| Shoulder impingement syndrome | |
|---|---|
| Other names | Subacromial impingement, painful arc syndrome, supraspinatus syndrome, swimmer's shoulder, thrower's shoulder |
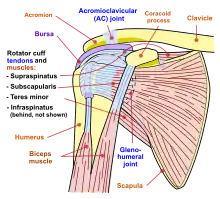 | |
| Shoulder joint | |
| Specialty | Orthopedics, sports medicine |
Shoulder impingement syndrome is a syndrome involving tendonitis (inflammation of tendons) of the rotator cuff muscles as they pass through the subacromial space, the passage beneath the acromion. It is particularly associated with tendonitis of the supraspinatus muscle.[1] This can result in pain, weakness, and loss of movement at the shoulder.[2][3]
Signs and symptoms
The most common symptoms in impingement syndrome are pain, weakness and a loss of movement at the affected shoulder.[2] The pain is often worsened by shoulder overhead movement and may occur at night, especially when lying on the affected shoulder. The onset of the pain may be acute if due to an injury or insidious if due to a gradual process such as an osteoarthritic spur. The pain has been described as dull rather than sharp, and lingers for long periods of time, making it hard to fall asleep.[2] Other symptoms can include a grinding or popping sensation during movement of the shoulder.[4]
The range of motion at the shoulder may be limited by pain. A painful arc of movement may be present during forward elevation of the arm from 60° to 120°.[4] Passive movement at the shoulder will appear painful when a downward force is applied at the acromion but the pain will ease once the force is removed.[2]
Causes
| Type | Appearance | Prevalence[5] | Angle of anterior slope[5] |
|---|---|---|---|
| Flat |  | 17.1% | 13.18 |
| Curved |  | 42.9% | 29.98 |
| Hooked |  | 39.3% | 26.98 |
When the arm is raised, the subacromial space (gap between the anterior edge of the acromion and the head of the humerus) narrows; the supraspinatus muscle tendon passes through this space.[6] Anything that causes further narrowing has the tendency to impinge the tendon and cause an inflammatory response, resulting in impingement syndrome. Such causes can be bony structures such as subacromial spurs (bony projections from the acromion), osteoarthritic spurs on the acromioclavicular joint, and variations in the shape of the acromion. Thickening or calcification of the coracoacromial ligament can also cause impingement. Loss of function of the rotator cuff muscles, due to injury or loss of strength, may cause the humerus to move superiorly, resulting in impingement. Inflammation and subsequent thickening of the subacromial bursa may also cause impingement.[2]
Weight training exercises where the arms are elevated above shoulder height but in an internally rotated position such as the upright row have been suggested as a cause of subacromial impingement.[7] Another common cause of Impingement syndrome is restrictions in the range movement of the scapulo-thoracic surfaces. Commonly, one or more ribs between rib 2 and rib 7/8 on the side of the impingement may jut out slightly and/or feel hard when the person springs on it or them. When this occurs, the scapula is raised and anteverted (angled forwards). This in turn pushes the acromion and the humeral head out of its usual anatomical position placing pressure downwards at the head of the humerus at the position of the nerve thus causing the impingement syndrome. This is visibly demonstrated by a slightly raised and protracted shoulder girdle. Note: the humerus anteverts in this position causing a more protrusive section of the humerus to press upwards towards the acromion.
Mechanism
The scapula plays an important role in shoulder impingement syndrome.[8] It is a wide, flat bone lying on the posterior thoracic wall that provides an attachment for three different groups of muscles. The intrinsic muscles of the scapula include the muscles of the rotator cuff- the subscapularis, infraspinatus, teres minor and supraspinatus.[9] These muscles attach to the surface of the scapula and are responsible for the internal and external rotation of the glenohumeral joint, along with humeral abduction. The extrinsic muscles include the biceps, triceps, and deltoid muscles and attach to the coracoid process and supraglenoid tubercle of the scapula, infraglenoid tubercle of the scapula, and spine of the scapula. These muscles are responsible for several actions of the glenohumeral joint. The third group, which is mainly responsible for stabilization and rotation of the scapula, consists of the trapezius, serratus anterior, levator scapulae, and rhomboid muscles and attach to the medial, superior, and inferior borders of the scapula. Each of these muscles has its own role in shoulder function and must be in balance with the others in order to avoid shoulder pathology.
Abnormal scapular function is called scapular dyskinesis. One action the scapula performs during a throwing or serving motion is elevation of the acromion process in order to avoid impingement of the rotator cuff tendons.[8] If the scapula fails to properly elevate the acromion, impingement may occur during the cocking and acceleration phase of an overhead activity. The two muscles most commonly inhibited during this first part of an overhead motion are the serratus anterior and the lower trapezius.[10] These two muscles act as a force couple within the glenohumeral joint to properly elevate the acromion process, and if a muscle imbalance exists, shoulder impingement may develop.
The scapula may also be misplaced if a rib deep to it is not moving correctly. Often in the case of Shoulder impingement syndrome, the scapula may be anteverted such that the shoulder on the affected side appears protracted. The ribs that may cause such an anteversion of the scapula include ribs 2–8.
Diagnosis

Impingement syndrome can be diagnosed by a targeted medical history and physical examination,[11][12] but it has also been argued that at least medical imaging[13] (generally X-ray initially) and/or response to local anesthetic injection[14] is necessary for workup. However, imaging studies are unable to show cause of shoulder pain in diagnosing. For example, MRI imaging would show rotator cuff pathology and bursitis but is unable to specify the cause.[15]
On physical exam, the physician may twist or elevate the patient's arm to test for reproducible pain (the Neer sign and Hawkins-Kennedy test). These tests help localize the pathology to the rotator cuff; however, they are not specific for impingement.[16] Neer sign may also be seen with subacromial bursitis.[17]
Response to local anesthetic
The physician may inject lidocaine (usually combined with a steroid) into the bursa, and if there is an improved range of motion and decrease in pain, this is considered a positive "Impingement Test". It not only supports the diagnosis for impingement syndrome, but it is also therapeutic.[18]
Imaging
Plain x-rays of the shoulder can be used to detect some joint pathology and variations in the bones, including acromioclavicular arthritis, variations in the acromion, and calcification. However, x-rays do not allow visualization of soft tissue and thus hold a low diagnostic value.[2] Ultrasonography, arthrography and MRI can be used to detect rotator cuff muscle pathology. MRI is the best imaging test prior to arthroscopic surgery.[2] Due to lack of understanding of the pathoaetiology, and lack of diagnostic accuracy in the assessment process by many physicians,[19] several opinions are recommended before intervention.
Treatment
Impingement syndrome is usually treated conservatively, but sometimes it is treated with arthroscopic surgery or open surgery.[20] Conservative treatment includes rest, cessation of painful activity, and physical therapy. Physical therapy treatments would typically focus at maintaining range of movement, improving posture, strengthening shoulder muscles, and reduction of pain. NSAIDs and ice packs may be used for pain relief.[4][20]
Therapeutic exercises might be favorable intervention compared to passive treatment approaches, electrotherapy and placebo. A recent meta-analysis done on rotator cuff tendinopathy has shown that nearly all types of active resistance training programs were proven to be effective in improving pain and shoulder function with no significant differences among the different exercise types, further cementing the favorability of a more active intervention over passive modalities when it comes to rotator cuff issues.[21] Exercises may help to regain the scapulo-humeral rhythm and scapular control which may reduce pain.[22]
Steroids
Therapeutic injections of corticosteroid and local anaesthetic may be used for persistent impingement syndrome.[20] The total number of injections is generally limited to three due to possible side effects from the corticosteroid.[4] A 2017 review found corticosteroid injections only give small and transient pain relief.[23]
Surgery
A number of surgical interventions are available, depending on the nature and location of the pathology. Surgery may be done arthroscopically or as open surgery. The impinging structures may be removed in surgery, and the subacromial space may be widened by resection of the distal clavicle and excision of osteophytes on the under-surface of the acromioclavicular joint.[4] Damaged rotator cuff muscles can be surgically repaired.
A 2019 review found that the evidence does not support decompression surgery in those with more than 3 months of shoulder pain without a history of trauma.[24] A recent metaanalysis has further supported that early SIS would likely benefit from non-operative treatment modalities and surgical open decompression should be considered only with chronic presentation.
History
Impingement syndrome was reported in 1852.[4] Impingement of the shoulder was previously thought to be precipitated by shoulder abduction and surgical intervention focused on lateral or total acromionectomy.[4][25] In 1972, Charles Neer proposed that impingement was due to the anterior third of the acromion and the coracoacromial ligament and suggested surgery should be focused on these areas.[4][25] The role of anteriorinferior aspect of the acromion in impingement syndrome and excision of parts of the anteriorinferior acromion has become a pivotal part of the surgical treatment of the syndrome.[4]
Criticism
Subacromial impingement is not free of criticism. First, the identification of acromion type shows poor intra- and inter-observer reliability.[26][27] Second, a computerized three-dimensional study failed to support impingement by any portion of the acromion on the rotator cuff tendons in different shoulder positions.[28] Third, most partial-thickness cuff tears do not occur on bursal surface fibers, where mechanical abrasion from the acromion does occur.[29][30] Fourth, it has been suggested that bursal surface cuff tears could be responsible for subacromial spurs and not the opposite.[31][32][33][34] Fifth, it has been shown that there is no association with acromiohumeral distance, measured at 0°, 45° and 60° of shoulder abduction, with people with subacromial pain syndrome and shoulder pain.[35] And finally, there is growing evidence that routine acromioplasty may not be required for successful rotator cuff repair, which would be an unexpected finding if acromial shape had a major role in generating tendon lesions.[36] In summary, despite being a popular theory, the bulk of evidence suggest that subacromial impingement probably does not play a dominant role in many cases of rotator cuff disease.[37]
See also
References
- ↑ Thomas M DeBerardino (17 January 2023). "Supraspinatus Tendonitis". Medscape. Updated: Dec 03, 2018
- 1 2 3 4 5 6 7 Fongemie AE, Buss DD, Rolnick SJ (February 1998). "Management of shoulder impingement syndrome and rotator cuff tears". Am Fam Physician. 57 (4): 667–74, 680–2. PMID 9490991.
- ↑ SimonMoyes.com. "What is Subacromial Impingement?". Archived from the original on 2011-08-27. Retrieved 2011-03-14.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 6 7 8 9 Chen AL, Rokito AS, Zuckerman JD (April 2003). "The role of the acromioclavicular joint in impingement syndrome". Clin Sports Med. 22 (2): 343–57. doi:10.1016/S0278-5919(03)00015-2. PMID 12825535.
- 1 2 Habermeyer, Magosch & Lichtenberg 2006, pp. 1–3
- ↑ Neer, C. S. (1983). "Impingement lesions". Clinical Orthopaedics and Related Research. 173: 70–77. doi:10.1097/00003086-198303000-00010.
- ↑ Schoenfeld, Brad; Kolber, Morey J; Haimes, Jonathan E (October 2011). "The Upright Row: Implications for Preventing Subacromial Impingement". Strength and Conditioning Journal. 33 (5): 25–28. doi:10.1519/SSC.0b013e31822ec3e3. S2CID 58333549.
- 1 2 Kibler, BW (1998). "The role of the scapula in athletic shoulder function". The American Journal of Sports Medicine. 26 (2): 325–337. doi:10.1177/03635465980260022801. PMID 9548131. S2CID 26608885.
- ↑ Marieb, E. (2005). Anatomy & Physiology (2nd ed.). San Francisco, CA: Pearson Benjamin Cummings.
- ↑ Cools, A.; Dewitte, V.; Lanszweert, F.; Notebaert, D.; Roets, A.; et al. (2007). "Rehabilitation of scapular muscle balance". The American Journal of Sports Medicine. 35 (10): 1744–51. doi:10.1177/0363546507303560. PMID 17606671. S2CID 4206849.
- ↑ Craig Hacking and Frank Gaillard (2019-03-06). "Subacromial impingement". Radiopaedia.
- ↑ "Shoulder Impingement Syndrome". Stanford University Medical Center. 2019-03-06.
- ↑ Garving, Christina; Jakob, Sascha; Bauer, Isabel; Nadjar, Rudolph; Brunner, Ulrich H. (2017). "Impingement Syndrome of the Shoulder". Deutsches Ärzteblatt Online. 114 (45): 765–776. doi:10.3238/arztebl.2017.0765. ISSN 1866-0452. PMC 5729225. PMID 29202926.
- ↑ Botser, Itamar; Hershkovich, Oded; Shapira, Shachar; Sela, Yaron (2014). "Role of radiographs in shoulder pathology: a clinical review". Reports in Medical Imaging: 75. doi:10.2147/RMI.S35587. ISSN 1179-1586.
- ↑ Dhillon, KS (November 2019). "Subacromial Impingement Syndrome of the Shoulder: A Musculoskeletal Disorder or a Medical Myth?". Malaysian Orthopaedic Journal. 13 (3): 1–7. doi:10.5704/MOJ.1911.001. ISSN 1985-2533. PMC 6915323. PMID 31890103.
- ↑ Koester MC, George MS, Kuhn JE (May 2005). "Shoulder impingement syndrome". The American Journal of Medicine. 118 (5): 452–5. doi:10.1016/j.amjmed.2005.01.040. PMID 15866244.
- ↑ Marreez, YM; Forman, MD; Brown, SR (May 2013). "Physical examination of the shoulder joint-Part I: Supraspinatus rotator cuff muscle clinical testing" (PDF). Osteopathic Family Physician. 5 (3): 128–134. doi:10.1016/j.osfp.2013.01.005.
- ↑ Oh JH, Kim SH, Kim KH, Oh CH, Gong HS (July 2010). "Modified impingement test can predict the level of pain reduction after rotator cuff repair". The American Journal of Sports Medicine. 38 (7): 1383–8. doi:10.1177/0363546509359071. PMID 20522833. S2CID 23919395.
- ↑ Lewis JS. (Oct 17, 2008). "Rotator cuff tendinopathy / subacromial impingement syndrome: Is it time for a new method of assessment?". British Journal of Sports Medicine. 43 (4): 259–64. doi:10.1136/bjsm.2008.052183. PMID 18838403.
- 1 2 3 Taheriazam A, Sadatsafavi M, Moayyeri A (2005). "Outcome predictors in nonoperative management of newly diagnosed subacromial impingement syndrome: a longitudinal study". MedGenMed. 7 (1): 63. PMC 1681371. PMID 16369368.
- ↑ Dominguez-Romero, Juan G.; Jiménez-Rejano, José J.; Ridao-Fernández, Carmen; Chamorro-Moriana, Gema (2021-03-16). "Exercise-Based Muscle Development Programmes and Their Effectiveness in the Functional Recovery of Rotator Cuff Tendinopathy: A Systematic Review". Diagnostics (Basel, Switzerland). 11 (3): 529. doi:10.3390/diagnostics11030529. ISSN 2075-4418. PMC 8002167. PMID 33809604.
- ↑ Gebremariam, Lukas; Hay, Elaine M.; van der Sande, Renske; Rinkel, Willem D.; Koes, Bart W.; Huisstede, Bionka M. A. (August 2014). "Subacromial impingement syndrome--effectiveness of physiotherapy and manual therapy". British Journal of Sports Medicine. 48 (16): 1202–1208. doi:10.1136/bjsports-2012-091802. ISSN 1473-0480. PMID 24217037. S2CID 27383041.
- ↑ Mohamadi, Amin; Chan, Jimmy J.; Claessen, Femke M. A. P.; Ring, David; Chen, Neal C. (January 2017). "Corticosteroid Injections Give Small and Transient Pain Relief in Rotator Cuff Tendinosis: A Meta-analysis". Clinical Orthopaedics and Related Research. 475 (1): 232–243. doi:10.1007/s11999-016-5002-1. ISSN 1528-1132. PMC 5174041. PMID 27469590.
- ↑ Poolman, Rudolf W.; Agoritsas, Thomas; Guyatt, Gordon; Proulx, Laurie; Fisch, Florian; Shunjie, Sean Chua; Albin, Alexandra; Siemieniuk, Reed A. C.; Lytvyn, Lyubov; Noorduyn, Julia; Bekerom, Michel van den; Karjalainen, Teemu; Hao, Qiukui; Burgers, Jako; Brox, Jens Ivar; Moro, Jaydeep; Buchbinder, Rachelle; Ardern, Clare; Lähdeoja, Tuomas; Vandvik, Per Olav (6 February 2019). "Subacromial decompression surgery for adults with shoulder pain: a clinical practice guideline". BMJ. 364: l294. doi:10.1136/bmj.l294. hdl:10138/313758. ISSN 0959-8138. PMID 30728120. S2CID 73425732.
- 1 2 Neer CS (January 1972). "Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report". J Bone Joint Surg Am. 54 (1): 41–50. doi:10.2106/00004623-197254010-00003. PMID 5054450.
- ↑ Zuckerman, JD; Kummer, FJ; Cuomo, F; Greller, M (1997). "Interobserver reliability of acromial morphology classification: an anatomic study". J Shoulder Elbow Surg. 6 (3): 286–7. doi:10.1016/s1058-2746(97)90017-3. PMID 9219133.
- ↑ Peh, WC; Farmer, TH; Totty, WG (1995). "Acromial arch shape:assessment with MR imaging". Radiology. 195 (2): 501–5. doi:10.1148/radiology.195.2.7724774. PMID 7724774.
- ↑ Chang, EY; Moses, DA; Babb, JS; Schweitzer, ME (2006). "Shoulder impingement: objective 3D shape analysis of acromial morphologic features". Radiology. 239 (2): 497–505. doi:10.1148/radiol.2392050324. PMID 16543591.
- ↑ Loehr, J; Uhthoff, H (1987). "The pathogenesis of degenerative rotator cuff tears". Orthopedic Trans. 11: 237–44.
- ↑ Ogata, S; Uhthoff, HK (1990). "Acromial enthesopathy and rotator cuff tear. A radiologic and histologic postmortem investigation of the coracoacromial arch". Clin Orthop Relat Res. 254: 39–48. doi:10.1097/00003086-199005000-00006.
- ↑ Thompson, WO; Debski, RE; Boardman, ND; et al. (1996). "A biomechanical analysis of rotator cuff deficiency in a cadaveric model". Am J Sports Med. 24 (3): 286–92. doi:10.1177/036354659602400307. PMID 8734877. S2CID 27853735.
- ↑ Chambler, AF; Pitsillides, AA; Emery, RJ (2003). "Acromial spur formation in patients with rotator cuff tears". J Shoulder Elbow Surg. 12 (4): 314–21. doi:10.1016/s1058-2746(03)00030-2. PMID 12934022.
- ↑ Sarkar, K; Taine, W; Uhthoff, HK (1990). "The ultrastructure of the coracoacromial ligament in patients with chronic impingement syndrome". Clin Orthop Relat Res. 254: 49–54. doi:10.1097/00003086-199005000-00007.
- ↑ Ozaki J, Fujimoto S, Nakagawa Y, et al. (1988). "Tears of the rotator cuff of the shoulder associated with pathological changes in the acromion. A study in cadavera". J Bone Joint Surg Am. 70 (8): 1224–30. doi:10.2106/00004623-198870080-00015. PMID 3417708.
- ↑ Park, Soo Whan; Chen, Yuan Tai; Thompson, Lindsay; Kjoenoe, Andreas; Juul-Kristensen, Birgit; Cavalheri, Vinicius; McKenna, Leanda (2020-11-26). "No relationship between the acromiohumeral distance and pain in adults with subacromial pain syndrome: a systematic review and meta-analysis". Scientific Reports. 10 (1): 20611. Bibcode:2020NatSR..1020611P. doi:10.1038/s41598-020-76704-z. ISSN 2045-2322. PMC 7693267. PMID 33244115.
- ↑ Pedowitz RA, Yamaguchi K, Ahmad CS, et al. (2012). "American Academy of Orthopaedic Surgeons Clinical Practice Guideline on optimizing the management of rotator cuff problems". J Bone Joint Surg Am. 94 (2): 163–7. doi:10.2106/jbjs.k.01368. PMID 22258004.
- ↑ Arend CF. Ultrasound of the Shoulder. Master Medical Books, 2013
The Arm Doc: https://thearmdoc.co.uk/shoulder-impingement