 | |
| Clinical data | |
|---|---|
| Trade names | Eumovate |
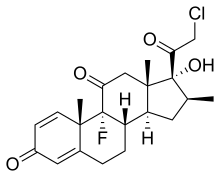
| Other names | (8S,9R,10S,13S,14S,16S,17R)-17-(2-Chloroacetyl)-9-fluoro-17-hydroxy-10,13,16-trimethyl-7,8,12,14,15,16-hexahydro-6H-cyclopenta[a]phenanthrene-3,11-dione |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Routes of administration | topical |
| ATC code | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ECHA InfoCard | 100.053.576 |
| Chemical and physical data | |
| Formula | C22H26ClFO4 |
| Molar mass | 408.89 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Clobetasone (INN[1]) is a corticosteroid used in dermatology, for treating such skin inflammation as seen in eczema, psoriasis and other forms of dermatitis, and ophthalmology. Topical clobetasone butyrate has shown minimal suppression of the hypothalamic–pituitary–adrenal axis.[2]
It is available as clobetasone butyrate under the brand names Eumosone or Eumovate[3] both manufactured by GlaxoSmithKline.
Trimovate also contains oxytetracycline, an antibiotic, and nystatin, an antifungal.[4]
Uses
In dermatology, topical clobetasone butyrate helps to reduce the itchiness and erythema associated with eczema and dermatitis.[5]
In ophthalmology, clobetasone butyrate 0.1% eye drops have been shown to be safe and effective in the treatment of dry eyes in Sjögren syndrome. Sjögren syndrome is an autoimmune disorder that affects the moisture producing glands of the body causing many symptoms including dry eyes.[6] When compared to other corticosteroid eye drops; clobetasone butyrate showed only minimal rises in intraocular pressure. Increased pressure within the eye can lead to glaucoma.[7][8][9]
Adverse effects
Side effects associated with clobetasone cream and ointment include: burning, irritation, itching, thinning of the skin, and changes in skin color.[5][10]
Contraindications
The following should not be treated with clobetasone with nystatin and oxytetracycline:
- Patients with known history of hypersensitivity to clobetasone butyrate, nystatin, oxytetracycline or any components of the formulation
- Primary cutaneous viral infections (Common viral skin infections include herpes simplex virus infection, herpes zoster, cutaneous and genital warts, and molluscum contagiosum.)[11]
- Primary infected skin lesions caused by infection with fungi, bacteria or yeasts (Fungal infections of the skin commonly seen in family practice include the various forms of tinea: tinea corporis, tinea gladiatorum, tinea cruris, tinea pedis, tinea capitis, and tinea unguium (e.g., onychomycosis).)[11]
- Cutaneous infections caused by Acinetobacter species (implicated in a number of hospital-acquired infections such as bacteremia, urinary tract infections (UTIs), secondary meningitis, infective endocarditis, and wound and burn infections.), methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas species, Proteus species Serratia species or Group B streptococcal infection (Streptococcus B., Group B streptococcal infection, also known as Group B streptococcal disease or just Group B strep, is the infection caused by the bacterium Streptococcus agalactiae (S. agalactiae) also known as group B streptococcus or GBS)
- Rosacea
- Acne vulgaris
- Pruritus without inflammation
Serious Contraindications
- Pseudomembranous colitis - C. Diff. Colitis, also called: clostridium difficile colitis, or Pseudomembranous colitis has been reported with the use of antibiotics and may range in severity from mild to life-threatening.
- Reversible hypothalamic-pituitary-adrenal (HPA) axis suppression - Manifestations of hypercortisolism (Cushing's syndrome) and reversible hypothalamic-pituitary-adrenal (HPA) axis suppression can occur in some individuals as a result of increased systemic absorption of topical corticosteroids. (The hypothalamic–pituitary–adrenal (HPA) axis is the complex relationship between the hypothalamus, the pituitary gland, and the adrenals; was previously called Adrenal Fatigue.)[12]
See also
References
- ↑ "United Nations Statistics Division - Classifications Registry - Alphabetical index for HS 2002 Entries starting with 'C' (page 310 of 422)". Archived from the original on 2011-06-08. Retrieved 2007-12-11.
- ↑ Munro DD, Wilson L (September 1975). "Clobetasone butyrate, a new topical corticosteroid: clinical activity and effects on pituitary-adrenal axis function and model of epidermal atrophy". British Medical Journal. 3 (5984): 626–8. doi:10.1136/bmj.3.5984.626. PMC 1674413. PMID 1164639.
- ↑ "Eumovate cream/ointment". NetDoctor.co.uk. 2017-07-05.
- ↑ "Trimovate". Electronic Medicines Compendium (EMC). Datapharm Ltd.
- 1 2 "Euvomate Medication Guide". GlaxoSmithKline. Archived from the original on 30 January 2014.
- ↑ Aragona P, Spinella R, Rania L, Postorino E, Sommario MS, Roszkowska AM, Puzzolo D (2013). "Safety and efficacy of 0.1% clobetasone butyrate eyedrops in the treatment of dry eye in Sjögren syndrome". European Journal of Ophthalmology. 23 (3): 368–76. doi:10.5301/ejo.5000229. PMID 23225089. S2CID 20730843.
- ↑ Ramsell TG, Bartholomew RS, Walker SR (January 1980). "Clinical evaluation of clobetasone butyrate: a comparative study of its effects in postoperative inflammation and on intraocular pressure". The British Journal of Ophthalmology. 64 (1): 43–5. doi:10.1136/bjo.64.1.43. PMC 1039346. PMID 6986899.
- ↑ Wilhelmus KR, Hunter PA, Rice NS (October 1981). "Equivalence of topical clobetasone and dexamethasone in experimental corneal allograft rejection". The British Journal of Ophthalmology. 65 (10): 699–701. doi:10.1136/bjo.65.10.699. PMC 1039641. PMID 7032579.
- ↑ Eilon LA, Walker SR (September 1981). "Clinical evaluation of clobetasone butyrate eye drops in the treatment of anterior uveitis and its effects on intraocular pressure". The British Journal of Ophthalmology. 65 (9): 644–7. doi:10.1136/bjo.65.9.644. PMC 1039614. PMID 7028089.
- ↑ "Clobetason Butyrate". WebMD. Archived from the original on March 2, 2012.
- 1 2 Woolever, Donald Raj (February 7, 2020). "Skin Infections and Outpatient Burn Management: Fungal and Viral Skin Infections". FP Essentials. 489: 16–20. PMID 31995350 – via PubMed.
- ↑ "Overcoming HPA Axis Suppression (Formerly Known as Adrenal Fatigue)". BodyLogicMD. October 23, 2017.