Lujan-Fryns綜合症
Lujan-Fryns綜合症(Lujan–Fryns syndrome、LFS)是一種X染色體伴性遺傳障礙,會導致輕度至中度智能障礙和類似於馬凡氏症候群的Marfanoid習性特徵。[4][5]特徵包括高瘦身材和修長四肢。[5]
| Lujan–Fryns syndrome Lujan-Fryns綜合症 | |
|---|---|
| 同义词 | 伴隨Marfanoid習性X染色體伴性遺傳精神發育遲滯Lujan綜合症[1][2][3] |
 | |
| 年輕成年男性,其特徵包括長而窄的臉和凹陷的下巴。 | |
| 分类和外部资源 | |
| 醫學專科 | Medical genetics |
| ICD-10 | F70.1 |
| OMIM | 309520 |
| DiseasesDB | 32654 |
綜合症與精神病理學和人類行為異常有關。綜合症還表現出許多如大腦心臟畸形的影響。[6][7][8]
歸因於MED12基因的錯義突變,該疾病以X連鎖顯性遺傳方式遺傳。[3]目前還沒有針對潛在的MED12功能障礙的治療或療法,並且該疾病的確切原因仍不清楚。[9]
體徵和症狀
智力障礙通常從輕度到中度不等,但也有嚴重病例的報導。[10][11]
相對常見的大腦異常,綜合症的是胼胝體發育不全,因胚胎發育錯誤導致不存在連接左右兩個大腦半球的胼胝體。[7][12]缺乏胼胝體會發現許多不良神經學影響,智力障礙的發生率約73%。[12]然而,尚未有綜合症胼胝體發育不全與智力障礙之間的相關性研究。[13]
精神病學
診斷該病症可能要考慮該症通常出現的精神病理學和相關行為異常。[7]
綜合症最常見的是自閉症樣譜系障礙,該綜合症被認為是與自閉症相關的遺傳障礙之一。[7][14]
Additional alterations of psychopathology with behavioral manifestations that have been observed in LFS include: psychotic behavior,[15] schizophrenia,[16] hyperactivity and attention-deficit hyperactivity disorder,[13][17] aggression,[17] oppositional defiant disorder,[13][18] obsessive compulsive disorder,[13] extreme shyness,[17] learning disability,[13] cognitive impairment,[13] short-term memory deficit,[13] low frustration tolerance,[13] social dysfunction,[13] lack of impulse control,[13] eating disorder and associated malnutrition, attributed to psychogenic loss of appetite;[6] and pyromania.[7][13][18]
While psychiatric conditions like these are to be expected with LFS, there have also been cases of the disorder with some preservation of mental and behavioral abilities, such as problem solving, reasoning and normal intelligence.[19]
The psychopathology of LFS usually exhibits schizophrenia.[16] When schizophrenia is diagnosed in an individual known to be affected by intellectual disability, LFS may be considered in the differential diagnosis of schizophrenia, with confirmation of cause through appropriate psychiatric and genetic evaluation methods.[16]
Marfanoid習性
LFS is clinically distinguished from other X-linked forms of intellectual disability by the accompanying presence of marfanoid habitus.[10] Marfanoid habitus describes a group of physical features common to Marfan syndrome.[5] Including Marfan syndrome and LFS, marfanoid features of this type have also been observed with several other disorders, one of which is multiple endocrine neoplasia type 2.[20]
In LFS, specific features identified as marfanoid include: a long, narrow face;[5][9] tall, thin stature;[3][9] long, slender limbs, fingers and toes (not unlike arachnodactyly)[3][21][22] with joint hyperextensibility,[17] shortened halluces (the big toes) and long second toes.[9]
頭臉
Craniofacial and other features of LFS include: maxillary hypoplasia (underdevelopment of the upper jaw bone),[9] a small mandible (lower jaw bone) and receding chin,[3][17] a high-arched palate (the roof of the mouth), with crowding and misalignment of the upper teeth;[5][7] macrocephaly (enlarged skull) with a prominent forehead,[3][9] hypernasal speech (voice),[5][7] a long nose with a high, narrow nasal bridge;[9] a deep, short philtrum (the indentation in the upper lip, beneath the nose),[9] low-set ears with some apparent retroversion,[9] hypotonia (decreased muscle tone),[3] pectus excavatum (a malformity of the chest),[9] slightly enlarged to normal testicular size in males,[9][17] and seizures.[9]
Hypernasal speech, or "hypernasality", is primarily the result of velopharyngeal insufficiency, a sometimes congenital aberration in which the velopharyngeal sphincter allows too much air into the nasal cavity during speech.[23][24] In LFS, hypernasality may also be caused by failure of the soft palate and uvula to reach the back wall of the pharynx (the interior cavity of the throat where swallowing generally occurs) during speech, a condition that can be associated with a submucosal cleft palate.[13][25]
心臟
A number of features involving the heart have been noted in several LFS cases, the most significant being dilation of the aortic root, a section of the ascending aorta.[8] Aortic root dilation (enlargement) is associated with a greatly increased risk of dissection of the aortic wall, resulting in aortic aneurysm.[26] As this presents a possible life-threatening consequence of LFS, routine cardiac evaluation methods such as echocardiogram are implemented when the disorder is first diagnosed, along with MRI scans of the brain to screen for suspected agenesis of the corpus callosum.[7] Additional effects on the heart that have been reported with LFS are ventricular and atrial septal defect.[8][17]
原因
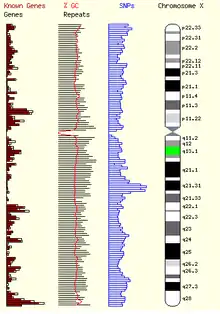
A missense mutation in the MED12 gene, located on the human X chromosome, has been established as the cause of LFS.[3][27] Missense mutations are genetic point mutations in which a single nucleotide in the genetic sequence is exchanged with another one. This leads to an erroneously substitution of a particular amino acid in the protein sequence during translation. The missense mutation in the MED12 gene, that causes LFS, is identified as p.N1007S.[3] This indicates that the amino acid asparagine, normally located at position 1007 along the MED12 sequence, has been mistakenly replaced by serine.[27] This mutation in MED12 causes incorrect expression and activity of the protein it encodes, resulting in the disorder.[3][9]
病理生理學
MED12, or mediator of RNA polymerase II transcription, subunit 12 homolog of S. cerevisiae, is one of several subunits in the mammalian mediator complex, which regulates RNA polymerase II during mRNA transcription.[28][29]
The Mediator complex is required for polymerase II transcription and acts as a bridge between the polymerase II enzyme and different gene-specific transcription factors. Mediator can contain up to 30 subunits, but some of the subunits are only required for regulation of transcription in particular tissues or cells.[30] Currently, the exact mechanism by which dysfunction of MED12 results in LFS and its associated neuropsychopathic and physical characteristics is unclear. Marfanoid habitus, a highly arched palate and several other features of LFS can be found with Marfan syndrome, a connective tissue disorder.[4] The finding of aortic root dilation in both disorders suggests that a mutation in an unspecified connective tissue regulating gene may contribute to the etiology of LFS.[1][5][8][13]
A number of interesting experimental results have been obtained by studying MED12 mutations in the zebrafish, an animal model representing vertebrates.[31][32][33] In zebrafish, a mutation in MED12 was found to be responsible for the mutant motionless (mot). Zebrafish with the mot mutation have neuronal and cardiovascular defects, although not all types of neurons are affected. Introduction of human MED12 mRNA into the zebrafish restores normal development.[34] MED12 is also a critical coactivator for the gene SOX9, which is involved in the developmental regulation of neurons, cartilage and bone. In the zebrafish, MED12 defects cause maldevelopment of vertebrate embryonic structures such as the neural crest, which would alter function of the autonomic and peripheral nervous systems; and they also cause malformations of cell types serving as precursors to cartilage and bone, such as osteocytes.[34][35][36] Some features found in LFS, like agenesis of the corpus callosum and cartilage-related craniofacial anomalies, are similar to defects found in zebrafish with MED12 and associated mutations.[3]
遺傳學
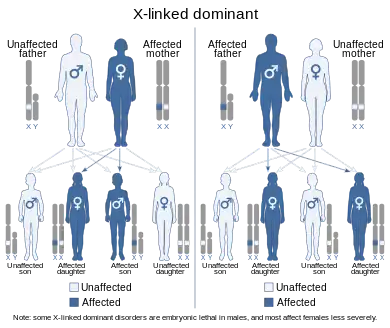
Lujan–Fryns syndrome is inherited in an X-linked dominant manner.[9][13][37] This means the defective gene responsible for the disorder (MED12) is located on the X chromosome, and only one copy of the defective gene is sufficient to cause the disorder when inherited from a parent who has the disorder. Males are normally hemizygous for the X chromosome, having only one copy. As a result, X-linked dominant disorders usually show higher expressivity in males than females. This phenomenon is thought to occur with LFS.[13][37]
As the X chromosome is one of the sex chromosomes (the other being the Y chromosome), X-linked inheritance is determined by the gender of the parent carrying a specific gene and can often seem complex. This is because, typically, females have two copies of the X-chromosome, while males have only one copy. The difference between dominant and recessive inheritance patterns also plays a role in determining the chances of a child inheriting an X-linked disorder from their parentage.
In LFS, X-linked dominant inheritance was suspected, as boy and girl siblings in one family both exhibited the disorder.[13][37] A scenario such as this would also be possible with X-linked recessive inheritance, but in this particular case report, the girl was believed to be a manifesting heterozygote[13][37] carrying one copy of the mutated gene.
Sporadic cases of LFS, where the disorder is present in an individual with no prior family history of it, have also been reported in a small number of affected males.[13][15][38]
與其他遺傳病的相似之處
An individual exhibiting intellectual disability and other symptoms similar to LFS was found to have a terminal deletion of the subtelomeric region in the short arm of chromosome 5.[25] Deletion of this area of chromosome 5 is associated with intellectual disability, psychotic behavior, autism, macrocephaly and hypernasal-like speech, as well as the disorder Cri du chat syndrome.[25][39] Fryns (2006) suggests a detailed examination of chromosome 5 with FISH should be performed as part of the differential diagnosis of LFS.[9]
Mutations in the UPF3B gene, also found on the X chromosome, are another cause of X-linked intellectual disability.[40] UPF3B is part of the nonsense-mediated mRNA decay (NMD) complex, which performs mRNA surveillance, detecting mRNA sequences that have been erroneously truncated (shortened) by the presence of nonsense mutations.[41] Mutations in UPF3B alter and prevent normal function of the NMD pathway, resulting in translation and expression of truncated mRNA sequences into malfunctioning proteins that can be associated with developmental errors and intellectual disability.[41][42] Individuals from two families diagnosed with LFS and one family with FGS were found to have mutations in UPF3B, confirming that the clinical presentations of the different mutations can overlap.[42]
診斷
Although LFS is usually suspected when intellectual disability and marfanoid habitus are observed together in a patient, the diagnosis of LFS can be confirmed by the presence of the p.N1007S missense mutation in the MED12 gene.[3][9][10]
鑑別診斷
In the differential diagnosis of LFS, another disorder that exhibits some features and symptoms of LFS and is also associated with a missense mutation of MED12 is Opitz-Kaveggia syndrome (FGS).[3][43] Common features shared by both LFS and FGS include X-linked intellectual disability, hyperactivity, macrocephaly, corpus callosum agenesis and hypotonia.[3] Notable features of FGS that have not been reported with LFS include excessive talkativeness, consistent strength in socialization skills, imperforate anus (occlusion of the anus) and ocular hypertelorism (extremely wide-set eyes).[44][45]
綜合症與錯義突變 p.N1007S 相關,而 FGS 與錯義突變 p.R961W 相關。[3][46] As both disorders originate from an identical type of mutation in the same gene, while exhibiting similar, yet distinct characteristics; LFS and FGS are considered to be allelic.[3][9][13][43] In the context of MED12, this suggests that the phenotype of each disorder is related to the way in which their respective mutations alter the MED12 sequence and its function.[3][27][43]
治療
雖然沒有針對綜合症的潛在遺傳原因特定治療方法,但在治療和管理與該疾病相關的許多顱面、骨科、精神問題時,可以考慮糾正程序、預防性干預措施和療法。更緊迫的問題,如心臟受累或癲癇發作,應進行常規檢查和監測。應給予密切關注和專門的後續護理,包括神經心理學評估方法和療法以及特殊教育,以診斷和預防精神障礙和相關的行為問題,如精神病和攻擊性爆發。[9]
流行病學
是一種罕見的 X 連鎖顯性綜合徵,男性多於女性。它在普通人群中的流行程度尚未確定。[9]
歷史
綜合症是以醫師的 J. Enrique Lujan 和 Jean-Pierre Fryns 命名的。[21] The initial observation of suspected X-linked intellectual disability with Marfanoid features and craniofacial effects such as a high-arched palate was described by Lujan et al. in 1984.[17]
In the report, four affected male members of a large kindred (consanguinous family) were noted.[3][13][17] Additional investigations of combined X-linked intellectual disability and Marfanoid habitus in other families, including two brothers, were reported by Fryns et al., beginning in 1987.[5] The disorder soon became known as Lujan–Fryns syndrome.[37]
参见
- Fragile X syndrome
- Aarskog syndrome
- Coffin–Lowry syndrome
- FG syndrome
參考
- Lacombe, D.; Bonneau, D.; Verloes, A.; Couet, D.; Koulischer, L.; Battin, J. . Genetic Counseling (Geneva, Switzerland). 1993, 4 (3): 193–198. ISSN 1015-8146. PMID 8267926.
- Fryns, J. P.; Van Den Berghe, H. . Genetic Counseling (Geneva, Switzerland). 1991, 2 (4): 241–244. ISSN 1015-8146. PMID 1799424.
- Schwartz, C. E.; Tarpey, P. S.; Lubs, H. A.; Verloes, A.; May, M. M.; Risheg, H.; Friez, M. J.; Futreal, P. A.; Edkins, S.; Teague, J.; Briault, S.; Skinner, C.; Bauer-Carlin, A.; Simensen, R. J.; Joseph, S. M.; Jones, J. R.; Gecz, J.; Stratton, M. R.; Raymond, F. L.; Stevenson, R. E. . Journal of Medical Genetics. July 2007, 44 (7): 472–477. ISSN 0022-2593. PMC 2597996
 . PMID 17369503. doi:10.1136/jmg.2006.048637.
. PMID 17369503. doi:10.1136/jmg.2006.048637. - OMIM 154700
- Fryns, J. P.; Buttiens, M.; Opitz, J. M.; Reynolds, J. F. . American Journal of Medical Genetics. Oct 1987, 28 (2): 267–274. ISSN 0148-7299. PMID 3322000. doi:10.1002/ajmg.1320280202.
- Alonso, P.; Pintos, G.; Almazan, F.; Hernández, L.; Loran, E.; Menchon, J. M.; Vallejo, J. . Clinical Dysmorphology. July 2006, 15 (3): 181–184. ISSN 0962-8827. PMID 16760741. S2CID 7415391. doi:10.1097/01.mcd.0000220610.24908.a4.
- Lerma‐Carrillo, I.; Molina, J. D.; Cuevas-Duran, T.; Julve-Correcher, C.; Espejo-Saavedra, J. M.; Andrade-Rosa, C.; Lopez-Muñoz, F. . American Journal of Medical Genetics Part A. December 2006, 140 (24): 2807–2811. ISSN 1552-4825. PMID 17036352. S2CID 22491132. doi:10.1002/ajmg.a.31503.
- Wittine, L. M.; Josephson, K. D.; Williams, M. S. . American Journal of Medical Genetics. Oct 1999, 86 (5): 405–409. ISSN 0148-7299. PMID 10508979. doi:10.1002/(SICI)1096-8628(19991029)86:5<405::AID-AJMG2>3.0.CO;2-1.
- Buggenhout, G. V.; Fryns, J. -P. . Orphanet Journal of Rare Diseases (Free full text). July 2006, 1: 26. PMC 1538574
 . PMID 16831221. doi:10.1186/1750-1172-1-26.
. PMID 16831221. doi:10.1186/1750-1172-1-26. - Fryns, J. P.; Buttiens, M.; Van Den Berghe, H. . Journal de Génétique Humaine. Jan 1988, 36 (1–2): 123–128. ISSN 0021-7743. PMID 3379374.
- Mégarbané A, C. C.; Chammas, C. . Genetic Counseling (Geneva, Switzerland). 1997, 8 (3): 195–200. ISSN 1015-8146. PMID 9327261.
- Jeret, J. S.; Serur, D.; Wisniewski, K. E.; Lubin, R. A. . Brain & Development. 1987, 9 (3): 255–264. ISSN 0387-7604. PMID 3310713. S2CID 4761497. doi:10.1016/s0387-7604(87)80042-6.
- OMIM 309520
- Artigas-Pallarés, J.; Gabau-Vila, E.; Guitart-Feliubadaló, M. . Revista de Neurología. Jan 2005,. 40 Suppl 1: S151–S162. ISSN 0210-0010. PMID 15736079. doi:10.33588/rn.40S01.2005073.
- Lalatta, F.; Livini, E.; Selicorni, A.; Briscioli, V.; Vita, A.; Lugo, F.; Zollino, M.; Gurrieri, F.; Neri, G. . American Journal of Medical Genetics. Feb 1991, 38 (2–3): 228–232. ISSN 0148-7299. PMID 2018063. doi:10.1002/ajmg.1320380211.
- De Hert, M.; Steemans, D.; Theys, P.; Fryns, J. P.; Peuskens, J. . American Journal of Medical Genetics. Apr 1996, 67 (2): 212–213. PMID 8723050. doi:10.1002/(SICI)1096-8628(19960409)67:2<212::AID-AJMG13>3.0.CO;2-M.
- Lujan, J. E.; Carlin, M. E.; Lubs, H. A.; Opitz, J. M. . American Journal of Medical Genetics. Jan 1984, 17 (1): 311–322. ISSN 0148-7299. PMID 6711603. doi:10.1002/ajmg.1320170124.
- Williams, M. S. . American Journal of Medical Genetics Part A. Dec 2006, 140 (24): 2812–2815. ISSN 1552-4825. PMID 17103446. S2CID 29096814. doi:10.1002/ajmg.a.31501.
- Donders, J.; Toriello, H.; Van Doornik, S. . American Journal of Medical Genetics. Jan 2002, 107 (3): 243–246. ISSN 0148-7299. PMID 11807907. doi:10.1002/ajmg.10144.
- Prabhu, M.; Khouzam, R. N.; Insel, J. . Southern Medical Journal. Nov 2004, 97 (11): 1130–1132. ISSN 0038-4348. PMID 15586612. S2CID 27428744. doi:10.1097/01.SMJ.0000140873.29381.12.
- synd/3838 - Who Named It?
- Buntinx, I. M.; Willems, P. J.; Spitaels, S. E.; Van Reempst, P. J.; De Paepe, A. M.; Dumon, J. E. . Journal of Medical Genetics. April 1991, 28 (4): 267–273. ISSN 0022-2593. PMC 1016831
 . PMID 1856834. doi:10.1136/jmg.28.4.267.
. PMID 1856834. doi:10.1136/jmg.28.4.267. - Willging, J. P. . International Journal of Pediatric Otorhinolaryngology. Oct 1999,. 49 Suppl 1: S307–S309. ISSN 0165-5876. PMID 10577827. doi:10.1016/S0165-5876(99)00182-2.
- Warren, D. W.; Dalston, R. M.; Mayo, R. . The Cleft Palate-Craniofacial Journal. Jul 1994, 31 (4): 257–262. ISSN 1055-6656. PMID 7918520. doi:10.1597/1545-1569(1994)031<0257:HAVI>2.3.CO;2.
- Stathopulu, E.; Ogilvie, C. M.; Flinter, F. A. . American Journal of Medical Genetics Part A. June 2003, 119A (3): 363–366. ISSN 1552-4825. PMID 12784307. S2CID 45722356. doi:10.1002/ajmg.a.10268.
- Gambarin, F.; Favalli, V.; Serio, A.; Regazzi, M.; Pasotti, M.; Klersy, C.; Dore, R.; Mannarino, S.; Viganò, M.; Odero, A.; Amato, S.; Tavazzi, L.; Arbustini, E. . Journal of Cardiovascular Medicine (Hagerstown, Md.). April 2009, 10 (4): 354–362. ISSN 1558-2027. PMID 19430350. S2CID 29419873. doi:10.2459/JCM.0b013e3283232a45.
- OMIM 300188
- Biddick, R.; Young, E. . Comptes Rendus Biologies. Sep 2005, 328 (9): 773–782. ISSN 1631-0691. PMID 16168358. doi:10.1016/j.crvi.2005.03.004.
- Sims, R. J. 3rd; Mandal, S. S.; Reinberg, D. . Current Opinion in Cell Biology. June 2004, 16 (3): 263–271. ISSN 0955-0674. PMID 15145350. doi:10.1016/j.ceb.2004.04.004.
- Malik, S.; Roeder, R. G. . Trends in Biochemical Sciences. Jun 2000, 25 (6): 277–283. ISSN 0968-0004. PMID 10838567. doi:10.1016/S0968-0004(00)01596-6.
- Chakraborty C, H. C.; Hsu, C. H.; Wen, Z. H.; Lin, C. S.; Agoramoorthy, G. . Current Drug Metabolism. Feb 2009, 10 (2): 116–124. ISSN 1389-2002. PMID 19275547. doi:10.2174/138920009787522197.
- Kari, G.; Rodeck, U.; Dicker, A. P. . Clinical Pharmacology and Therapeutics. July 2007, 82 (1): 70–80. ISSN 0009-9236. PMID 17495877. S2CID 41443542. doi:10.1038/sj.clpt.6100223.
- McGonnell, I. M.; Fowkes, R. C. (Free full text). The Journal of Endocrinology. June 2006, 189 (3): 425–439 [2022-12-28]. ISSN 0022-0795. PMID 16731775. doi:10.1677/joe.1.06683
 . (原始内容存档于2019-12-15).
. (原始内容存档于2019-12-15). - Wang, X.; Yang, N.; Uno, E.; Roeder, R. G.; Guo, S. . Proceedings of the National Academy of Sciences of the United States of America (Free full text). November 2006, 103 (46): 17284–17289. Bibcode:2006PNAS..10317284W. ISSN 0027-8424. PMC 1859923
 . PMID 17088561. doi:10.1073/pnas.0605414103
. PMID 17088561. doi:10.1073/pnas.0605414103  .
. - Rau, M. J.; Fischer, S.; Neumann, C. J. . Developmental Biology. Aug 2006, 296 (1): 83–93. ISSN 0012-1606. PMID 16712834. doi:10.1016/j.ydbio.2006.04.437
 .
. - Hong, S. -K.; Haldin, C. E.; Lawson, N. D.; Weinstein, B. M.; Dawid, I. B.; Hukriede, N. A. . Proceedings of the National Academy of Sciences of the United States of America. December 2005, 102 (51): 18473–18478. Bibcode:2005PNAS..10218473H. ISSN 0027-8424. PMC 1311743
 . PMID 16344459. doi:10.1073/pnas.0509457102
. PMID 16344459. doi:10.1073/pnas.0509457102  .
. - Gurrieri, F.; Neri, G. . American Journal of Medical Genetics. Feb 1991, 38 (2–3): 290–291. ISSN 0148-7299. PMID 2018074. doi:10.1002/ajmg.1320380225.
- Fryns, J. P. . American Journal of Medical Genetics. Feb 1991, 38 (2–3): 233. ISSN 0148-7299. PMID 2018064. doi:10.1002/ajmg.1320380212.
- Fang, J. S.; Lee, K. F.; Huang, C. T.; Syu, C. L.; Yang, K. J.; Wang, L. H.; Liao, D. L.; Chen, C. H. . Clinical Genetics. Jun 2008, 73 (6): 585–590. ISSN 0009-9163. PMID 18400035. S2CID 6209765. doi:10.1111/j.1399-0004.2008.00995.x.
- OMIM 300298
- Chang, Y. F.; Imam, J. S.; Wilkinson, M. F. . Annual Review of Biochemistry. 2007, 76: 51–74. ISSN 0066-4154. PMID 17352659. doi:10.1146/annurev.biochem.76.050106.093909.
- Tarpey, P. S.; Raymond, F. L.; Nguyen, L. S.; Rodriguez, J.; Hackett, A.; Vandeleur, L.; Smith, R.; Shoubridge, C.; Edkins, S.; Stevens, C.; O'Meara, S.; Tofts, C.; Barthorpe, S.; Buck, G.; Cole, J.; Halliday, K.; Hills, K.; Jones, D.; Mironenko, T.; Perry, J.; Varian, J.; West, S.; Widaa, S.; Teague, J.; Dicks, E.; Butler, A.; Menzies, A.; Richardson, D.; Jenkinson, A.; Shepherd, R. . Nature Genetics (Free full text). September 2007, 39 (9): 1127–1133. ISSN 1061-4036. PMC 2872770
 . PMID 17704778. doi:10.1038/ng2100.
. PMID 17704778. doi:10.1038/ng2100. - OMIM 305450
- Graham, J. M.; Superneau, D.; Rogers, R. C.; Corning, K.; Schwartz, C. E.; Dykens, E. M. . American Journal of Medical Genetics. 1999, 85 (5): 470–475. PMID 10405444. doi:10.1002/(SICI)1096-8628(19990827)85:5<470::AID-AJMG7>3.0.CO;2-S.
- Graham, J. M. Jr.; Visootsak, J.; Dykens, E.; Huddleston, L.; Clark, R. D.; Jones, K. L.; Moeschler, J. B..; Opitz, J. M..; Morford, J.; Simensen, R.; Rogers, R. C.; Schwartz, C. E.; Friez, M. J.; Stevenson, R. E. . American Journal of Medical Genetics Part A. December 2008, 146A (23): 3011–3017. ISSN 1552-4825. PMC 3092600
 . PMID 18973276. doi:10.1002/ajmg.a.32553.
. PMID 18973276. doi:10.1002/ajmg.a.32553. - Risheg, H.; Graham, J. M.; Clark, R. D.; Rogers, R. C.; Opitz, J. M.; Moeschler, J. B.; Peiffer, A. P.; May, M.; Joseph, S. M.; Jones, J. R.; Stevenson, R. E.; Schwartz, C. E.; Friez, M. J. . Nature Genetics. April 2007, 39 (4): 451–453 [2022-12-28]. ISSN 1061-4036. PMID 17334363. S2CID 26858160. doi:10.1038/ng1992. (原始内容存档于2022-01-11).
延伸閱讀
- GeneReview/NIH/UW entry on MED12-Related Disorders (页面存档备份,存于)
- Van Buggenhout, G. J. C. M.; Trommelen, J. C. M.; Brunner, H. G.; Hamel, B. C. J.; Fryns, J. P. . Annales de Génétique. Jan 2001, 44 (1): 47–55. ISSN 0003-3995. PMID 11334618. doi:10.1016/S0003-3995(01)01038-3.