| Microphthalmia | |
|---|---|
 | |
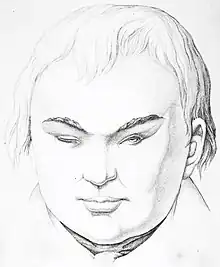
| Right unilateral microphthalmia | |
| Specialty | Medical genetics |
| Symptoms | Abnormally small eyeball(s) |
| Usual onset | Birth[1] |
| Duration | Lifelong[1] |
| Causes | Genetic or environmental factors[1] |
| Frequency | 1 in 10,000 individuals[1] |
Microphthalmia (Greek: μικρός, mikros, 'small', ὀφθαλμός, ophthalmos, 'eye'), also referred as microphthalmos, is a developmental disorder of the eye in which one (unilateral microphthalmia) or both (bilateral microphthalmia) eyes are abnormally small and have anatomic malformations. Microphthalmia is a distinct condition from anophthalmia and nanophthalmia. Although sometimes referred to as 'simple microphthalmia', nanophthalmia is a condition in which the size of the eye is small but no anatomical alterations are present.[2][3]
Presentation
.jpg.webp)
Microphthalmia is a congenital disorder in which the globe of the eye is unusually small and structurally disorganized.[2][4] While the axis of an adult human eye has an average length of about 23.8 mm (0.94 in), a diagnosis of microphthalmia generally corresponds to an axial length below 21 mm (0.83 in) in adults.[3][5] Additionally, the diameter of the cornea is about 9–10.5 mm (0.35–0.41 in) in affected newborns and 10.5–12 mm (0.41–0.47 in) in adults with the condition.[3] The presence of a small eye within the orbit can be a normal incidental finding but in many cases it is atypical and results in visual impairment. The prevalence of this condition is around 1 in 10,000 births, and it affects roughly 3–11% of blind children.[3][1][6]
Causes
It has been postulated that microphthalmia arises as a result of interference with postnatal eye growth, in contrast to anophthalmia which originates much earlier during fetal development. Genetic causes of microphthalmia include chromosomal abnormalities (e.g. Patau syndrome, mosaic trisomy 9, 13q deletion syndrome, Wolf–Hirschhorn syndrome) or monogenetic Mendelian disorders (e.g. CHARGE syndrome, Fraser syndrome, oculofaciocardiodental syndrome, Lenz microphthalmia syndrome).[3][7] Microphthalmia in newborns is sometimes associated with fetal alcohol spectrum disorder[2] or infections during pregnancy, particularly herpes simplex virus, rubella and cytomegalovirus (CMV), but the evidence is inconclusive.[3]
The following genes, many of which are transcription and regulatory factors, have been implicated in microphthalmia, anophthalmia, and coloboma:[8][9][10]
- ABCB6
- ACTB
- ACTG1
- ALDH1A3
- ATOH7
- BCOR
- BMP4
- BMP7
- C12orf57
- CC2D2A
- CHD7
- CLDN19
- COX7B
- CRIM1
- CRYAA
- CRYBA4
- CRYBB2
- DHX38
- DPYD
- ERCC1
- ERCC5
- FADD
- FAM111A
- FNBP4
- FOXL2
- FRAS1
- FREM1
- FREM2
- FZD5
- GDF3
- GDF6
- GJA1
- GRIP1
- HCCS
- HMGB3
- HMX1
- IGBP1
- KAT6B
- KMT2D
- LRP2
- MAB21L2
- MAF
- MFRP
- NAA10
- NDUFB11
- NHS
- OTX2
- PAX2
- PAX6
- PDE6D
- PIGL
- POLR1C
- POLR1D
- PORCN
- PQBP1
- PRSS56
- PTCH1
- RAB3GAP1
- RAB3GAP2
- RARB
- RAX
- RBP4
- RPGRIP1L
- SALL1
- SALL2
- SALL4
- SCLT1
- SEMA3E
- SHH
- SIX3
- SIX6
- SMOC1
- SNX3
- SOX2
- SRD5A3
- STRA6
- TBC1D20
- TBC1D32
- TBX22
- TCOF1
- TENM3
- TFAP2A
- TMEM98
- TMEM67
- TMX3
- VAX1
- VSX2
- YAP1
- ZEB2
- ZIC2
SOX2 has been implicated in a substantial number (10–15%) of cases and in many other cases failure to develop the ocular lens often results in microphthalmia.[3]
Microphthalmia-associated transcription factor (MITF), located on chromosome 14q32, is associated with one form of isolated microphthalmia (MCOP1). In mammals, the failure of expression of MITF in the retinal pigment epithelium prevents this structure from fully differentiating, causing a malformation of the choroid fissure of the eye and drainage of vitreous body fluid. Without this fluid, the eye fails to enlarge, resulting in microphthalmia. Waardenburg syndrome type 2 in humans may also be caused by mutations in MITF[11] The human MITF gene is homologous to the mouse microphthalmia gene (gene symbol mi); mouse with mutations in this gene are hypopigmented in their fur. The identification of the genetics of WS type 2 owes a lot to observations of phenotypes of MITF-mutant mice.[11]
Diagnosis

Microphthalmia is often diagnosed soon after birth. An initial diagnosis usually occurs after the eyes are inspected through the lids.[3] In addition to visual examinations, measurements of the cornea are used in the diagnosis of this condition.[3] An ultrasound may also be conducted to confirm whether the axial length of the eye is clinically below average (i.e. at least 2 standard deviations below the age-adjusted mean).[3][5]
When a case of microphthalmia is detected, the patient should visit an eye specialist as soon as possible. It is important for an ophthalmologist to conduct a thorough examination within 2 weeks after birth.[13] The ophthalmologist will confirm the preliminary diagnosis and look for signs of other anomalies in both eyes. These abnormalities may include coloboma, optic nerve hypoplasia, retinal dystrophy, and cataract.[13] Ultrasound may also be used to determine the presence of any internal eye issues, which may not otherwise be visible.[13] It is possible for individuals with microphthalmia to have some vision in the affected eye(s). For this reason, the vision of infants with microphthalmia should be evaluated early on, even in severe cases.[13] Pediatric vision tests along with electrodiagnostics are typically used to assess visual acuity.[13]
If no related symptoms are present, microphthalmia is defined as non-syndromic or isolated microphthalmia (MCOP). When occurring in conjunction with other developmental defects, it may be diagnosed as syndromic microphthalmia (MCOPS). Approximately 60 to 80% of microphthalmia cases are syndromic.[14] Several types of MCOPS have been recognized based on their genetic causes:
| Type | Causative gene/locus | Inheritance [lower-alpha 1] | Synonyms |
|---|---|---|---|
| MCOPS1 | NAA10[15] | XL | Lenz microphthalmia syndrome |
| MCOPS2 | BCOR[16] | XLR | |
| XLD | oculofaciocardiodental syndrome | ||
| MCOPS3 | SOX2[14] | AD | SOX2 anophthalmia syndrome, anophthalmia/microphthalmia-esophageal atresia (AEG) syndrome |
| MCOPS4 | Xq27-q28[14] | XLR | microphthalmia-ankyloblepharon-intellectual disability syndrome |
| MCOPS5 | OTX2[14] | AD | OTX2-related eye disorders |
| MCOPS6 | BMP4[17] | AD | Bakrania-Ragge syndrome, microphthalmia with brain and digit anomalies |
| MCOPS7 | HCCS, COX7B, NDUFB11[14][9] | XLD | MIDAS syndrome, microphthalmia with linear skin defects (MLS) syndrome |
| MCOPS8 | SNX3[10] | AD | microcephaly-microphthalmia ectrodactyly of lower limbs and prognathism (MMEP) syndrome, Viljoen–Smart syndrome |
| MCOPS9 | STRA6[18] | AR | anophthalmia/microphthalmia and pulmonary hypoplasia, Spear syndrome, Matthew–Wood syndrome |
| MCOPS10 | unknown[14] | microphthalmia and brain atrophy (MOBA) syndrome | |
| MCOPS11 | VAX1[14] | AR | N/A |
| MCOPS12 | RARB[14] | AD, AR | microphthalmia with or without pulmonary hypoplasia, diaphragmatic hernia, and/or cardiac defects |
| MCOPS13 | HMGB3[14] | XL | colobomatous microphthalmia with microcephaly, short stature, and psychomotor retardation, Maine microphthalmos |
| MCOPS14 | MAB21L2[14] | AD, AR | colobomatous microphthalmia-rhizomelic dysplasia syndrome, microphthalmia-coloboma-rhizomelic skeletal dysplasia |
- ↑ AD: autosomal dominant; AR: autosomal recessive; XL: X-linked; XLD: X-linked dominant; XLR: X-linked recessive
Treatment
Microphthalmia cannot be cured. However, there are treatments options to manage the condition and its associated symptoms. When the affected eye(s) display some visual function, a patient's eyesight can be improved (sometimes up to good state) by plus lenses, as a small eye is usually far-sighted.[13] When one of the eyes is unaffected, caution should be taken to guard this 'good' eye and preserve its vision. In these unilateral cases, eye glasses may be worn to offer a measure of physical protection.[3][13]
A key aspect of managing this condition is accounting for the small volume of the eye. The small orbit size characteristic of microphthalmia can impact the growth and structural development of the face after birth. As a result, microphthalmia can cause hemifacial asymmetry.[3][13] This possibility is a particular concern for individuals with unilateral cases of microphthalmia. With one eye of average size, the asymmetry often becomes much more severe as the child ages.[13] An axial length of less than 16 mm (0.63 in) indicates that a microphthalmic eye's growth will not be sufficient, and intervention will be necessary to reduce the degree of facial asymmetry.[13]
Minimizing facial asymmetry is important for cosmetic and structural reasons.[3][5][13] In order to address the size discrepancy of the affected eye(s), it is important to begin eye socket expansion early in life. The face reaches 70% of its adult size by roughly 2 years of age, and 90% of its adult size by about 5.5 years of age.[13] Additionally, the symmetry fostered by early socket expansion allows for a better prosthetic fit later in life.[5][13] Typically, an infant begins wearing a conformer, or an unpainted ocular prosthesis, in the first weeks of life.[3][5][13] The conformer is repeatedly replaced with a prothesis of a slightly larger size. This process, which takes place during the first 5 years of life, gradually enlarges the eye socket.[3][5][13] Socket expansion through the use of implants of increasing size is another effective strategy.[3][13]
After socket expansion is complete, a painted prosthetic eye can be worn for cosmetic reasons.[13] If the microphthalmic eye has functional vision, an affected individual may opt against wearing a painted prothesis. Lenses are also sometimes used for cosmetic purposes, such as a plus lens to enlarge the microphthalmic eye.[13]
Epidemiology
Microphthalmia and anophthalmia combined are estimated to occur in about 1 in 10,000 births,[19] though estimates have varied from 2 and 23 in 100,000 births. Approximately 3–11% of all blind children born globally have microphthalmia.[14]
| Study region | Category | Incidence (95% CI) | Time period |
|---|---|---|---|
| Denmark[20] | AO+MO | 1.2 | 1995–2012 |
| UK[6] | AO | 0.24 (0.13–0.40) | 1999 |
| 0.04 (0–0.13) | 2011 | ||
| MO | 1.08 (0.82–1.35) | 1999 | |
| 1.00 (0.76–1.24) | 2011 | ||
| US[21] | AO+MO | 2.08 (1.90–2.26) | 1999–2001 |
| 1.87 (1.73–2.01) | 2004–2006 | ||
| 1.91 (1.79–2.03) | 2010–2014 |
See also
- Abdominal musculature absent with microphthalmia and joint laxity
- Acorea, microphthalmia and cataract syndrome
- CHARGE syndrome
- Cross syndrome
- Fraser syndrome
- Lenz microphthalmia syndrome
- MCOPS12
- Microphthalmia–dermal aplasia–sclerocornea syndrome
- Nance–Horan syndrome
- Oculofaciocardiodental syndrome
- Patau syndrome
- Walker–Warburg syndrome
- Waardenburg syndrome
References
- 1 2 3 4 5 "Microphthalmia". MedlinePlus. US National Library of Medicine. Retrieved 2021-11-04.
- 1 2 3 "Definition of Microphthalmia". MedicineNet. Archived from the original on 2011-06-06. Retrieved 2009-01-01.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Verma AS, Fitzpatrick DR (November 2007). "Anophthalmia and microphthalmia". Orphanet Journal of Rare Diseases. 2 (1): 47. doi:10.1186/1750-1172-2-47. PMC 2246098. PMID 18039390.
- ↑ Williams AL, Bohnsack BL (June 2015). "Neural crest derivatives in ocular development: discerning the eye of the storm". Birth Defects Research. Part C, Embryo Today. 105 (2): 87–95. doi:10.1002/bdrc.21095. PMC 5262495. PMID 26043871.
- 1 2 3 4 5 6 Groot AL, Kuijten MM, Remmers J, Gilani A, Mourits DL, Kraal-Biezen E, et al. (February 2020). "Classification for treatment urgency for the microphthalmia/anophthalmia spectrum using clinical and biometrical characteristics". Acta Ophthalmologica. 98 (5): 514–520. doi:10.1111/aos.14364. PMC 7497250. PMID 32100474.
- 1 2 Dharmasena A, Keenan T, Goldacre R, Hall N, Goldacre MJ (June 2017). "Trends over time in the incidence of congenital anophthalmia, microphthalmia and orbital malformation in England: database study". The British Journal of Ophthalmology. 101 (6): 735–739. doi:10.1136/bjophthalmol-2016-308952. PMID 27601422. S2CID 27880982.
- ↑ Bardakjian, Tanya M.; Schneider, Adele (September 2011). "The genetics of anophthalmia and microphthalmia". Current Opinion in Ophthalmology. 22 (5): 309–313. doi:10.1097/ICU.0b013e328349b004. ISSN 1040-8738. PMID 21825993. S2CID 12373641.
- ↑ "Ocular Conditions Gene Panel (Oculome)" (PDF). Great Ormond Street Hospital for Children. NHS Foundation Trust. Archived (PDF) from the original on 2021-11-04. Retrieved 2021-11-04.
- 1 2 van Rahden VA, Fernandez-Vizarra E, Alawi M, Brand K, Fellmann F, Horn D; et al. (2015). "Mutations in NDUFB11, encoding a complex I component of the mitochondrial respiratory chain, cause microphthalmia with linear skin defects syndrome". Am J Hum Genet. 96 (4): 640–50. doi:10.1016/j.ajhg.2015.02.002. PMC 4385192. PMID 25772934.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 Vervoort VS, Viljoen D, Smart R, Suthers G, DuPont BR, Abbott A; et al. (2002). "Sorting nexin 3 (SNX3) is disrupted in a patient with a translocation t(6;13)(q21;q12) and microcephaly, microphthalmia, ectrodactyly, prognathism (MMEP) phenotype". J Med Genet. 39 (12): 893–9. doi:10.1136/jmg.39.12.893. PMC 1757218. PMID 12471201.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 Tassabehji, Mayada; Newton, Valeria E.; Read, Andrew P. (November 1994). "Waardenburg syndrome type 2 caused by mutations in the human microphthalmia ( MITF ) gene". Nature Genetics. 8 (3): 251–255. doi:10.1038/ng1194-251. ISSN 1546-1718. PMID 7874167. S2CID 331869.
- ↑ CDC (2019-12-05). "Facts about Anophthalmia / Microphthalmia | CDC". Centers for Disease Control and Prevention. Retrieved 2021-04-20.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Ragge, N K; Subak-Sharpe, I D; Collin, J R O (October 2007). "A practical guide to the management of anophthalmia and microphthalmia". Eye. 21 (10): 1290–1300. doi:10.1038/sj.eye.6702858. ISSN 0950-222X. PMID 17914432.
- 1 2 3 4 5 6 7 8 9 10 11 Eintracht J, Corton M, FitzPatrick D, Moosajee M (2020). "CUGC for syndromic microphthalmia including next-generation sequencing-based approaches". Eur J Hum Genet. 28 (5): 679–690. doi:10.1038/s41431-019-0565-4. PMC 7171178. PMID 31896778.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ George A, Cogliati T, Brooks BP (2020). "Genetics of syndromic ocular coloboma: CHARGE and COACH syndromes". Exp Eye Res. 193: 107940. doi:10.1016/j.exer.2020.107940. PMC 7310839. PMID 32032630.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Ng D, Thakker N, Corcoran CM, Donnai D, Perveen R, Schneider A; et al. (2004). "Oculofaciocardiodental and Lenz microphthalmia syndromes result from distinct classes of mutations in BCOR". Nat Genet. 36 (4): 411–6. doi:10.1038/ng1321. PMID 15004558. S2CID 23628891.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Blackburn PR, Zepeda-Mendoza CJ, Kruisselbrink TM, Schimmenti LA, García-Miñaur S, Palomares M; et al. (2019). "Variable expressivity of syndromic BMP4-related eye, brain, and digital anomalies: A review of the literature and description of three new cases". Eur J Hum Genet. 27 (9): 1379–1388. doi:10.1038/s41431-019-0423-4. PMC 6777538. PMID 31053785.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Casey J, Kawaguchi R, Morrissey M, Sun H, McGettigan P, Nielsen JE; et al. (2011). "First implication of STRA6 mutations in isolated anophthalmia, microphthalmia, and coloboma: a new dimension to the STRA6 phenotype". Hum Mutat. 32 (12): 1417–26. doi:10.1002/humu.21590. PMC 3918001. PMID 21901792.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Searle A, Shetty P, Melov SJ, Alahakoon TI (2018). "Prenatal diagnosis and implications of microphthalmia and anophthalmia with a review of current ultrasound guidelines: two case reports". J Med Case Rep. 12 (1): 250. doi:10.1186/s13256-018-1746-4. PMC 6114735. PMID 30153864.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Roos L, Jensen H, Grønskov K, Holst R, Tümer Z (2016). "Congenital Microphthalmia, Anophthalmia and Coloboma among Live Births in Denmark". Ophthalmic Epidemiol. 23 (5): 324–30. doi:10.1080/09286586.2016.1213859. PMID 27552085. S2CID 5101866.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ; et al. (2019). "National population-based estimates for major birth defects, 2010-2014". Birth Defects Res. 111 (18): 1420–1435. doi:10.1002/bdr2.1589. PMC 7203968. PMID 31580536.
{{cite journal}}: CS1 maint: multiple names: authors list (link)