Publicly funded healthcare is a form of health care financing designed to meet the cost of all or most healthcare needs from a publicly managed fund. Usually this is under some form of democratic accountability, the right of access to which are set down in rules applying to the whole population contributing to the fund or receiving benefits from it.
The fund may be a not-for-profit trust that pays out for healthcare according to common rules established by the members or by some other democratic form. In some countries, the fund is controlled directly by the government or by an agency of the government for the benefit of the entire population. That distinguishes it from other forms of private medical insurance, the rights of access to which are subject to contractual obligations between an insured person (or their sponsor) and an insurance company, which seeks to make a profit by managing the flow of funds between funders and providers of health care services.
When taxation is the primary means of financing health care and sometimes with compulsory insurance, all eligible people receive the same level of cover regardless of their financial circumstances or risk factors.[1]
Varieties of public systems
Most developed countries have partially or fully publicly funded health systems. Most western industrial countries have a system of social insurance based on the principle of social solidarity that covers eligible people from bearing the direct burden of most health care expenditure, funded by taxation during their working life.
Among countries with significant public funding of healthcare there are many different approaches to the funding and provision of medical services. Systems may be funded from general government revenues (as in Canada, United Kingdom, Brazil and India) or through a government social security system (as in Australia, France, Belgium, Japan and Germany) with a separate budget and hypothecated taxes or contributions. The proportion of the cost of care covered also differs: in Canada, all hospital care is paid for by the government, while in Japan, patients must pay 10 to 30% of the cost of a hospital stay. Services provided by public systems vary. For example, the Belgian government pays the bulk of the fees for dental and eye care, while the Australian government covers eye care but not dental care.
Publicly funded medicine may be administered and provided by the government, as in the Nordic countries, Portugal, Spain, and Italy; in some systems, though, medicine is publicly funded but most hospital providers are private entities, as in Canada. The organization providing public health insurance is not necessarily a public administration, and its budget may be isolated from the main state budget. Some systems do not provide universal healthcare or restrict coverage to public health facilities. Some countries, such as Germany, have multiple public insurance organizations linked by a common legal framework. Some, such as the Netherlands and Switzerland, allow private for-profit insurers to participate.
Two-tier healthcare
Almost every major country that has a publicly funded healthcare system also has a parallel private system for patients who hold private medical insurance or themselves pay for treatment.[2] In those states, those able to pay have access to treatment and comforts that may not be available to those dependent upon the state system.
From the inception of the NHS model (1948), public hospitals in the United Kingdom have included "amenity beds" which would typically be siderooms fitted more comfortably, and private wards in some hospitals where for a fee more amenities are provided. Patients using these beds are in an NHS hospital for surgical treatment, and operations are generally carried out in the same operating theatres as NHS work and by the same personnel but the hospital and the physician receive funding from an insurance company or the patient. These amenity beds do not exist in all publicly funded systems, such as in Spain. The NHS also pays for private hospitals to take on surgical cases under contract.
Policy discussion
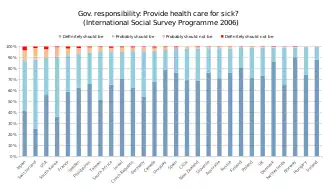
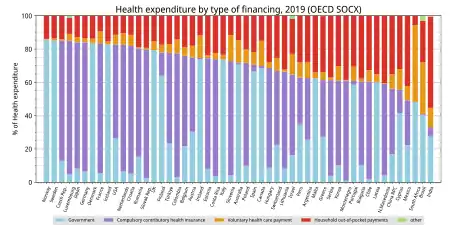
Many countries are seeking the right balance of public and private insurance, public subsidies, and out-of-pocket payments.
Many OECD countries have implemented reforms to achieve policy goals of ensuring access to health care, improving the quality of health care and health outcomes, allocating an appropriate level of public sector other resources to healthcare but at the same time ensuring that services are provided in a cost-efficient and cost-effective manner (microeconomic efficiency). A range of measures, such as better payment methods, have improved the microeconomic incentives facing providers. However, introducing improved incentives through a more competitive environment among providers and insurers has proved difficult.[3]
A 2009 Harvard study published in the American Journal of Public Health found more than 44,800 excess deaths annually in the United States because of Americans' lacking health insurance, equivalent to one excess death every 12 min.[4][5] More broadly, the total number of people in the United States, whether insured or uninsured, who die because of lack of medical care was estimated in a 1997 analysis to be nearly 100,000 per year.[6]
See also
- Global health
- Health policy
- Health system
- Health law
- Health care compared for varying degrees of public funding
- National health insurance
- Public opinion on health care reform in the United States
- Single-payer health care
- Socialized medicine
- Social insurance
- Universal health care
- National Health Service of the United Kingdom
References
- ↑ Claude Blanchette, Erin Tolley. "PUBLIC- AND PRIVATE-SECTOR INVOLVEMENT IN HEALTH-CARE SYSTEMS: A COMPARISON OF OECD COUNTRIES." May 1997. Retrieved September 12, 2006.
- ↑ "Supreme Court of Canada - Decisions - Chaoulli v. Quebec (Attorney General)". Archived from the original on 2011-02-02. Retrieved 2011-02-11. Canadian Supreme Court, after expert testimony, found that all OECD countries and four of the ten Canadian provinces allow private medical insurance alongside the state system
- ↑ Elizabeth Docteur; Howard Oxley (2003). "Health-Care Systems: Lessons from the Reform Experience" (PDF). OECD.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU (December 2009). "Health Insurance and Mortality in US Adults" (PDF). American Journal of Public Health. 99 (12): 2289–2295. doi:10.2105/ajph.2008.157685. PMC 2775760. PMID 19762659. Retrieved 10 September 2014.
- ↑ State-by-state breakout of excess deaths from lack of insurance
- ↑ A 1997 study carried out by Professors David Himmelstein and Steffie Woolhandler (New England Journal of Medicine 336, no. 11 [1997]) "concluded that almost 100,000 people died in the United States each year because of lack of needed care—three times the number of people who died of AIDs." The Inhuman State of U.S. Health Care, Monthly Review, Vicente Navarro, September 2003. Retrieved 2009-09-10
Further reading
- Devereaux PJ, Choi PT, Lacchetti C, et al. (May 2002). "A systematic review and meta-analysis of studies comparing mortality rates of private for-profit and private not-for-profit hospitals". CMAJ. 166 (11): 1399–406. PMC 111211. PMID 12054406.
- Devereaux PJ, Heels-Ansdell D, Lacchetti C, et al. (June 2004). "Payments for care at private for-profit and private not-for-profit hospitals: a systematic review and meta-analysis". CMAJ. 170 (12): 1817–24. doi:10.1503/cmaj.1040722. PMC 419772. PMID 15184339.
- Doctors support universal health care: survey, Reuters, March 31, 2008 (first reported in Annals of Internal Medicine).
- Krauss, C. As Canada's Slow-Motion Public Health System Falters, Private Medical Care is Surging, New York Times, February 26, 2006.
- Woolhandler S, Himmelstein DU (August 1999). "When money is the mission—the high costs of investor-owned care". N. Engl. J. Med. 341 (6): 444–6. doi:10.1056/NEJM199908053410611. PMID 10432332.