| Pancreatic duct | |
|---|---|
 The pancreatic duct | |
 | |
| Details | |
| Precursor | Pancreatic bud |
| Identifiers | |
| Latin | ductus pancreaticus |
| MeSH | D010183 |
| TA98 | A05.9.01.015 |
| TA2 | 3129 |
| FMA | 10419 |
| Anatomical terminology | |
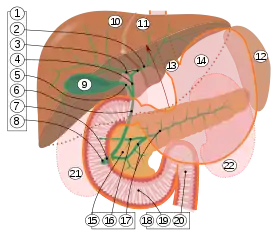
9. Gallbladder.
10–11. Right and left lobes of liver.
12. Spleen.
13. Esophagus.
14. Stomach.
15. Pancreas: 16. Accessory pancreatic duct, 17. Pancreatic duct.
18. Small intestine: 19. Duodenum, 20. Jejunum
21–22. Right and left kidneys.
The front border of the liver has been lifted up (brown arrow).[1]
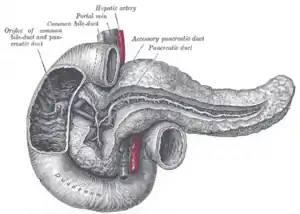
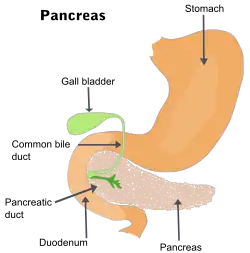
The pancreatic duct, or duct of Wirsung (also, the major pancreatic duct due to the existence of an accessory pancreatic duct), is a duct joining the pancreas to the common bile duct. This supplies it with pancreatic juice from the exocrine pancreas, which aids in digestion.
Structure
The pancreatic duct joins the common bile duct just prior to the ampulla of Vater, after which both ducts perforate the medial side of the second portion of the duodenum at the major duodenal papilla. There are many anatomical variants reported, but these are quite rare.[2]
Accessory pancreatic duct
Most people have just one pancreatic duct. However, some have an additional accessory pancreatic duct, also called the Duct of Santorini. An accessory pancreatic duct can be functional or non-functional.[3][4] It may open separately into the second part of the duodenum,[3][4] which is dorsal, and usually (in 70% of people) drains into the duodenum via the minor duodenal papilla. In the other 30% of people, it drains into the main pancreatic duct, which drains into the duodenum via the major duodenal papilla. The main pancreatic duct and the accessory duct both eventually—either directly or indirectly—connect to the second part ('D2', the vertical segment) of the duodenum.
It is named for Giovanni Domenico Santorini.[5][6]
 Formation of an accessory pancreatic duct
Formation of an accessory pancreatic duct
Clinical significance
Compression, obstruction or inflammation of the pancreatic duct may lead to acute pancreatitis. The most common cause for obstruction is the presence of gallstones in the common bile duct, a condition called choledocholithiasis. Obstruction can also be due to duodenal inflammation in Crohn's disease.[7] A gallstone may get lodged in the constricted distal end of the ampulla of Vater, where it blocks the flow of both bile and pancreatic juice into the duodenum. Bile backing up into the pancreatic duct may initiate pancreatitis.[8] The pancreatic duct is generally regarded as abnormally enlarged if being over 3 mm in the head and 2 mm in the body or tail on CT scan.[9] Pancreatic duct or parts of pancreatic duct can be demonstrated on ultrasound in 75 to 85% of people.[10]
Pancreatic ductal carcinoma is a common form of pancreatic cancer.
History
The pancreatic duct is also called the duct of Wirsung.[11] This is named after its discoverer, the German anatomist Johann Georg Wirsung (1589–1643).[12]
Additional images
 ERCP image showing the pancreatic duct and biliary tree.
ERCP image showing the pancreatic duct and biliary tree. Accessory digestive system.
Accessory digestive system.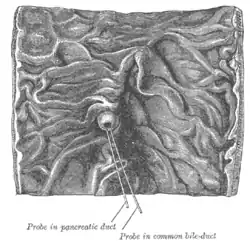 Interior of the descending portion of the duodenum, showing bile papilla.
Interior of the descending portion of the duodenum, showing bile papilla. Pancreas of a human embryo of five weeks.
Pancreas of a human embryo of five weeks. Pancreas of a human embryo at end of sixth week.
Pancreas of a human embryo at end of sixth week. Pancreatic duct Deep dissection.Anterior view.
Pancreatic duct Deep dissection.Anterior view. Ultrasonography of a dilated pancreatic duct (in this case 9mm) due to pancreatic cancer.
Ultrasonography of a dilated pancreatic duct (in this case 9mm) due to pancreatic cancer.
References
- ↑ Standring S, Borley NR, eds. (2008). Gray's anatomy : the anatomical basis of clinical practice. Brown JL, Moore LA (40th ed.). London: Churchill Livingstone. pp. 1163, 1177, 1185–6. ISBN 978-0-8089-2371-8.
- ↑ Goel, Shivi; Rustagi, SM; Saha, S; Mehta, V; Suri, RK; Rath, G (July 2015). "Aberrant pancreatic ductal organisation: a case report". Surgical and Radiologic Anatomy. 37 (5): 543–6. doi:10.1007/s00276-015-1474-z. PMID 25840941. S2CID 6917153.
- 1 2 Moore KL, Dalley AF. 2006. Clinically Oriented Anatomy. 5th Ed. Lippincott Williams & Wilkins. p 287.
- 1 2 1. Mchonde GJ, Gesase AP. Termination pattern of main and accessory pancreatic ducts among Tanzanians. Anatomy Journal of Africa. 2014; 3(1):223–227.
- ↑ synd/3087 at Who Named It?
- ↑ G. D. Santorini. Observationes anatomicae. Venetiis, apus J. B. Recurti, 1724
- ↑ "American Gastroenterological Association". Archived from the original on 2008-06-07. Retrieved 2010-03-15.
- ↑ Moore, Keith L.; Dalley, Arthur F. (2006). Clinically Oriented Anatomy, Fifth Edition. Lippincott Williams & Wilkins. p. 287. ISBN 0-7817-3639-0.
- ↑ Edge, Mark D (2007). "Clinical significance of main pancreatic duct dilation on computed tomography: Single and double duct dilation". World Journal of Gastroenterology. 13 (11): 1701–1705. doi:10.3748/wjg.v13.i11.1701. ISSN 1007-9327. PMC 4146949. PMID 17461473.
- ↑ Glaser, J.; Högemann, B.; Krummenerl, T.; Schneider, M.; Hultsch, E.; Van Husen, N.; Gerlach, U. (October 1987). "Sonographic imaging of the pancreatic duct: New diagnostic possibilities using secretin stimulation". Digestive Diseases and Sciences. 32 (10): 1075–1081. doi:10.1007/BF01300191. ISSN 0163-2116. PMID 3308373. S2CID 20674576.
- ↑ Eisenscher, Albert; Weill, Francis (1979). "Ultrasonic visualization of Wirsung's duct: Dream or reality?". Journal of Clinical Ultrasound. 7 (1): 41–44. doi:10.1002/jcu.1870070112. ISSN 1097-0096. PMID 108297. S2CID 21851681.
- ↑ doctor/2941 at Who Named It?