| Skin tag | |
|---|---|
| Other names | Acrochordon, acrochorda, skin polyp, fibroepithelial polyp,[1] fibrovascular papilloma, soft fibroma, fibroma molle |
 | |
| Several acrochorda in the skin of the lower neck, soft consistency, the bottom acrochordon taking a pedunculated shape | |
| Specialty | Dermatology |
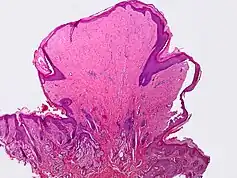
A skin tag, or acrochordon (pl.: acrochorda), is a small benign tumor that forms primarily in areas where the skin forms creases (or rubs together), such as the neck, armpit and groin. They may also occur on the face, usually on the eyelids. Though tags up to half an inch (12.7 mm) long have been seen,[2] they are typically the size of a grain of rice. The surface of an acrochordon may be smooth or irregular in appearance and is often raised from the surface of the skin on a fleshy stalk called a peduncle. Microscopically, an acrochordon consists of a fibrovascular core, sometimes also with fat cells, covered by an unremarkable epidermis. However, tags may become irritated by shaving, clothing, jewellery, or eczema.
Etiology
Skin tags are thought to occur from skin rubbing against skin, since they are so often found in skin creases and folds.[2] Studies have shown existence of low-risk human papillomaviruses 6 and 11 in skin tags, hinting at a possible role in their pathogenesis,[3] although a 2012 study found no association between skin tags and either low- or high-risk HPV.[4] Acrochorda have been reported to have a prevalence of 46% in the general population.[5] A causal genetic component is thought to exist.[6] They are also more common in women than in men. Acrochorda were once thought to be associated with colorectal polyps, but studies have shown no such connection exists.[7] Rarely, they can be associated with Birt–Hogg–Dubé syndrome, acromegaly, or polycystic ovary syndrome.[8]
Elevated blood sugar and insulin is linked to an increased incidence of skin tags through an unknown mechanism.[9]
Treatment
Removal, if desired or warranted, can be done by a dermatologist, a general practitioner, or a similarly trained professional who may use cauterization, cryosurgery, excision, laser, or surgical ligation to remove the acrochorda.[2][10] Varied home remedies are also available, but most are unproven and some (e.g. tea tree oil) may cause allergic skin reactions.[10]
See also
- Molluscum contagiosum (a viral disease which is similar in appearance and grows in similar areas)
- List of cutaneous neoplasms associated with systemic syndromes
- Papilloma
- Cutaneous horn
References
- ↑ Edwards L, Lynch PJ (2010). Genital Dermatology Atlas. Lippincott Williams & Wilkins. p. 209. ISBN 9781608310791.
- 1 2 3 "Cutaneous skin tag". Medline Plus. Retrieved 20 August 2012.
- ↑ Gupta S, Aggarwal R, Gupta S, Arora SK (2008). "Human papillomavirus and skin tags: Is there any association?". Indian J Dermatol Venereol Leprol. 74 (3): 222–5. doi:10.4103/0378-6323.39585. hdl:1807/48117. PMID 18583787.
- ↑ Pezeshkpoor F, Jafarian AH, Ghazvini K, Yazdanpanah MJ, Sadeghian A, Esmaili H, Karrabi M, Rohani F, Joushan B (May 2012). "An association of human papillomaviruses low risk and high risk subtypes with skin tag". Iranian Journal of Basic Medical Sciences. 15 (3): 840–4. PMC 3586892. PMID 23493098.
- ↑ Schwartz RA. "Acrochordon". Medscape Reference. Retrieved 20 August 2012.
- ↑ "Acrochordons - Symptoms & Treatment". Womens-health-beauty.com. Archived from the original on 29 November 2011. Retrieved 28 November 2011.
- ↑ Brendler; et al. (June 1989). "Skin tags are not a risk factor for colorectal polyps". Journal of Clinical Gastroenterology. 11 (3): 299–302. doi:10.1097/00004836-198906000-00011. PMID 2754216. S2CID 39346487.
- ↑ "Acrochordon (Skin Tag, Fibroepithelial Polyp)". Thedoctorsdoctor.com. 1 December 2008. Retrieved 28 November 2011.
- ↑ Tamega A, Aranha AM, Guiotoku MM, Miot LD, Miot HA (1 January 2010). "[Association between skin tags and insulin resistance]". Anais Brasileiros de Dermatologia. 85 (1): 25–31. doi:10.1590/S0365-05962010000100003. hdl:11449/11731. PMID 20464083.
- 1 2 "Skin tag removal: Optional but effective". Harvard Medical School. 23 March 2020. Retrieved 13 November 2021.