| Bordetella pertussis | |
|---|---|
 | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Betaproteobacteria |
| Order: | Burkholderiales |
| Family: | Alcaligenaceae |
| Genus: | Bordetella |
| Species: | B. pertussis |
| Binomial name | |
| Bordetella pertussis (Bergey et al. 1923) Moreno-López 1952 | |
Bordetella pertussis is a Gram-negative, aerobic, pathogenic, encapsulated coccobacillus of the genus Bordetella, and the causative agent of pertussis or whooping cough. Like B. bronchiseptica, B. pertussis can express a flagellum-like structure, even if it has been historically categorized as a nonmotile bacteria.[1] Its virulence factors include pertussis toxin, adenylate cyclase toxin, filamentous hæmagglutinin, pertactin, fimbria, and tracheal cytotoxin.
The bacterium is spread by airborne droplets; its incubation period is 7–10 days on average (range 6–20 days).[2][3] Humans are the only known reservoir for B. pertussis.[4] The complete B. pertussis genome of 4,086,186 base pairs was published in 2003.[5] Compared to its closest relative B. bronchiseptica, the genome size is greatly reduced. This is mainly due to the adaptation to one host species (human) and the loss of capability of survival outside a host body.[6]
History
The disease pertussis was first described by French physician Guillaume de Baillou after the epidemic of 1578. The causative agent of pertussis was identified and isolated by Jules Bordet and Octave Gengou in 1906.[7][8] B. pertussis was found closely related to Bordetella bronchiseptica and Bordetella parapertussis.[9] Developments in genome sequencing allowed B. pertussis to be studied more. Evidence of mutations through studying the gene showed missing genomes present on the DNA strand.[9] A study by Bart et al., revealed that 25% of the genes on the Tohama I reference strain of B. pertussis sequence were missing in comparison to the ancestral strains.[10]
Taxonomy
The genus Bordetella contains nine species: B. pertussis, B. parapertussis, B. bronchiseptica, B. avium, B. hinzii, B. holmesii, B. trematum, B. ansorpii, and B. petrii.[6]
B. pertussis, B. parapertussis and B. bronchiseptica form a closely related phylogenetical group. B. parapertussis causes a disease similar to whooping cough in humans, and B. bronchiseptica infects a range of mammal hosts, including humans, and causes a spectrum of respiratory disorders.[6]
Evolution
It is believed that the genus Bordetella may have evolved from ancestors that could survive in the soil according to 16S rRNA gene sequencing data.[11] 16S rRNA is a component of all bacteria that allows for the comparison of phyla within a sample. In this case, it was determined that although pathogenic Bordetella, like B. pertussis, have adapted to specifically infect humans, they are still able to multiply and thrive in soil conditions.[11] Genes controlled by the BvgAS system have transformed B. pertussis into a much more contagious pathogen [12] and are responsible for regulating the genes expressed by B. pertussis that can influence metabolic processes within the pathogen.[12]
Pertussis
Pertussis is an infection of the respiratory system characterized by a “whooping” sound when the person breathes in.[13] In the US, it killed between 10,000 and 20,000 people per year before a vaccine was available. Vaccination has transformed this; between 1985 and 1988, fewer than 100 children died from pertussis. Worldwide in 2000, according to the WHO, around 39 million people were infected annually and about 297,000 died. Since the introduction of vaccination in England in 1957, the rate of pertussis infection has dropped by 97%.[14]
B. pertussis infects its host by colonizing lung epithelial cells. The bacterium contains a surface protein, filamentous haemagglutinin adhesin, which binds to the sulfatides found on cilia of epithelial cells. Other adhesins are fimbriae and petractin.[6] Once anchored, the bacterium produces tracheal cytotoxin, which stops the cilia from beating. This prevents the cilia from clearing debris from the lungs, so the body responds by sending the host into a coughing fit. These coughs expel some bacteria into the air, which can then infect other hosts.
B. pertussis has the ability to inhibit the function of the host's immune system. The toxin, known as pertussis toxin, inhibits G protein coupling that regulates an adenylate cyclase-mediated conversion of ATP to cyclic adenosine monophosphate. The result is that phagocytes convert too much adenosine triphosphate to cyclic adenosine monophosphate, causing disturbances in cellular signaling mechanisms, and preventing phagocytes from correctly responding to the infection. Pertussis toxin, formerly known as lymphocytosis-promoting factor, causes a decrease in the entry of lymphocytes into lymph nodes, which can lead to a condition known as lymphocytosis, with a complete lymphocyte count of over 4000/μl in adults or over 8000/μl in children. Beside targeting lymphocytes, it limits neutrophil migration to the lungs. It also decreases the function of tissue-resident macrophages, which are responsible for some bacterial clearance.[15]
Another toxin that inhibits the immune response is the adenylate cyclase toxin. This toxin has an intrinsic adenylate cyclase activity, increasing intracellular cAMP almost immediately. It is also able to form cation-specific pores in the membrane of the target cell.[6][16] The resulting deregulation of cell signaling leads to the blocking of phagocytosis and reduction in the ability of neutrophils to kill bacteria. It also inhibits the maturation of dendritic cells and their migration to the lymph nodes.[15]
The infection occurs mostly in children under the age of one when they are unimmunized, or children with faded immunity, normally around the ages 11 through 18. The signs and symptoms are similar to a common cold: runny nose, sneezing, mild cough, and low-grade fever.[4] The patient becomes most contagious during the catarrhal stage of infection, normally two weeks after the coughing begins. It may become airborne when the person coughs, sneezes, or laughs. The paroxysmal cough precedes a crowing inspiratory sound characteristic of pertussis. After a spell, the patient might make a “whooping” sound when breathing in, or may vomit. Transmission rates are expected to rise as the host experiences their most contagious stage when the total viable count of B. pertussis is at its highest. After the host coughs, the bacteria in their respiratory airways will be exposed into the air by way of aerosolized droplets, threatening nearby humans.[17]
A human host can exhibit a range of physical reactions as a result of the B. pertussis pathogen, depending on how well their body is equipped to fight infection.[17] Adults have milder symptoms, such as prolonged coughing without the “whoop”. Infants less than six months also may not have the typical whoop. A coughing spell may last a minute or more, producing cyanosis, apnoea, and seizures. When not in a coughing fit, the patient does not experience trouble breathing. This is because B. pertussis inhibits the immune response, so very little mucus is generated in the lungs.
A prolonged cough may be irritating and sometimes a disabling cough may go undiagnosed in adults for many months.
Transmission
Pertussis is a highly contagious infection of the respiratory tract but for B. pertussis to persist in a population the bacterium needs an uninterrupted chain of transmission as there are no animal reservoirs and the bacteria do not survive in the environment.[18]
The incapacity for B. pertussis to live within amoeba has led to its classification as an extracellular pathogen.[12] Although B. pertussis is considered an extracellular pathogen, the evolution of human population density and gene modification has contributed to its ability to survive within respiratory epithelial and phagocytic cells.[19]
Prevention
Pertussis vaccine has been widely used since the second half of the 20th century.[9][3] The first vaccines were whole-cell vaccines, composed of chemically inactivated bacteria. They are being replaced by acellular vaccines which have, recently, shown a decreased time of immunity.[20] These acellular vaccines are composed of purified surface antigens, mainly fimbriae, filamentous haemagglutinin, pertactin and pertussis toxin. It is part of the diphtheria, tetanus, and acellular pertussis (DTaP) immunization.[3] Those being administered these vaccines are recommended to receive boosters as they are only afford protection for about 6 years. Cases in infants are common and often have serious impacts as they are more susceptible to Bordetella pertussis. Therefore, to decrease likelihood of contracting and spreading this disease, new parents may be recommended to receive the preventative vaccine.[21]
Mistakes in DTaP vaccine causing increased susceptibility
In the 20th century two articles published by Margaret Pittman, who lead pertussis research in the NIH and FDA, suggested that pertussis was a pertussis toxin mediated disease. From this research the idea came forth that, because of its toxin mediated origin, a less reactogenic acellular vaccine could be produced. The goal was that its effect on the bacterium would be just as potent as previous vaccines produced, like the whole-cell pertussis vaccine (DTwP) made available in the 1930s. Japan was then the first nation to produce a less reactogenic vaccine to target pertussis: the diphtheria, tetanus pertussis vaccine (DTaP). The DTaP vaccine was tested for its efficacy in the 1990s and approved for its use in many nations including the United States. Since this approval for routine use in the U.S., several pertussis epidemics have occurred within the last 13 years. Studies done regarding these epidemics have consistently addressed the cause of these epidemics to be due to the shortcomings the DTaP vaccine held such as the inadequate amount of antigens present in the vaccine as well as the type of cellular immune response it produced. Now, we see that the children who received the DTaP vaccine have increased vulnerability to pertussis infection for the remainder of their life.[22]
As a zoonotic disease
Uncertainties of B. pertussis and whooping cough as a zoonotic disease have existed since around 1910,[23][24] but in the 1930s, the bacteria were found to have lost their virulent power when repeatedly spread on agar media. This explained the difficulties in reproducing results from different studies, as the preinoculation handling of the bacteria was not standardized among scientists.[25]
At least some primate species are highly sensitive to B. pertussis, and develop a clinical whooping cough in high incidence when exposed to low inoculation doses.[26][27] Whether the bacteria spread naturally in wild animal populations has not been confirmed satisfactorily by laboratory diagnosis, but whooping cough has been found among wild gorillas.[28] Several zoos have learned to vaccinate their primates against whooping cough.[29]
Diagnosis
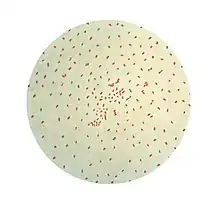
A nasopharyngeal or an oropharynx swab is sent to the bacteriology laboratory for Gram stain (Gram-negative, coccobacilli, diplococci arrangement), growth on Bordet–Gengou agar or buffered charcoal yeast extract agar with added cephalosporin to select for the organism, which shows mercury drop-like colonies. B. pertussis can also be detected by polymerase chain reaction, which is more sensitive than culture. The primers used for PCR usually target the transposable elements IS481 and IS1001.[30]
Several diagnostic tests are available, especially ELISA kits. These are designed to detect filamentous haemaggutinin and/or anti-pertussis-toxin antibodies of immunoglobulin G, immunoglobulin A, or immunoglobulin M. Some kits use a combination of antigens which lead to a higher sensitivity, but might also make the interpretation of the results harder, since one cannot know which antibody has been detected.
The organism is oxidase positive, but urease, nitrate reductase, and citrate negative. It is also motile.
Treatment
Whooping cough is treated by macrolides, for example erythromycin. The therapy is most effective when started during the incubation period or the catarrhal period. When applied during the paroxysmal cough phase, the time of reconvalescence is not affected, only further transmission is reduced to 5–10 days after infection.[3][31]
References
- ↑ Hoffman CL, Gonyar LA, Zacca F, Sisti F, Fernandez J, Wong T, et al. (May 2019). "Bordetella pertussis Can Be Motile and Express Flagellum-Like Structures". mBio. 10 (3): e00787–19. doi:10.1128/mBio.00787-19. PMC 6520453. PMID 31088927.
- ↑ Heymann DL, ed. (2008). Pertussis; in Control of Communicable Diseases Manual (19th ed.). Washington DC: American Public Health Association. p. 457. ISBN 978-0-87553-189-2.
- 1 2 3 4 Organisation mondiale de la santé; World Health Organization (1998). Relevé épidémiologique hebdomadaire (Online) = Weekly epidemiological record. Organisation mondiale de la sante. OCLC 301147153.
- 1 2 Havers FP, Moro PL, Hariri S, Skoff T (2015). "Pertussis". In Atkinson W, Wolfe S, Hamborsky J (eds.). Epidemiology and Prevention of Vaccine-Preventable Diseases: The Pink Book (13th ed.). Centers for Disease Control and Prevention, Public Health Foundation.
- ↑ Parkhill J, Sebaihia M, Preston A, Murphy LD, Thomson N, Harris DE, et al. (September 2003). "Comparative analysis of the genome sequences of Bordetella pertussis, Bordetella parapertussis and Bordetella bronchiseptica". Nature Genetics. 35 (1): 32–40. doi:10.1038/ng1227. PMID 12910271.
- 1 2 3 4 5 Locht C (2007). Bordetella: molecular microbiology. Wymondham: Horizon Bioscience. ISBN 9781904933311. OCLC 159579443.
- ↑ Rosenberg E, DeLong EF, Lory S, Stackebrandt E, Thompson F, eds. (2013). The Prokaryotes. Berlin, Heidelberg: Springer Berlin Heidelberg. doi:10.1007/978-3-642-30144-5. ISBN 9783642301438. S2CID 43556050.
- ↑ Guilfoile P (2010). Whooping Cough. Infobase Publishing. ISBN 9781604132298.
- 1 2 3 Sealey KL, Belcher T, Preston A (June 2016). "Bordetella pertussis epidemiology and evolution in the light of pertussis resurgence". Infection, Genetics and Evolution. 40: 136–143. doi:10.1016/j.meegid.2016.02.032. PMID 26932577.
- ↑ Bart MJ, Harris SR, Advani A, Arakawa Y, Bottero D, Bouchez V, et al. (April 2014). "Global population structure and evolution of Bordetella pertussis and their relationship with vaccination". mBio. 5 (2): e01074. doi:10.1128/mbio.01074-14. PMC 3994516. PMID 24757216.
- 1 2 Hamidou Soumana I, Linz B, Harvill ET (2017). "Environmental Origin of the Genus Bordetella". Frontiers in Microbiology. 8: 28. doi:10.3389/fmicb.2017.00028. PMC 5258731. PMID 28174558.
- 1 2 3 Belcher T, Dubois V, Rivera-Millot A, Locht C, Jacob-Dubuisson F (December 2021). "Pathogenicity and virulence of Bordetella pertussis and its adaptation to its strictly human host". Virulence. 12 (1): 2608–2632. doi:10.1080/21505594.2021.1980987. PMC 8489951. PMID 34590541.
- ↑ Lv Z, Yin S, Jiang K, Wang W, Luan Y, Wu S, et al. (May 2023). "The whole-cell proteome shows the characteristics of macrolides-resistant Bordetella pertussis in China linked to the biofilm formation". Archives of Microbiology. 205 (6): 219. doi:10.1007/s00203-023-03566-0. PMC 10164027. PMID 37148370.
- ↑ Lindsay P, Bagness C, Peate I (2018-02-16). Midwifery Skills at a Glance. John Wiley & Sons. ISBN 9781119233985.
- 1 2 Carbonetti NH (June 2007). "Immunomodulation in the pathogenesis of Bordetella pertussis infection and disease". Current Opinion in Pharmacology. Respiratory/Musculoskeletal. 7 (3): 272–278. doi:10.1016/j.coph.2006.12.004. PMID 17418639.
- ↑ Sebo P, Osicka R, Masin J (October 2014). "Adenylate cyclase toxin-hemolysin relevance for pertussis vaccines". Expert Review of Vaccines. 13 (10): 1215–1227. doi:10.1586/14760584.2014.944900. PMID 25090574. S2CID 27038032.
- 1 2 Warfel JM, Beren J, Merkel TJ (September 2012). "Airborne transmission of Bordetella pertussis". The Journal of Infectious Diseases. 206 (6): 902–906. doi:10.1093/infdis/jis443. PMC 3501154. PMID 22807521.
- ↑ Trainor EA, Nicholson TL, Merkel TJ (November 2015). "Bordetella pertussis transmission". Pathogens and Disease. 73 (8): ftv068. doi:10.1093/femspd/ftv068. PMC 4626651. PMID 26374235.
- ↑ Lamberti Y (December 2013). "Bordetella pertussis entry into respiratory epithelial cells and intracellular survival". academic.oup.com. Retrieved 2023-10-24.
- ↑ Carbonetti NH (June 2016). "Bordetella pertussis: new concepts in pathogenesis and treatment". Current Opinion in Infectious Diseases. 29 (3): 287–294. doi:10.1097/QCO.0000000000000264. PMC 4846492. PMID 26906206.
- ↑ Wang J, Gao J, Fan H, Guo H, Yin Z, Dong M, Huang X (April 2023). "Multiple rib and vertebral fractures associated with Bordetella pertussis infection: a case report". BMC Infectious Diseases. 23 (1): 212. doi:10.1186/s12879-023-08189-w. PMC 10080936. PMID 37024849.
- ↑ "The 112-Year Odyssey of Pertussis and Pertussis Vaccines—Mistakes Made and Implications for the Future". academic.oup.com. doi:10.1093/jpids/piz005. Retrieved 2023-12-10.
- ↑ Inaba I (1912). "Über den Bordet-Gengouschen Keuchhustenbacillus Übertragungsversuches des Keuchenhustens auf Tiere". Zeitschrift für Kinderheilkunde. 4 (1): 252–264. doi:10.1007/BF02088879. S2CID 42345587.
- ↑ Bachamn W, Burghard E (1925). "Der Nachweis der Bordet–Gengouschen Bacillen und ihre ätiologische Bedeutung für den Keuchenhusten". Zeitschrift für Kinderheilkunde. 39 (5): 465–483. doi:10.1007/BF02225286. S2CID 30221200.
- ↑ Shibley GS, Hoelscher H (September 1934). "Studies on whooping cough. I. Type-specific (S) and dissociation (R) forms of Hemophilus pertussis". The Journal of Experimental Medicine. 60 (4): 403–418. doi:10.1084/jem.60.4.403. PMC 2132401. PMID 19870311.
- ↑ Gustavsson OE, Röken BO, Serrander R (1990). "An epizootic of whooping cough among chimpanzees in a zoo". Folia Primatologica; International Journal of Primatology. 55 (1): 45–50. doi:10.1159/000156498. PMID 2394416.
- ↑ Warfel JM, Merkel TJ (October 2014). "The baboon model of pertussis: effective use and lessons for pertussis vaccines". Expert Review of Vaccines. 13 (10): 1241–1252. doi:10.1586/14760584.2014.946016. PMID 25182980. S2CID 24133254.
- ↑ Kingdon J, Happold D, Butynski T (2013). Primates. Mammals of Africa. Vol. 2. A&C Black. p. 51. ISBN 978-1-4081-8996-2.
- ↑ Loomis MR (1985). "Immunoprofylaxis in infant great apes". In Graham CE, Bowen JA (eds.). Clinical management of infant great apes: proceedings of a workshop on clinical management of infant great apes, held during the IXth Congress of the International Primatological Society. Monographs in Primatology. Vol. 5. Liss. pp. 107–112. ISBN 978-0845134047.
- ↑ Nieves DJ, Heininger U (June 2016). "Bordetella pertussis". Microbiology Spectrum. 4 (3): 311–339. doi:10.1128/microbiolspec.EI10-0008-2015. ISBN 9781555819446. PMID 27337481. S2CID 30621755.
- ↑ Finger H, von Koenig CH (1996). "Bordetell". In Baron S (ed.). Medical Microbiology (4th ed.). Galveston (TX): University of Texas Medical Branch at Galveston. ISBN 978-0-9631172-1-2. PMID 21413270.
Further reading
- Horst F, von Koenig CH (1996). "Ch. 31 Bordetella". In Baron S (ed.). Medical Microbiology (4th ed.). University of Texas Medical Branch. ISBN 978-0-9631172-1-2. PMID 21413252. NBK7813.