
Dietary factors are recognized as having a significant effect on the risk of cancers, with different dietary elements both increasing and reducing risk. Diet and obesity may be related to up to 30–35% of cancer deaths,[1] while physical inactivity appears to be related to 7% risk of cancer occurrence.[2]
While many dietary recommendations have been proposed to reduce the risk of cancer, few have significant supporting scientific evidence.[3] Obesity and drinking alcohol have been correlated with the incidence and progression of some cancers.[3] Lowering the consumption of sweetened beverages is recommended as a measure to address obesity.[4]
Some specific foods are linked to specific cancers. There is strong evidence that processed meat and red meat intake increases risk of colorectal cancer.[5][6][7] Aflatoxin B1, a frequent food contaminant, increases risk of liver cancer,[8] while drinking coffee is associated with a reduced risk.[9] Betel nut chewing causes oral cancer.[8] Stomach cancer is more common in Japan due to its high-salt diet.[8][10] Immigrant communities tend to develop the risk of their new country, often within one generation, suggesting a substantial link between diet and cancer.[11]
Dietary recommendations for cancer prevention typically include weight management and eating a healthy diet, consisting mainly of "vegetables, fruit, whole grains and fish, and a reduced intake of red meat, animal fat, and refined sugar."[3] A healthy dietary pattern may lower cancer risk by 10-20%.[12]
Types of diet
Restrictive diets
A number of diets and diet-based regimes are claimed to be useful against cancer. Popular types of "anti-cancer" diets include the Breuss diet, Gerson therapy, the Budwig protocol and the macrobiotic diet. None of these diets has been found to be effective, and some of them have been found to be harmful.[13]
Dietary patterns
Nutritional epidemiologists use multivariate statistics, such as principal components analysis and factor analysis, to measure how patterns of dietary behavior influence the risk of developing cancer.[14] (The most well-studied dietary pattern is the mediterranean diet.) Based on their dietary pattern score, epidemiologists categorize people into quantiles. To estimate the influence of dietary behavior on risk of cancer, they measure the association between quantiles and the distribution of cancer prevalence (in case-control studies) and cancer incidence (in longitudinal studies). They usually include other variables in their statistical model to account for the other differences between people with and without cancer (confounders). For breast cancer, there is a replicated trend for women with a more "prudent or healthy" diet, i.e. higher in fruits and vegetables, to have a lower risk of cancer.[15] A "drinker dietary pattern" is also associated with higher breast cancer risk, while the association is inconsistent between a more westernized diet and elevated risk of breast cancer. Pickled foods are linked with cancer.
Western pattern diet
The Western pattern diet has been generally linked to increased risk for colorectal cancer.[16] Meta-analyses have found that diet patterns consistent with those of the Western pattern diet are positively correlated with risk for prostate cancer.[17][18] Greater adherence to a Western pattern diet was also found to increase the overall risk of mortality due to cancer.[19]
No significant relation has been established between the Western pattern diet and breast cancer.[20][21]Mediterranean diet
Dietary components
Alcohol
Alcohol is associated with an increased risk of a number of cancers.[26] It has been reported that 3.6% of all cancer cases and 3.5% of cancer deaths worldwide are attributable to drinking of alcohol.[27] Breast cancer in women is linked with alcohol intake.[3][28] Alcohol also increases the risk of cancers of the mouth, esophagus, pharynx and larynx,[29] colorectal cancer,[30][31] liver cancer,[32] stomach[33] and ovaries.[34] The International Agency for Research on Cancer (Centre International de Recherche sur le Cancer) of the World Health Organization has classified alcohol as a Group 1 carcinogen. Its evaluation states, "There is sufficient evidence for the carcinogenicity of alcoholic beverages in humans. ... Alcoholic beverages are carcinogenic to humans (Group 1)."[35]
Eggs
A 2015 meta-analysis found an association between higher egg consumption (5 a week) with increased risk of breast cancer compared to no egg consumption.[36] Another meta-analysis found that egg consumption may increase ovarian cancer risk.[37]
A 2019 meta-analysis found an association between high egg consumption and risk of upper aero-digestive tract cancers in hospital-based case-control studies.[38]
A 2021 review did not find a significant association between egg consumption and breast cancer.[39] A 2021 umbrella review found that egg consumption significantly increases the risk of ovarian cancer.[40]Processed and red meat
There is strong evidence that processed meat and red meat intake increases risk of colorectal cancer.[41][42][43] The American Cancer Society in their "Diet and Physical Activity Guideline", stated "evidence that red and processed meats increase cancer risk has existed for decades, and many health organizations recommend limiting or avoiding these foods."[44]
On October 26, 2015, the International Agency for Research on Cancer of the World Health Organization reported that eating processed meat (e.g., bacon, ham, hot dogs, sausages) or red meat was linked to some cancers and classed them as Group 1 (carcinogenic to humans) and Group 2a (probably carcinogenic to humans) carcinogens respectively.[45] There is some evidence that suggests that heme and nitrite are involved in the processes linking red and processed meat intake with colorectal cancer.[45] Heme is present in particular in red meat and nitrite is used as curing salt in many processed meats.
Salted fish
Fiber, fruits and vegetables
There is strong evidence that consumption of dietary fiber reduces risk of colorectal cancer.[50][51][52] Two 2020 meta-analyses found that a high fiber intake was associated with a lower risk of both premenopausal and postmenopausal breast cancers[53] and a higher survival rate in patients with breast cancer.[54]
A 2021 review found that there is moderate-quality evidence 200g of fruit intake per day is associated with a lower risk of breast cancer.[55] Another review found that high total fruit and vegetable consumption are associated with reduced risk of breast cancer.[56]
Pickled vegetables
The World Health Organization has listed pickled vegetables as a possible carcinogen, and the British Journal of Cancer released an online 2009 meta-analysis of research on pickles as increasing the risks of esophageal cancer. The report, citing limited data in a statistical meta analysis, indicates a potential two-fold increased risk of esophageal cancer associated with Asian pickled vegetable consumption. Results from the research are described as having "high heterogeneity" and the study said that further well-designed prospective studies were warranted.[57] However, their results stated "The majority of subgroup analyses showed a statistically significant association between consuming pickled vegetables and Oesophageal Squamous Cell Carcinoma".[57]
The 2009 meta-analysis reported heavy infestation of pickled vegetables with fungi. Some common fungi can facilitate the formation of N-nitroso compounds, which are strong esophageal carcinogens in several animal models.[58] Roussin red methyl ester,[59] a non-alkylating nitroso compound with tumour-promoting effect in vitro, was identified in pickles from Linzhou, Henan (formerly Linxian) in much higher concentrations than in samples from low-incidence areas. Fumonisin mycotoxins have been shown to cause liver and kidney tumours in rodents.[57]
A 2017 study in Chinese Journal of Cancer[60] has linked salted vegetables (pickled mustard green common among Chinese cuisine) to a fourfold increase in nasopharynx cancer. The researchers believe possible mechanisms include production of nitrosamines (a type of N-nitroso compound) by fermentation and activation of Epstein–Barr virus by fermentation products.[61][62]
Historically, pickling caused health concerns for reasons associated with copper salts, as explained in the mid-19th century The English and Australian Cookery Book: "The evidence of the Lancet commissioner (Dr. Hassall) and Mr. Blackwell (of the eminent firm of Crosse and Blackwell) went to prove that the pickles sold in the shops are nearly always artificially coloured, and are thus rendered highly unwholesome, if not actually poisonous."Flavonoids
Flavonoids (specifically flavonoids such as the catechins) are "the most common group of polyphenolic compounds in the human diet and are found ubiquitously in plants."[63] While some studies have suggested flavonoids may have a role in cancer prevention, others have been inconclusive or suggested they may be harmful.[64][65]
Mushrooms
According to Cancer Research UK, "there is currently no evidence that any type of mushroom or mushroom extract can prevent or cure cancer", although research into some species continues.[66]
Dairy products
The American Institute for Cancer Research (AICR), World Cancer Research Fund International (WCRF), Cancer Council Australia (CCA) and Cancer Research UK have stated that there is strong evidence that consumption of dairy products decreases risk of colorectal cancer.[67][68][69][70] The AICR, WCRF, CCA and Prostate Cancer UK have stated that there is limited but suggestive evidence that dairy products increase risk of prostate cancer.[67][68][69][71][72] The American Cancer Society (ACS) have stated that because dairy products "may lower the risk of some cancers and possibly increase the risk of others, the ACS does not make specific recommendations on dairy food consumption for cancer prevention."[73]
It has been suggested that consumption of insulin-like growth factor 1 (IGF-1) in dairy products could increase cancer risk, particularly prostate cancer.[74][75] However, a 2018 review by the Committee on Carcinogenicity of Chemicals in Food, Consumer Products and the Environment (COC) concluded that there is "insufficient evidence to draw any firm conclusions as to whether exposure to dietary IGF-1 is associated with an increased incidence of cancer in consumers".[75] The COC also stated it is unlikely that there would be absorption of intact IGF-1 from food by most consumers.[76]
A 2019 review concluded that higher-quality research was needed to characterise valid associations between dairy consumption and risk of and/or cancer-related mortality.[77] A 2021 umbrella review found strong evidence that consumption of dairy products decreases risk of colorectal cancer.[78] Fermented dairy is associated with significantly decreased bladder cancer and colorectal cancer risk.[79]
A 2023 review found no association between consumption of dairy products and breast cancer.[80]Whole grains
There is strong evidence that consumption of whole grains decreases risk of colorectal cancer.[51][81][82][83]
Saturated fat
Several reviews of case–control studies have found that saturated fat intake is associated with breast cancer risk and mortality.[84][85][86]
Observational studies have shown that a diet high in saturated fat increases the risk of prostate cancer.[87]Other
- According to the American Cancer Society, there is no conclusive evidence for an anticancer effect of consuming soy products.[88]
- Green tea consumption has no effect on cancer risk.[89][90][91]
- A 2016 meta-analysis showed that women and men who drank coffee had a lower risk of liver cancer.[9] An umbrella review of meta-analyses found that coffee was associated with a lower risk of liver and endometrial cancer.[92]
- A 2014 systematic review found, "no firm evidence that vitamin D supplementation affects cancer occurrence in predominantly elderly community-dwelling women."[93]
Mechanisms of action
Methionine metabolism

Although numerous cellular mechanisms are involved in food intake, many investigations over the past decades have pointed out defects in the methionine metabolic pathway as cause of carcinogenesis.[94][95] For instance, deficiencies of the main dietary sources of methyl donors, methionine and choline, lead to the formation of liver cancer in rodents.[96][97] Methionine is an essential amino acid that must be provided by dietary intake of proteins or methyl donors (choline and betaine found in beef, eggs and some vegetables). Assimilated methionine is transformed in S-adenosyl methionine (SAM) which is a key metabolite for polyamine synthesis, e.g. spermidine, and cysteine formation (see the figure on the right). Methionine breakdown products are also recycled back into methionine by homocysteine remethylation and methylthioadenosine (MTA) conversion (see the figure on the right). Vitamins B6, B12, folic acid and choline are essential cofactors for these reactions. SAM is the substrate for methylation reactions catalyzed by DNA, RNA and protein methyltransferases.
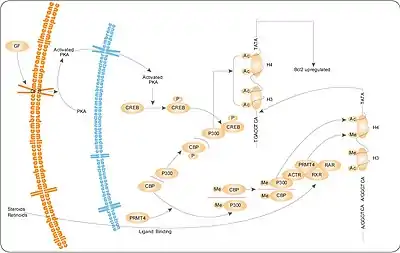
The products of these reactions are methylated DNA, RNA or proteins and S-adenosylhomocysteine (SAH). SAH has a negative feedback on its own production as an inhibitor of methyltransferase enzymes. Therefore, SAM:SAH ratio directly regulates cellular methylation, whereas levels of vitamins B6, B12, folic acid and choline regulates indirectly the methylation state via the methionine metabolism cycle.[98][99] A near ubiquitous feature of cancer is a maladaption of the methionine metabolic pathway in response to genetic or environmental conditions resulting in depletion of SAM and/or SAM-dependent methylation. Whether it is deficiency in enzymes such as methylthioadenosine phosphorylase, methionine-dependency of cancer cells, high levels of polyamine synthesis in cancer, or induction of cancer through a diet deprived of extrinsic methyl donors or enhanced in methylation inhibitors, tumor formation is strongly correlated with a decrease in levels of SAM in mice, rats and humans.[100][101]
According to a 2012 review, the effect of methionine restriction on cancer has yet to be studied directly in humans and "there is still insufficient knowledge to give reliable nutritional advice".[102]
AMPK
AMPK is thought to be a major element or mechanism in cancer-related effects of diet. It modulates the activity of cellular survival signaling such as mTOR and Akt, leading to cell growth inhibition which is relevant to cancer growth. Targeting AMPK has become a novel strategy for cancer prevention and treatment.[103][104][105] Potential complementary or preventive options under investigation include periods of caloric restriction and AMPK agonists (typically mTOR inhibitors).[106][107][108][109][110][111] However, AMPK can also promote cancer in some settings.[103][108]
See also
- Alcohol and cancer
- Alcohol and breast cancer
- Acrylamide
- Bovine Meat and Milk Factors
- Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective
- List of ineffective cancer treatments
- List of topics characterized as pseudoscience
- Microplastics ingested through diet
- Zero waste supermarket
References
- ↑ Anand P, Kunnumakkara AB, Kunnumakara AB, Sundaram C, Harikumar KB, Tharakan ST, et al. (September 2008). "Cancer is a preventable disease that requires major lifestyle changes". Pharmaceutical Research. 25 (9): 2097–2116. doi:10.1007/s11095-008-9661-9. PMC 2515569. PMID 18626751.
- ↑ Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. (June 2016). "Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults". JAMA Internal Medicine. 176 (6): 816–825. doi:10.1001/jamainternmed.2016.1548. PMC 5812009. PMID 27183032.
- 1 2 3 4 Wicki A, Hagmann J (9 September 2011). "Diet and cancer". Swiss Medical Weekly. 141: w13250. doi:10.4414/smw.2011.13250. PMID 21904992.
- ↑ Stewart BW, Wild CP, eds. (2014). "Ch. 2: Cancer Etiology § 6 Diet, obesity and physical activity". World Cancer Report 2014. World Health Organization. pp. 124–33. ISBN 978-92-832-0429-9.
- ↑ "Meat, fish, dairy and cancer risk". wcrf.org. Retrieved 24 April 2023.
- ↑ "Red Meat and Processed Meat Consumption". progressreport.cancer.gov. Retrieved 24 April 2023.
- ↑ "Red Meat (Beef, Pork, Lamb): Increases Risk of Colorectal Cancer". aicr.org. Retrieved 24 April 2023.
- 1 2 3 Park S, Bae J, Nam BH, Yoo KY (2008). "Aetiology of cancer in Asia" (PDF). Asian Pacific Journal of Cancer Prevention. 9 (3): 371–380. PMID 18990005.
- 1 2 Yu C, Cao Q, Chen P, Yang S, Deng M, Wang Y, Li L (December 2016). "An updated dose-response meta-analysis of coffee consumption and liver cancer risk". Scientific Reports. 6 (1): 37488. Bibcode:2016NatSR...637488Y. doi:10.1038/srep37488. PMC 5133591. PMID 27910873.
- ↑ Brenner H, Rothenbacher D, Arndt V (2009). "Epidemiology of Stomach Cancer". In Mukesh V (ed.). Cancer Epidemiology. Methods in Molecular Biology. Vol. 472. pp. 467–477. doi:10.1007/978-1-60327-492-0_23. ISBN 978-1-60327-491-3. PMC 2166976. PMID 19107449.
- ↑ Buell P, Dunn JE (May 1965). "Cancer mortality among Japanese Issei and Nisei of California". Cancer. 18 (5): 656–664. doi:10.1002/1097-0142(196505)18:5<656::AID-CNCR2820180515>3.0.CO;2-3. PMID 14278899.
- ↑ "Preventing Cancer". hsph.harvard.edu. Retrieved 24 April 2023.
- ↑ Hübner J, Marienfeld S, Abbenhardt C, Ulrich CM, Löser C (November 2012). "[How useful are diets against cancer?]". Deutsche Medizinische Wochenschrift. 137 (47): 2417–2422. doi:10.1055/s-0032-1327276. PMID 23152069. S2CID 76124925.
- ↑ Edefonti V, Randi G, La Vecchia C, Ferraroni M, Decarli A (June 2009). "Dietary patterns and breast cancer: a review with focus on methodological issues". Nutrition Reviews. 67 (6): 297–314. doi:10.1111/j.1753-4887.2009.00203.x. PMID 19519672.
- ↑ Brennan SF, Cantwell MM, Cardwell CR, Velentzis LS, Woodside JV (May 2010). "Dietary patterns and breast cancer risk: a systematic review and meta-analysis". The American Journal of Clinical Nutrition. 91 (5): 1294–1302. doi:10.3945/ajcn.2009.28796. PMID 20219961.
- ↑ Fung, Teresa; Hu, Frank B.; Fuchs, Charles; Giovannucci, Edward; Hunter, David J.; Stampfer, Meir J.; Colditz, Graham A.; Willett, Walter C. (2003-02-10). "Major Dietary Patterns and the Risk of Colorectal Cancer in Women". Archives of Internal Medicine. 163 (3): 309–14. doi:10.1001/archinte.163.3.309. ISSN 0003-9926. PMID 12578511.
- ↑ Fabiani, Roberto; Minelli, Liliana; Bertarelli, Gaia; Bacci, Silvia (2016-10-12). "A Western Dietary Pattern Increases Prostate Cancer Risk: A Systematic Review and Meta-Analysis". Nutrients. 8 (10): 626. doi:10.3390/nu8100626. ISSN 2072-6643. PMC 5084014. PMID 27754328.
- ↑ Jalilpiran, Y; Dianatinasab, M; Zeighami, S; Bahmanpour, S; Ghiasvand, R; Mohajeri, SAR; Faghih, S (August–September 2018). "Western Dietary Pattern, But not Mediterranean Dietary Pattern, Increases the Risk of Prostate Cancer". Nutrition and Cancer. 70 (6): 851–859. doi:10.1080/01635581.2018.1490779. PMID 30235016. S2CID 52308508.
- ↑ Entwistle MR, Schweizer D, Cisneros R. Dietary patterns related to total mortality and cancer mortality in the United States. Cancer Causes Control. 2021 Nov;32(11):1279-1288. doi: 10.1007/s10552-021-01478-2. Epub 2021 Aug 11. PMID: 34382130; PMCID: PMC8492557
- ↑ Sánchez-Zamorano, Luisa María; Flores-Luna, Lourdes; Angeles-Llerenas, Angélica; Ortega-Olvera, Carolina; Lazcano-Ponce, Eduardo; Romieu, Isabelle; Mainero-Ratchelous, Fernando; Torres-Mejía, Gabriela (August 2016). "The Western dietary pattern is associated with increased serum concentrations of free estradiol in postmenopausal women: implications for breast cancer prevention". Nutrition Research (New York, N.Y.). 36 (8): 845–854. doi:10.1016/j.nutres.2016.04.008. ISSN 1879-0739. PMID 27440539.
- ↑ Brennan, S. F.; Cantwell, M. M.; Cardwell, C. R.; Velentzis, L. S.; Woodside, J. V. (10 March 2010). "Dietary patterns and breast cancer risk: a systematic review and meta-analysis". American Journal of Clinical Nutrition. 91 (5): 1294–1302. doi:10.3945/ajcn.2009.28796. PMID 20219961.
- ↑ Sofi F, Cesari F, Abbate R, Gensini GF, Casini A (2008). "Adherence to Mediterranean diet and health status: meta-analysis". BMJ (Clinical Research Ed.). 337 (sep11 2): a1344. doi:10.1136/bmj.a1344. PMC 2533524. PMID 18786971.
- ↑ Schwingshackl, L; Hoffmann, G (15 October 2014). "Adherence to Mediterranean diet and risk of cancer: a systematic review and meta-analysis of observational studies". International Journal of Cancer. 135 (8): 1884–97. doi:10.1002/ijc.28824. PMID 24599882. S2CID 10389033.
- ↑ Dinu, M; Pagliai, G; Casini, A; Sofi, F (10 May 2017). "Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials". European Journal of Clinical Nutrition. 72 (1): 30–43. doi:10.1038/ejcn.2017.58. hdl:2158/1081996. PMID 28488692. S2CID 7702206.
- ↑ Morze J, Danielewicz A, Przybyłowicz K (2021). "An updated systematic review and meta-analysis on adherence to mediterranean diet and risk of cancer". European Journal of Nutrition. 60 (3): 1561–1586. doi:10.1007/s00394-020-02346-6. PMC 7987633. PMID 32770356.
- ↑ National Institute on Alcohol Abuse and Alcoholism (NIAAA) (July 1993). "Alcohol and Cancer". Alcohol Alert. 21: PH 345. Archived from the original on 2005-12-23.
- ↑ Boffetta P, Hashibe M, La Vecchia C, Zatonski W, Rehm J (August 2006). "The burden of cancer attributable to alcohol drinking". International Journal of Cancer. 119 (4): 884–887. doi:10.1002/ijc.21903. hdl:2434/22728. PMID 16557583. S2CID 14938863.
- ↑ Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C (May–June 2012). "Epidemiology and pathophysiology of alcohol and breast cancer: Update 2012". Alcohol and Alcoholism. 47 (3): 204–212. doi:10.1093/alcalc/ags011. PMID 22459019.
- ↑ Marmot M, Atinmo T, Byers T, Chen J, Hirohata T, Jackson A, et al. (2007). "Ch. 4: Food and Drinks §8: Alcoholic drinks" (PDF). Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective (PDF). World Cancer Research Fund / American Institute for Cancer Research (AICR) Expert Reports. Vol. 2. Washington, DC: AICR. pp. 157–71. ISBN 978-0-9722522-2-5. Archived from the original (PDF) on 2016-05-07. Retrieved 2014-08-29.
- ↑ Su LJ, Arab L (2004). "Alcohol consumption and risk of colon cancer: evidence from the national health and nutrition examination survey I epidemiologic follow-up study". Nutrition and Cancer. 50 (2): 111–119. doi:10.1207/s15327914nc5002_1. PMID 15623458. S2CID 25461607.
- ↑ Cho E, Smith-Warner SA, Ritz J, van den Brandt PA, Colditz GA, Folsom AR, et al. (April 2004). "Alcohol intake and colorectal cancer: a pooled analysis of 8 cohort studies". Annals of Internal Medicine. 140 (8): 603–613. doi:10.7326/0003-4819-140-8-200404200-00007. PMID 15096331. S2CID 37915731.
- ↑ Voigt MD (February 2005). "Alcohol in hepatocellular cancer". Clinics in Liver Disease. 9 (1): 151–169. doi:10.1016/j.cld.2004.10.003. PMID 15763234.
- ↑ Benedetti A, Parent ME, Siemiatycki J (2009). "Lifetime consumption of alcoholic beverages and risk of 13 types of cancer in men: results from a case-control study in Montreal". Cancer Detection and Prevention. 32 (5–6): 352–362. doi:10.1016/j.canep.2009.03.001. PMID 19588541.
- ↑ Bagnardi V, Blangiardo M, La Vecchia C, Corrao G (2001). "Alcohol consumption and the risk of cancer: a meta-analysis". Alcohol Research & Health. 25 (4): 263–270. PMC 6705703. PMID 11910703.
- ↑ Berrino F, Grant M, Griciute L, Holmberg B, McMichael AJ, Møller-Jensen O, et al. (IARC Working Group on the Evaluation of Carcinogenic Risks to Humans: Alcohol Drinking) (1988). "Ch. 6: Summary of Data Reported and Evaluation §5: Evaluation" (PDF). Alcohol Drinking. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 44. Lyon: International Agency for Research on Cancer (IARC): World Health Organization. pp. 258–9. ISBN 978-92-832-1244-7.
- ↑ Keum N, Lee DH, Marchand N, Oh H, Liu H, Aune D, Greenwood DC, Giovannucci EL (2015). "Egg intake and cancers of the breast, ovary and prostate: a dose-response meta-analysis of prospective observational studies". British Journal of Nutrition. 114 (7): 1099–107. doi:10.1017/S0007114515002135. hdl:10044/1/48759. PMID 26293984. S2CID 31168561.
- ↑ Zeng ST, Guo L, Liu SK, et al. (2015). "Egg consumption is associated with increased risk of ovarian cancer: Evidence from a meta-analysis of observational studies". Clinical Nutrition. 34 (4): 635–641. doi:10.1016/j.clnu.2014.07.009. PMID 25108572.
- ↑ Aminianfar A, Fallah-Moshkani R, Salari-Moghaddam A, et al. (2019). "Egg Consumption and Risk of Upper Aero-Digestive Tract Cancers: A Systematic Review and Meta-Analysis of Observational Studies". Advances in Nutrition. 10 (4): 660–672. doi:10.1093/advances/nmz010. PMC 6628841. PMID 31041448.
- ↑ Kazemi A, Barati-Boldaji R, Soltani S, et al. (2021). "Intake of Various Food Groups and Risk of Breast Cancer: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies". Advances in Nutrition. 12 (3): 809–849. doi:10.1093/advances/nmaa147. PMC 8166564. PMID 33271590.
- ↑ Tanha K, Mottaghi A, Nojomi M, Moradi M, Rajabzadeh R, Lotfi S, Janani L (2021). "Investigation on factors associated with ovarian cancer: an umbrella review of systematic review and meta-analyses". Journal of Ovarian Research. 14 (1): 153. doi:10.1186/s13048-021-00911-z. PMC 8582179. PMID 34758846.
- ↑ "Does eating processed and red meat cause cancer?". Cancer Research UK. 25 June 2019. Retrieved 30 December 2022.
- ↑ "Red Meat (Beef, Pork, Lamb): Increases Risk of Colorectal Cancer". American Institute for Cancer Research. Retrieved 30 December 2022.
- ↑ "Limit red and processed meat". WCRF International. Retrieved 30 December 2022.
- ↑ Rock, Cheryl L.; Thomson, Cynthia; Gansler, Ted; Gapstur, Susan M.; McCullough, Marjorie L.; Patel, Alpa V.; Andrews, Kimberly S.; Bandera, Elisa V.; Spees, Colleen K.; Robien, Kimberly; Hartman, Sheri; Sullivan, Kristen; Grant, Barbara L.; Hamilton, Kathryn K.; Kushi, Lawrence H.; Caan, Bette J.; Kibbe, Debra; Black, Jessica Donze; Wiedt, Tracy L.; McMahon, Catherine; Sloan, Kirsten; Doyle, Colleen (2020). "American Cancer Society guideline for diet and physical activity for cancer prevention". CA. 70 (4): 245–271. doi:10.3322/caac.21591. PMID 32515498. S2CID 219550658.
- 1 2 Staff (October 26, 2015). "World Health Organization - IARC Monographs evaluate consumption of red meat and processed meat" (PDF). International Agency for Research on Cancer. Retrieved October 26, 2015.
- ↑ "Diet, Nutrition, Physical Activity and Cancer: A Global Perspective". wcrf.org. Retrieved 14 February 2023. "There is strong evidence, mostly from Asia, that consuming foods preserved by salting (including salt-preserved vegetables, fish and salt-preserved foods in general) is a cause of stomach cancer."
- ↑ "Meat, fish and dairy products and the risk of cancer". wcrf.org. Retrieved 14 February 2023.
- ↑ "Known and Probable Human Carcinogens". cancer.org. Retrieved 14 February 2023.
- ↑ "Agents classified by the IARC Monographs". monographs.iarc.who.int. Retrieved 14 February 2023.
- ↑ "Wholegrains, vegetables, fruit and cancer risk". wcrf.org. Retrieved 13 April 2023.
- 1 2 "Wholegrains, vegetables and fruit and the risk of cancer". wcrf.org. Retrieved 13 April 2023.
- ↑ Jabbari M, Pourmoradian S, Eini-Zinab H, Mosharkesh E, Hosseini Balam F, Yaghmaei Y, Yadegari A, Amini B, Arman Moghadam D, Barati M, Hekmatdoost A (2022). "Levels of evidence for the association between different food groups/items consumption and the risk of various cancer sites: an umbrella review". Int J Food Sci Nutr. 73 (7): 861–874. doi:10.1080/09637486.2022.2103523. PMID 35920747. S2CID 251280745.
- ↑ Farvid MS, Spence ND, Holmes MD, Barnett JB (July 2020). "Fiber consumption and breast cancer incidence: A systematic review and meta-analysis of prospective studies". Cancer. 126 (13): 3061–3075. doi:10.1002/cncr.32816. PMID 32249416. S2CID 214809009.
- ↑ Jayedi A, Emadi A, Khan TA, Abdolshahi A, Shab-Bidar S (2020). "Dietary Fiber and Survival in Women with Breast Cancer: A Dose-Response Meta-Analysis of Prospective Cohort Studies". Nutrition and Cancer. 73 (9): 1570–1580. doi:10.1080/01635581.2020.1803928. PMID 32795218. S2CID 221132662.
- ↑ Sun L, Liang X (2021). "Fruit consumption and multiple health outcomes: An umbrella review". Trends in Food Science & Technology. 118: 505–528. doi:10.1016/j.tifs.2021.09.023. S2CID 244212291.
- ↑ Farvid MS, Barnett JB, Spence ND (2021). "Fruit and vegetable consumption and incident breast cancer: a systematic review and meta-analysis of prospective studies". Br J Cancer. 125 (2): 284–298. doi:10.1038/s41416-021-01373-2. PMC 8292326. PMID 34006925.
- 1 2 3 Islami, F (2009). "Pickled vegetables and the risk of oesophageal cancer: a meta-analysis". British Journal of Cancer. 101 (9): 1641–1647. doi:10.1038/sj.bjc.6605372. PMC 2778505. PMID 19862003.
- ↑ Li, MH; Ji, C; Cheng, SJ (1986). "Occurrence of nitroso compounds in fungi‐contaminated foods: A review". Nutrition and Cancer. 8 (1): 63–69. doi:10.1080/01635588609513877. PMID 3520493.
- ↑ Liu, J. G.; Li, M. H. (1989). "Roussin red methyl ester, a tumor promoter isolated from pickled vegetables". Carcinogenesis. 10 (3): 617–620. doi:10.1093/carcin/10.3.617. PMID 2494003.
- ↑ Yong, SK; Ha, TC; Yeo, MC; Gaborieau, V; McKay, JD; Wee, J (7 January 2017). "Associations of lifestyle and diet with the risk of nasopharyngeal carcinoma in Singapore: a case-control study". Chinese Journal of Cancer. 36 (1): 3. doi:10.1186/s40880-016-0174-3. PMC 5219694. PMID 28063457.
- ↑ "Study: Salted vegetables increase risk of nose cancer". 16 January 2017. Retrieved 15 February 2018.
- ↑ "Health". Archived from the original on 23 April 2017. Retrieved 15 February 2018.
- ↑ Spencer JP (May 2008). "Flavonoids: modulators of brain function?". The British Journal of Nutrition. 99 E Suppl 1 (E Suppl 1): ES60–ES77. doi:10.1017/S0007114508965776. PMID 18503736.
- ↑ Romagnolo DF, Selmin OI (2012). "Flavonoids and cancer prevention: a review of the evidence". Journal of Nutrition in Gerontology and Geriatrics. 31 (3): 206–238. doi:10.1080/21551197.2012.702534. PMID 22888839. S2CID 205960210.
- ↑ Jin H, Leng Q, Li C (August 2012). "Dietary flavonoid for preventing colorectal neoplasms". Colorectal Cancer Group. The Cochrane Database of Systematic Reviews. 8 (8): CD009350. doi:10.1002/14651858.CD009350.pub2. PMID 22895989.
- ↑ "Mushrooms in cancer treatment § Mushrooms and cancer". www.cancerresearchuk.org. Cancer Research UK. 30 January 2013. Archived from the original on 2014-07-08.
- 1 2 Clinton SK, Giovannucci EL, Hursting SD (2020). "The World Cancer Research Fund/American Institute for Cancer Research Third Expert Report on Diet, Nutrition, Physical Activity, and Cancer: Impact and Future Directions". The Journal of Nutrition. 150 (4): 663–671. doi:10.1093/jn/nxz268. PMC 7317613. PMID 31758189.
- 1 2 "Meat, fish and dairy products and the risk of cancer". wcrf.org. Retrieved 24 January 2023.
- 1 2 "Information sheet: Dairy foods and cancer". cancer.org.au. Retrieved 24 January 2023.
- ↑ "Can milk and dairy products cause cancer?". cancerresearchuk.org. Retrieved 24 January 2023.
- ↑ "Diet, nutrition, physical activity and prostate cancer". wcrf.org. Retrieved 24 January 2023.
- ↑ "Which foods might increase my risk of prostate cancer?". prostatecanceruk.org. Retrieved 24 January 2023.
- ↑ "American Cancer Society Guideline for Diet and Physical Activity". cancer.org. Retrieved 24 January 2023.
- ↑ Harrison S, Lennon R, Holly J, Higgins JP, Gardner M, Perks C, Gaunt T, Tan V, Borwick C, Emmet P, Jeffreys M, Northstone K, Rinaldi S, Thomas S, Turner SD, Pease A, Vilenchick V, Martin RM, Lewis SJ (2017). "Does milk intake promote prostate cancer initiation or progression via effects on insulin-like growth factors (IGFs)? A systematic review and meta-analysis". Cancer Causes Control. 28 (6): 497–528. doi:10.1007/s10552-017-0883-1. PMC 5400803. PMID 28361446.
- 1 2 "Statement on possible carcinogenic hazard to consumers from insulin-like growth factor-1 (IGF-1) in the diet. assets.publishing.service.gov.uk. Retrieved 4 February 2023.
- ↑ "Non-Technical Summary of Statement on possible carcinogenic hazard to consumers from insulin-like growth factor-1 (IGF-1) in the diet". assets.publishing.service.gov.uk. Retrieved 4 February 2023.
- ↑ Jeyaraman, Maya M; Abou-Setta, Ahmed M; Grant, Laurel; Farshidfar, Farnaz; Copstein, Leslie; Lys, Justin; Gottschalk, Tania; Desautels, Danielle; Czaykowski, Piotr; Pitz, Marshall; Zarychanski, Ryan (2019). "Dairy product consumption and development of cancer: an overview of reviews". BMJ Open. 9 (1): e023625. doi:10.1136/bmjopen-2018-023625. ISSN 2044-6055. PMC 6352799. PMID 30782711.
- ↑ Papadimitriou N, Markozannes G, Kanellopoulou A, Critselis E, Alhardan S, Karafousia V, Kasimis JC, Katsaraki C, Papadopoulou A, Zografou M, Lopez DS, Chan DS, Kyrgiou M, Ntzani E, Cross AJ, Marrone MT, Platz EA, Gunter MJ, Tsilidis KK (2021). "An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites". Nature Communications. 12 (1): 4579. Bibcode:2021NatCo..12.4579P. doi:10.1038/s41467-021-24861-8. PMC 8319326. PMID 34321471.
- ↑ Zhang K, Dai H, Liang W, Zhang L, Deng Z (2019). "Fermented dairy foods intake and risk of cancer". Int J Cancer. 144 (9): 2099–2108. doi:10.1002/ijc.31959. PMID 30374967. S2CID 53114731.
- ↑ Arafat HM, Omar J, Shafii N, Naser IA, Al Laham NA, Muhamad R, Al-Astani TA, Shaqaliah AJ, Shamallakh OM, Shamallakh KM, Abusalah MA (2023). "The association between breast cancer and consumption of dairy products: a systematic review". Ann Med. 55 (1): 2198256. doi:10.1080/07853890.2023.2198256. PMC 10120447. PMID 37078247.
- ↑ Clinton SK, Giovannucci EL, Hursting SD (2020). "The World Cancer Research Fund/American Institute for Cancer Research Third Expert Report on Diet, Nutrition, Physical Activity, and Cancer: Impact and Future Directions". The Journal of Nutrition. 150 (4): 663–671. doi:10.1093/jn/nxz268. PMC 7317613. PMID 31758189.
- ↑ Papadimitriou N, Markozannes G, Kanellopoulou A, Critselis E, Alhardan S, Karafousia V, Kasimis JC, Katsaraki C, Papadopoulou A, Zografou M, Lopez DS, Chan DS, Kyrgiou M, Ntzani E, Cross AJ, Marrone MT, Platz EA, Gunter MJ, Tsilidis KK (2021). "An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites". Nature Communications. 12 (1): 4579. Bibcode:2021NatCo..12.4579P. doi:10.1038/s41467-021-24861-8. PMC 8319326. PMID 34321471.
- ↑ Zhang XF, Wang XK, Tang YJ, Guan XX, Guo Y, Fan JM, Cui LL (2021). "Association of whole grains intake and the risk of digestive tract cancer: a systematic review and meta-analysis". Nutrition Journal. 19 (1): 52. doi:10.1186/s12937-020-00556-6. PMC 7271550. PMID 32493399.
- ↑ Xia, H; Ma, S; Wang, S; Sun, G. (2015). "Meta-Analysis of Saturated Fatty Acid Intake and Breast Cancer Risk". Medicine. 94 (52): e2391. doi:10.1097/MD.0000000000002391. PMC 5291630. PMID 26717389.
- ↑ Brennan, SF; Woodside, JV; Lunny, PM; Cardwell, CR; Cantwell, MM. (2017). "Dietary fat and breast cancer mortality: A systematic review and meta-analysis". Critical Reviews in Food Science and Nutrition. 57 (10): 1999–2008. doi:10.1080/10408398.2012.724481. PMID 25692500. S2CID 34098509.
- ↑ Dandamudi, A; Tommie, J; Nommsen-Rivers, L; Couch, S. (2018). "Dietary Patterns and Breast Cancer Risk: A Systematic Review". Anticancer Research. 38 (6): 3209–3222. doi:10.21873/anticanres.12586. PMID 29848668. S2CID 44149964.
- ↑ Gathirua-Mwangi, Wambui G.; Zhang, Jianjun (2014). "Dietary factors and risk for advanced prostate cancer". European Journal of Cancer Prevention. 23 (2): 96–109. doi:10.1097/CEJ.0b013e3283647394. PMC 4091618. PMID 23872953.
- ↑ "Soybean". www.cancer.org. American Cancer Society. 17 January 2013. Archived from the original on 2014-08-26.
- ↑ Filippini T, Malavolti M, Borrelli F, Izzo AA, Fairweather-Tait SJ, Horneber M, Vinceti M (March 2020). "Green tea (Camellia sinensis) for the prevention of cancer". The Cochrane Database of Systematic Reviews. 3 (11): CD005004. doi:10.1002/14651858.CD005004.pub3. PMC 7059963. PMID 32118296.
- ↑ "Green Tea". www.cancer.org. American Cancer Society. 4 May 2012. Archived from the original on 2014-08-26.
- ↑ Zhao LG, Li ZY, Feng GS, Ji XW, Tan YT, Li HL, et al. (March 2021). "Tea Drinking and Risk of Cancer Incidence: A Meta-Analysis of Prospective Cohort Studies and Evidence Evaluation". Advances in Nutrition. 12 (2): 402–412. doi:10.1093/advances/nmaa117. PMC 8009746. PMID 33002099.
- ↑ Zhao LG, Li ZY, Feng GS, Ji XW, Tan YT, Li HL, et al. (February 2020). "Coffee drinking and cancer risk: an umbrella review of meta-analyses of observational studies". BMC Cancer. 20 (1): 101. doi:10.1186/s12885-020-6561-9. PMC 7003434. PMID 32024485.
- ↑ Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Krstic G, Wetterslev J, Gluud C (June 2014). "Vitamin D supplementation for prevention of cancer in adults". Metabolic and Endocrine Disorders Group. The Cochrane Database of Systematic Reviews. 6 (6): CD007469. doi:10.1002/14651858.CD007469.pub2. PMID 24953955.
- ↑ Mikol YB, Hoover KL, Creasia D, Poirier LA (December 1983). "Hepatocarcinogenesis in rats fed methyl-deficient, amino acid-defined diets". Carcinogenesis. 4 (12): 1619–1629. doi:10.1093/carcin/4.12.1619. PMID 6317218.
- ↑ Ghoshal AK, Farber E (October 1984). "The induction of liver cancer by dietary deficiency of choline and methionine without added carcinogens". Carcinogenesis. 5 (10): 1367–1370. doi:10.1093/carcin/5.10.1367. PMID 6488458.
- ↑ Newmark HL, Yang K, Lipkin M, Kopelovich L, Liu Y, Fan K, Shinozaki H (November 2001). "A Western-style diet induces benign and malignant neoplasms in the colon of normal C57Bl/6 mice". Carcinogenesis. 22 (11): 1871–1875. doi:10.1093/carcin/22.11.1871. PMID 11698351.
- ↑ Henning SM, Swendseid ME, Coulson WF (January 1997). "Male rats fed methyl- and folate-deficient diets with or without niacin develop hepatic carcinomas associated with decreased tissue NAD concentrations and altered poly(ADP-ribose) polymerase activity". The Journal of Nutrition. 127 (1): 30–36. doi:10.1093/jn/127.1.30. PMID 9040540.
- ↑ Caudill MA, Wang JC, Melnyk S, Pogribny IP, Jernigan S, Collins MD, et al. (November 2001). "Intracellular S-adenosylhomocysteine concentrations predict global DNA hypomethylation in tissues of methyl-deficient cystathionine beta-synthase heterozygous mice". The Journal of Nutrition. 131 (11): 2811–2818. doi:10.1093/jn/131.11.2811. PMID 11694601.
- ↑ Poirier LA, Wise CK, Delongchamp RR, Sinha R (June 2001). "Blood determinations of S-adenosylmethionine, S-adenosylhomocysteine, and homocysteine: correlations with diet". Cancer Epidemiology, Biomarkers & Prevention. 10 (6): 649–655. PMID 11401915.
- ↑ Prinz-Langenohl R, Fohr I, Pietrzik K (June 2001). "Beneficial role for folate in the prevention of colorectal and breast cancer". European Journal of Nutrition. 40 (3): 98–105. doi:10.1007/PL00007387. PMID 11697447. S2CID 39886028.
- ↑ Van den Veyver IB (2002). "Genetic effects of methylation diets". Annual Review of Nutrition. 22: 255–282. doi:10.1146/annurev.nutr.22.010402.102932. PMID 12055346.
- ↑ Cavuoto P, Fenech MF (October 2012). "A review of methionine dependency and the role of methionine restriction in cancer growth control and life-span extension". Cancer Treatment Reviews. 38 (6): 726–736. doi:10.1016/j.ctrv.2012.01.004. PMID 22342103.
- 1 2 Wang, Zhiyu; Wang, Neng; Liu, Pengxi; Xie, Xiaoming (2016). "AMPK and Cancer". AMP-activated Protein Kinase. Experientia Supplementum. Vol. 107. Springer International Publishing. pp. 203–226. doi:10.1007/978-3-319-43589-3_9. ISBN 978-3-319-43587-9. PMID 27812982.
{{cite book}}:|journal=ignored (help) - ↑ Carling, David (April 2017). "AMPK signalling in health and disease". Current Opinion in Cell Biology. 45: 31–37. doi:10.1016/j.ceb.2017.01.005. hdl:10044/1/45767. PMID 28232179.
- ↑ Li, Jin; Zhong, Liping; Wang, Fengzhong; Zhu, Haibo (May 2017). "Dissecting the role of AMP-activated protein kinase in human diseases". Acta Pharmaceutica Sinica B. 7 (3): 249–259. doi:10.1016/j.apsb.2016.12.003. PMC 5430814. PMID 28540163.
- ↑ Yung, Mingo M.H.; Ngan, Hextan Y.S.; Chan, David W. (1 April 2016). "Targeting AMPK signaling in combating ovarian cancers: opportunities and challenges". Acta Biochimica et Biophysica Sinica. 48 (4): 301–317. doi:10.1093/abbs/gmv128. PMC 4886241. PMID 26764240.
- ↑ Meynet, Ophélie; Ricci, Jean-Ehrland (August 2014). "Caloric restriction and cancer: molecular mechanisms and clinical implications". Trends in Molecular Medicine. 20 (8): 419–427. doi:10.1016/j.molmed.2014.05.001. ISSN 1471-499X. PMID 24916302.
- 1 2 Fay, Judith R.; Steele, Vernon; Crowell, James A. (1 April 2009). "Energy Homeostasis and Cancer Prevention: The AMP-Activated Protein Kinase". Cancer Prevention Research. 2 (4): 301–309. doi:10.1158/1940-6207.CAPR-08-0166. PMID 19336731. S2CID 22495750.
- ↑ Skuli, Sarah J.; Alomari, Safwan; Gaitsch, Hallie; Bakayoko, A'ishah; Skuli, Nicolas; Tyler, Betty M. (19 May 2022). "Metformin and Cancer, an Ambiguanidous Relationship". Pharmaceuticals. 15 (5): 626. doi:10.3390/ph15050626. PMC 9144507. PMID 35631452.
- ↑ Ingram, Donald K.; Roth, George S. (June 2021). "Glycolytic inhibition: an effective strategy for developing calorie restriction mimetics". GeroScience. 43 (3): 1159–1169. doi:10.1007/s11357-020-00298-7. PMC 8190254. PMID 33184758.
- ↑ Guigas, Bruno; Viollet, Benoit (2016). "Targeting AMPK: From Ancient Drugs to New Small-Molecule Activators". AMP-activated Protein Kinase. Experientia Supplementum. Vol. 107. pp. 327–350. doi:10.1007/978-3-319-43589-3_13. ISBN 978-3-319-43587-9. PMID 27812986.
{{cite book}}:|journal=ignored (help)
External links
- "Diet, healthy eating and cancer". info.cancerresearchuk.org. Cancer Research UK. 2013-08-22.
- "EPIC (European Prospective Investigation into Cancer and Nutrition) Study". epic.iarc.fr. International Agency for Research on Cancer: World Health Organization.