In microbiology, the minimum inhibitory concentration (MIC) is the lowest concentration of a chemical, usually a drug, which prevents visible in vitro growth of bacteria or fungi.[1][2] MIC testing is performed in both diagnostic[1][2] and drug discovery laboratories.[3][4]
The MIC is determined by preparing a dilution series of the chemical, adding agar or broth, then inoculating with bacteria or fungi, and incubating at a suitable temperature. The value obtained is largely dependent on the susceptibility of the microorganism and the antimicrobial potency of the chemical, but other variables can affect results too.[5] The MIC is often expressed in micrograms per milliliter (μg/mL) or milligrams per liter (mg/L).
In diagnostic labs, MIC test results are used to grade the susceptibility of microbes. These grades are assigned based on agreed upon values called breakpoints. Breakpoints are published by standards development organizations such as the U.S. Clinical and Laboratory Standards Institute (CLSI), the British Society for Antimicrobial Chemotherapy (BSAC) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST).[6][7][8] The purpose of measuring MICs and grading microbes is to enable physicians to prescribe the most appropriate antimicrobial treatment.
The first step in drug discovery is often measurement of the MICs of biological extracts, isolated compounds or large chemical libraries against bacteria and fungi of interest.[9][10] MIC values provide a quantitative measure of an extract or compound’s antimicrobial potency. The lower the MIC, the more potent the antimicrobial.[4] When in vitro toxicity data is available, MICs can also be used to calculate selectivity index values, a measure of off-target to target toxicity.[4]
History
After the discovery and commercialization of antibiotics, microbiologist, pharmacologist, and physician Alexander Fleming developed the broth dilution technique using the turbidity of the broth for assessment.[11] This is commonly believed to be the conception point of minimum inhibitory concentrations.[12] Later in the 1980s, the Clinical and Laboratory Standards Institute consolidated the methods and standards for MIC determination and clinical usage. Because pathogens continue to evolve, and new drugs continue to be developed, the CLSI’s MIC protocols are periodically updated to reflect these changes.[13] The protocols and parameters set by the CLSI are considered to be the "gold standard" in the United States and are used by regulatory authorities, such as the FDA, to make evaluations.[14]
Clinical usage
Nowadays, the MIC is used in antimicrobial susceptibility testing. The MIC is reported by providing the susceptibility interpretation next to each antibiotic. The different susceptibility interpretations are: "S" (susceptible or responding to a standard dosing regimen), "I" (intermediate or requiring increased exposure), and "R" (resistant). These interpretations were developed by the CLSI and EUCAST.[6][8] There have been major discrepancies between the breakpoints from various European countries over the years, and between those from the CLSI and EUCAST.[15]
In clinics, more often than not, exact pathogens cannot be easily determined by symptoms of the patient. Then, even if the pathogen is determined, different strains of pathogens, such as Staphylococcus aureus, have varying levels of resistance to antimicrobials. As such, it is difficult to prescribe correct antimicrobials.[16] The MIC is determined in such cases by growing the pathogen isolate from the patient on plate or broth, which is later used in the assay.[17] Thus, knowledge of the MIC will provide a physician valuable information for making a prescription.
Accurate and precise usage of antimicrobials is also important in the context of multidrug-resistant bacteria. Microbes such as bacteria have been gaining resistance to antimicrobials they were previously susceptible to.[18] Usage of incompatible levels of antimicrobials provides the selective pressure that has driven the direction and evolution of resistance of bacterial pathogens.[19] This has been seen at sub-MIC levels of antibiotics.[20] As such, it is increasingly important to determine the MIC in order to make the best choice in prescribing antimicrobials.
Methods
Broth dilution assay
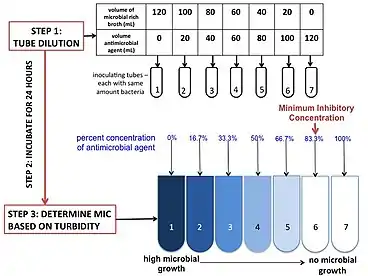
There are three main reagents necessary to run this assay: the media, an antimicrobial agent, and the microbe being tested. The most commonly used media is cation-adjusted Mueller Hinton Broth, due to its ability to support the growth of most pathogens and its lack of inhibitors towards common antibiotics.[21] Depending on the pathogen and antibiotics being tested, the media can be changed and/or adjusted. The antimicrobial concentration is adjusted into the correct concentration by mixing stock antimicrobial with media. The adjusted antimicrobial is serially diluted into multiple tubes (or wells) to obtain a gradient. The dilution rate can be adjusted depending on the breakpoint and the practitioner's needs. The microbe, or the inoculating agent, must come from the same colony-forming unit, and must be at the correct concentration. This may be adjusted by incubation time and dilution. For verification, the positive control is plated in a hundred fold dilution to count colony forming units. The microbes inoculate the tubes (or plate) and are incubated for 16–20 hours. The MIC is generally determined by turbidity.[21]
Etest

Etests can be used as an alternative method to determine the minimum inhibitory concentrations of a wide range of antimicrobial agents against different organisms. They have been widely used in microbiology laboratories around the world. Manufactured by bioMérieux, Etests are a ready-to-use, non-porous plastic reagent strip with a predefined gradient of antibiotic, covering a continuous concentration range.[22]
MBC testing
While the MIC is the lowest concentration of an antibacterial or antifungal agent necessary to inhibit visible growth, the minimum bactericidal concentration (MBC) is the minimum concentration of an antibacterial agent that results in bacterial death. It is defined by the inability to re-culture bacteria, and the closer the MIC is to the MBC, the more bactericidal the compound.[23]
MIC is used clinically over MBC because MIC is more easily determined.[13] In addition, drug effectiveness is generally similar when taken at both MIC and MBC concentrations because the host immune system can expel the pathogen when bacterial proliferation is at a standstill.[24] When the MBC is much higher than the MIC, drug toxicity makes taking the MBC of the drug detrimental to patient. Antimicrobial toxicity can come in many forms, such as immune hypersensitivity and off-target toxicity.[25]
See also
- Kirby–Bauer test
- Arthur Thomas Palin, pioneer in drinking water chlorination treatment and testing
References
- 1 2 Magréault S, Jauréguy F, Carbonnelle E, Zahar JR (December 2010). "When and How to Use MIC in Clinical Practice?". Antibiotics. 11 (12): Article 1748. doi:10.3390/antibiotics11121748. PMC 9774413. PMID 36551405.
- 1 2 Pfaller MA, Andes D, Diekema DJ, Espinel-Ingroff A, Sheehan D (December 2010). "Wild-type MIC distributions, epidemiological cutoff values and species-specific clinical breakpoints for fluconazole and Candida: Time for harmonization of CLSI and EUCAST broth microdilution methods". Drug Resistance Updates. 13 (6): 180–195. doi:10.1016/j.drup.2010.09.002. PMID 21050800.
- ↑ Bennani FE, Doudach L, El Rhayam Y, Karrouchi K, Cherrah Y, Tarib A, Ansar M, Faouzi ME (November 2022). "Identification of the new progress on pyrazole derivatives molecules as antimicrobial and antifungal agents". West African Journal of Medicine. 39 (11): 1217–1244. PMID 36455285.
- 1 2 3 Cushnie TP, Cushnie B, Echeverría J, Fowsantear W, Thammawat S, Dodgson JL, Law S, Clow SM (June 2020). "Bioprospecting for antibacterial drugs: a multidisciplinary perspective on natural product source material, bioassay selection and avoidable pitfalls". Pharmaceutical Research. 37 (7): Article 125. doi:10.1007/s11095-020-02849-1. PMID 32529587. S2CID 254932190.
- ↑ McKinnon PS, Davis SL (April 2004). "Pharmacokinetic and pharmacodynamic issues in the treatment of bacterial infectious diseases". European Journal of Clinical Microbiology & Infectious Diseases. 23 (4): 271–88. doi:10.1007/s10096-004-1107-7. PMID 15015030. S2CID 28455936.
- 1 2 Humphries R, Bobenchik AM, Hindler JA, Schuetz AN (November 2021). "Overview of Changes to the Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Testing, M100, 31st Edition". J Clin Microbiol. 59 (12): Article e0021321. doi:10.1128/JCM.00213-21. PMC 8601225. PMID 34550809.
- ↑ Andrews JM (July 2001). "Determination of minimum inhibitory concentrations". The Journal of Antimicrobial Chemotherapy. 48 Suppl 1 (suppl 1): 5–16. doi:10.1093/jac/48.suppl_1.5. PMID 11420333.
- 1 2 "New definitions of S, I and R from 2019". European Committee on Antimicrobial Susceptibility Testing (EUCAST). Retrieved 5 May 2023.
- ↑ Turnidge JD, Ferraro MJ, Jorgensen JH (2003). "Susceptibility Test Methods: General Considerations". In Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH (eds.). Manual of Clinical Microbiology (8th ed.). Washington: American Society of Clinical Microbiology. p. 1103. ISBN 1-55581-255-4.
- ↑ O'Neill AJ, Chopra I (August 2004). "Preclinical evaluation of novel antibacterial agents by microbiological and molecular techniques". Expert Opinion on Investigational Drugs. 13 (8): 1045–63. doi:10.1517/13543784.13.8.1045. PMID 15268641. S2CID 24016698.
- ↑ Fleming A (1944). On the antibacterial action of cultures of a penicillium, with special reference to their use in the isolation of B. influenzae. H. K. Lewis & Co. Ltd. OCLC 25424051.
- ↑ Wheat PF (July 2001). "History and development of antimicrobial susceptibility testing methodology". The Journal of Antimicrobial Chemotherapy. 48 Suppl 1 (suppl_1): 1–4. doi:10.1093/jac/48.suppl_1.1. PMID 11420332.
- 1 2 Cockerill FR (2012). Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically: approved standard (9th ed.). Wayne, Pa: Clinical and Laboratory Standards Institute. ISBN 978-1562387846. OCLC 1016466655.
- ↑ Cockerill F (2012). Performance standards for antimicrobial susceptibility testing: twenty-second informational supplement. Wayne, PA: Clinical and Laboratory Standards Institute. ISBN 978-1562387853. OCLC 795927370.
- ↑ Diene SM, Abat C, Rolain JM, Raoult D (July 2017). "How artificial is the antibiotic resistance definition?". The Lancet Infectious Diseases. 17 (7): 690. doi:10.1016/S1473-3099(17)30338-9. PMID 28653629.
- ↑ Cameron DR, Howden BP, Peleg AY (September 2011). "The interface between antibiotic resistance and virulence in Staphylococcus aureus and its impact upon clinical outcomes". Clinical Infectious Diseases. 53 (6): 576–82. doi:10.1093/cid/cir473. PMID 21865195.
- ↑ Schwalbe R, Steele-Moore L, Goodwin AC (2007). Antimicrobial susceptibility testing protocols. Boca Raton: CRC Press. ISBN 9781420014495. OCLC 666899344.
- ↑ World Health Organization (2015-12-15). Global antimicrobial resistance surveillance system: manual for early implementation. World Health Organization. Geneva, Switzerland. ISBN 978-9241549400. OCLC 950637154.
{{cite book}}: CS1 maint: location missing publisher (link) - ↑ Geisinger E, Isberg RR (February 2017). "Interplay Between Antibiotic Resistance and Virulence During Disease Promoted by Multidrug-Resistant Bacteria". The Journal of Infectious Diseases. 215 (suppl_1): S9–S17. doi:10.1093/infdis/jiw402. PMC 5853982. PMID 28375515.
- ↑ Gullberg E, Cao S, Berg OG, Ilbäck C, Sandegren L, Hughes D, Andersson DI (July 2011). "Selection of resistant bacteria at very low antibiotic concentrations". PLOS Pathogens. 7 (7): e1002158. doi:10.1371/journal.ppat.1002158. PMC 3141051. PMID 21811410.
- 1 2 Cockerill F (2015). Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically: approved standard (Tenth ed.). Wayne, Pa.: Clinical and Laboratory Standards Institute. ISBN 978-1562387839. OCLC 932608948.
- ↑ "ETEST". bioMérieux. Retrieved 2019-04-23.
- ↑ Tripathi KD (2013). Essentials of Medical Pharmacology (7th ed.). New Delhi, India: Jaypee Brothers Medical Publishers. pp. 696, 697. ISBN 9789350259375.
- ↑ Gallagher JC (2016-11-21). Antibiotics simplified. Jones & Bartlett Publishers. ISBN 9781284111293. OCLC 952657550.
- ↑ Guengerich FP (2011). "Mechanisms of drug toxicity and relevance to pharmaceutical development". Drug Metabolism and Pharmacokinetics. 26 (1): 3–14. doi:10.2133/dmpk.DMPK-10-RV-062. PMC 4707670. PMID 20978361.