantation a viable intrauterine pregnancy was confirmed, which resulted in the delivery of a healthy baby. Donnez’s claims have been challenged because there was no absolute proof if the mother was infertile before treatment.[9] However, Sherman Silber in St. Louis, Missouri, and another of Gosden’s collaborators, Dror Meirow at the Sheba Medical Center in Israel, and subsequently others have proven beyond doubt the technique is effective. Healthy babies of both genders have been born.
The first birth following transplantation of ovarian tissue stored at a central cryo bank and transported overnight has been achieved by centers of the Fertiprotekt network in Germany 2011. This demonstrated that ovarian tissue can be stored centrally in specialized centers.[10][11]
References
- ↑ Isachenko V, Lapidus I, Isachenko E, et al. (2009). "Human ovarian tissue vitrification versus conventional freezing: morphological, endocrinological, and molecular biological evaluation". Reproduction. 138 (2): 319–27. doi:10.1530/REP-09-0039. PMID 19439559.
- 1 2 3 Oktay K, Oktem O (November 2008). "Ovarian cryopreservation and transplantation for fertility preservation for medical indications: report of an ongoing experience". Fertil. Steril. 93 (3): 762–8. doi:10.1016/j.fertnstert.2008.10.006. PMID 19013568.
- ↑ Jadoul, P.; Dolmans, M. -M.; Donnez, J. (2010). "Fertility preservation in girls during childhood: is it feasible, efficient and safe and to whom should it be proposed?". Human Reproduction Update. 16 (6): 617–30. doi:10.1093/humupd/dmq010. PMID 20462941.
- ↑ Livebirth after orthotopic transplantation of cryopreserved ovarian tissue The Lancet, Sep 24, 2004
- ↑ Lan C, Xiao W, Xiao-Hui D, Chun-Yan H, Hong-Ling Y (December 2008). "Tissue culture before transplantation of frozen-thawed human fetal ovarian tissue into immunodeficient mice". Fertil. Steril. 93 (3): 913–9. doi:10.1016/j.fertnstert.2008.10.020. PMID 19108826.
- 1 2 McLaughlin, M; Albertini, D F; Wallace, W H B; Anderson, R A; Telfer, E E (2018). "Metaphase II oocytes from human unilaminar follicles grown in a multi-step culture system" (PDF). MHR: Basic Science of Reproductive Medicine. 24 (3): 135–142. doi:10.1093/molehr/gay002. ISSN 1360-9947. PMID 29390119.
Further comments in BBC News article: James Gallagher (2018-02-09). "First human eggs grown in laboratory". BBC News. - ↑ Andersen, C. Y., et al. "Two Successful Pregnancies Following Autotransplantation of Frozen/Thawed Ovarian Tissue." Human Reproduction, vol. 23, no. 10, August 2008, pp. 2266–2272. Oxford Academy , doi:10.1093/humrep/den244
- 1 2 3 Bastings, L.; Beerendonk, C. C. M.; Westphal, J. R.; Massuger, L. F. A. G.; Kaal, S. E. J.; Van Leeuwen, F. E.; Braat, D. D. M.; Peek, R. (2013). "Autotransplantation of cryopreserved ovarian tissue in cancer survivors and the risk of reintroducing malignancy: A systematic review". Human Reproduction Update. 19 (5): 483–506. doi:10.1093/humupd/dmt020. PMID 23817363. S2CID 8855950.
- ↑ "Ovarian transplant update: Authors of 2004 live-birth follow-up letter ask Lancet to retract it". 2012-07-26.
- ↑ Ralf Dittrich, Laura Lotz, Gudrun Keck, Inge Hoffmann, Andreas Mueller, Matthias W. Beckmann, Hans van der Ven, Markus Montag: Live birth after ovarian tissue autotransplantation following overnight transportation before cryopreservation. Fertil Steril. 97 (2012), S. 387-90, doi:10.1016/j.fertnstert.2011.11.047.
- ↑ Andreas Müller, Katja Keller, Jennifer Wacker, Ralf Dittrich, Gudrun Keck, Markus Montag, Hans van der Ven, David Wachter, Matthias W. Beckmann, Wolfgang Distler: Retransplantation of Cryopreserved Ovarian Tissue: the First Live Birth in Germany. Dtsch Ärztebl Int 109 (2012), S. 8-13, doi:10.3238/arztebl.2012.0008.