Factor interacting with PAPOLA and CPSF1 (i.e, FIP1L1; also termed Pre-mRNA 3'-end-processing factor FIP1) is a protein that in humans is encoded by the FIP1L1 gene (also known as Rhe, FIP1, and hFip1).[3][4] A medically important aspect of the FIP1L1 gene is its fusion with other genes to form fusion genes which cause clonal hypereosinophilia and leukemic diseases in humans.
Gene
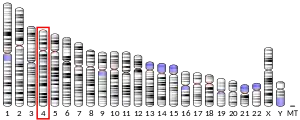
The human FIP1L1 gene is located on chromosome 4 at position q12 (4q12), contains 19 exons, and codes for a complete protein consisting of 594 amino acids. However, alternative splicing of its Precursor mRNA results in multiple transcript variants encoding distinct FIP1L1 protein isoforms. The FIP1L1 gene is found in a wide range of species, being designated as FIP1 in Saccharomyces cerevisiae (yeast) and fip1l1 in coho salmon as well as mice and numerous other mammalian species.[5][6]
In humans, an interstitial chromosomal deletion of about 800 kilobases at 4q12 deletes the CHIC2 gene (i.e.cysteine rich hydrophobic domain 2 gene) to create an in-frame fusion of the FIP1L1 gene with the platelet-derived growth factor receptor alpha gene (PGDFRA) gene. The product of PDGFRA, platelet-derived growth factor receptor alpha (PDGFRA), is a tyrosine kinase receptor of the RTK class III. When bound by its proper ligand, Platelet-derived growth factor (PDGF), it tyrosine kinase becomes active in phosphorylating proteins that, among other functions, promote cell growth and proliferation. (The FIP1L1-PDGFRA mutation was the first description of a gain of function mutation resulting from an interstitial deletion instead of a chromosomal translocation.) The FIP1L1-PDGFRA fusion gene consists of the 5'-end of FIP1L1 united to the 3'-end of PGDFRA at variable breakpoints in both genes extending over a 40 kilobase region in FIP1L1 and a small region of exon 12 in PDGFRA. The fusion gene may produce a protein consisting of the first 233 amino acids of FIP1L1 joined to the last 523 amino acids of PDGFRA or fused proteins consisting of other FIP1L1 and PDGFRA amino acid lengths. The known FIP1L1-PDGFRA fusion proteins exhibit similar if not identical pathological activities.[7]
A Chromosomal translocation of FIP1L1 (4q12) with the Retinoic acid receptor alpha gene, i.e. RARA, (17q12) at various points yields a (15;17)(q22;q21) fusion gene, FIP1L1-RARA that also has been implicated in the development of human leukemic diseases in three case reports.[8]
FIPL1 function
FIP1L1 is a subunit of the cleavage and polyadenylation specificity factor subunit 1 (CPSF1) complex that polyadenylates the 3' end of precursor mRNAs (pre-mRNA) (see CPSF). The FIP1 motif of 40 amino acids on FIP1L1 is responsible for its binding to CPSF1. CPSF1 is an RNA processing protein that binds to uracil-rich sequences in pre-mRNA, concurrently binds with and stimulates POPOLA, i.e. Polynucleotide adenylyltransferase, and then proceeds to add adenylyl residues to pre-mRNA. This poly-adenylyl action increases pre-mRNA's maturation and movement from the nucleus to cytoplasm while also increasing the stability of the mRNA formed from pre-mRNA: FIP1L1 is a Pre-mRNA 3'-end-processing factor. FIP1L1 gene fusions between it and either the platelet-derived growth factor receptor, alpha (PGDFRA) or Retinoic acid receptor alpha (RARA) genes are causes of certain human diseases associated with pathologically increased levels of blood eosinophils and/or Leukemias.[8][5]
FIP1L1-PDGFRA fusion genes
Expression
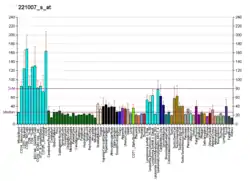
FIP1L1-PDGFRA fusion genes have been detected in the eosinophils, neutrophils, mast cells, monocytes, T lymphocytes, and B lymphocytes involved in hematological malignancies. This suggests that the initial underlying genetic defect in these malignancies can begin in myeloid or lymphoid progenitor cells or in precursors to these myeloid and lymphoid progenitor cells.[7] In the majority of instances, this fusion appears in and promotes the proliferation and differentiation of myeloid precursor cells along the eosinophil lineage. In other cases, however, the fusion, while occurring in myeloid precursor cells, promotes proliferation and differentiation of precursor cells along the neutrophil lineage or, less commonly, occurs in lymphoid precursor cells to promote the proliferation and differentiation of precursor cells along the lymphoid lineage.[9]
Function
FIP1L1-PDGFRA fusion proteins retain PDGFRA-related Tyrosine kinase activity but, unlike PDGFRA, their tyrosine kinase is constitutive, i.e. continuously active: the fusion proteins lack the intact protein's 3'-end that includes its juxtamembrane domain which normally blocks tyrosine kinase activity unless PDGFRA is bound to its activating ligand, platelet-derived growth factor. FIP1L1-PDGFRA fusion proteins are also resistant to PDGFRA's normal pathway of degradation, i.e. Proteasome-dependent ubiquitnation. In consequence, they are highly stable, long-lived, unregulated, and continuously express the stimulating actions of their PDGFRA tyrosine kinase component.[7] In consequence, cells expressing FIP1L1-PDGFRA fusion proteins differentiate and proliferate along eosinophil, other granulocyte, or T lymphocyte lineages and bearers of these mutations suffer either: a) chronic eosinophilia which may progress to hypereosinophilia, the hypereosinophilic syndrome, and chronic eosinophilic leukemia; b) a type of myeloproliferative neoplasm/myeloblastic leukemia not distinguished by eosinophilia; or c) T-lymphoblastic leukemia/lymphoma.[7][9][10] At least one case of FIP1L1-PDGFRA-induced disease presented as a myeloid sarcoma with eosinophilia has been reported.[7] (i.e. These pathological proliferation and differentiation responses are due to the unabated activity of the fusion proteins' tyrosine kinase in phosphorylating and thereby activating certain proteins that promote these functions. For example, in vitro studies show that a FIP1L1-PDGFRA fusion gene stimulates CD34+ cells to proliferate and differentiate along the eosinophil lineage by causing the activation of NF-κB, STAT5, and Protein kinase B cell signaling pathways. The FIP1L1 component of FIP1L1-PDGFRA is required for the fusion protein to activate STAT4 and protein kinase B.[7][8]
Clinical aspects
Incidence
The age-adjusted incidence of hypereosinophilic syndrome/chronic eosinophilic leukemia reported by the International Classification of Diseases for Oncology (Version 3) is ~0.036 per 100,000 with the mean frequency of FIP1L1-PDGFRA gene fusions occurring in ~10% of patients with hypereosinophilia as detected in developed countries. The fused gene occurs with a male/female ratio of 1.47; the reason for this male predominance is not known. The fusion gene has been found in people of all age groups but only rarely in infants and children.[10]
Presentation
The ~70% of patients with the FIP1L1-PDGFRA fusion gene (also termed the F/P fusion gene) and marked eosinophilia commonly complain of weakness and malaise. They may also present with or have a history of signs and/or symptoms that are due to the damaging actions of tissue-infiltrating eosinophils such as: skin rashes or erythema; eosinophilic myocarditis (i.e. heart disease which may manifest as coronary artery disease, heart failure due to injured cardiac muscle, restrictive cardiomyopathy due to cardiac fibrosis, or blockage of arteries due to the embolization of blood clots that from in the heart); pulmonary airway and parenchymal disease; eosinophilic gastroenteritis; eosinophilic esophagitis; and dysfunction of other organs targeted by eosinophils. The ~30% of patients in whom the fusion gene effects non-eosinophilic granulocyte or lymphoid cell lineages present with signs and symptoms respectively of acute myeloid leukemia or lymphoma T-lymphoblastic leukemia/lymphoma or lymphocytic leukemia.[7][11][12]
Diagnosis
Patients expressing the eosinophil-driving fusion protein typically present with hypereosinophilia arbitrarily define as blood cell counts containing greater than 1.5x109/liter eosinophils that have persisted for more than 6 months. However, lower levels of eosinophil counts and/or eosinophilia with a shorter history of duration are not a counter-indication of the diagnoses. These patients also exhibit elevations in their serum levels of Vitamin B12 and tryptase. Elevations of serum VitaminB12 and tryptase are seen regularly in systemic mastocytosis, a disease which may also present with eosinophilia and must be distinguished from FIP1L1-PDGFRA-induced diseases because of the very different treatments for the two types of diseases. Bone marrow examination may reveal increases in eosinophils and mast cells but usually does not contain elevated numbers of precursor cells or cells with microscopically visible chromosome abnormalities. This examination may be useful in excluding other malignant diseases associated with eosinophilia such as acute myeloid leukemia but does not give definitive results indicating FIP1L1-PDGFRA-induced disease. Rather, definitive results are obtained by detecting the presence of the FIP1L1-PDGFRA fusion gene in the blood and/or bone marrow cells of sufferers by cytogenic analysis using Fluorescence in situ hybridization or nested Reverse transcription polymerase chain reaction testing. Non-eosinophilic forms of FIP1L1-PDGFRA fusion gene-induced diseases are suggested by the presence of morphologically abnormal or excessive numbers of myeloid or lymphoid cells in the blood or bone marrow and, with respect to the lymphoid variants, by the presence of lymphadenopathy and/or lymphoma masses; ultimately, these variants also require demonstration of the FIP1L1-PDGFRA fusion genes fr diagnosis.[7][9][13]
Treatment
FIP1L1-PDGFRA fusion gene-induced eosinophil leukemia diseases, unlike most other diseases involving hypereosinophilia, are typically resistant to corticosteroid therapy.[14] However, and unlike most cases of myeloid leukemia, FIP1L1-PDGFRA fusion gene-induced eosinophil leukemia diseases (including a case presenting with myeloid sarcoma) have been treated with great success and long term remissions using low dosages of the tyrosine kinase inhibitor, Imatinib.[11] This drug, also known as Gleevec, has been a FDA-approved and most successful treatment for Philadelphia chromosome-positive chronic myelogenous leukemia (CML) and certain other diseases. More recently, the FDA approved Gleevec for treatingFIP1L1-PDGFRA fusion gene-induced eosinophil leukemia. Commonly, patients suffering this disease respond to low dos (e.g. 100 mg/day) Gleevec but if not attaining complete remission at this dose may require the higher dosages (up to 400/mg/day) typically used to treat CML. Acquired resistance to Gleevec is uncommon but has been observed in patients whose mutated cells develop a T674I or D842V mutation in the fused gene.[13][9] Should FIP1L1-PDGFRA fusion gene-induced eosinophil leukemia diseases become resistant to or enter an accelerated or blast phase while on Gleevec therapy, the aggressive chemotherapy and/or bone marrow transplantation used to treat aggressive leukemia may be required.
While the success of Gleevec in treating the myeloproliferative neoplasm/myeloblastic leukemia or T-lymphoblastic leukemia/lymphoma forms of FIP1L1-PDGFRA fusion gene-induced disease is unclear, initial treatment with the drug is recommended.
FIP1L1-RARA
RARA, the Retinoic acid receptor alpha gene, is located on human chromosome 17 at position q21.2 (i.e. 17q21.2), consists of 17 exons, and encodes the nuclear retinoic acid receptor alpha (RARA) protein. The RARA protein, when ligand-bound, regulates the expression of genes that are implicated in the control of development, differentiation, apoptosis, myelopoiesis, and the transcription of transcription factors which in turn regulate the transcription of clock genes. Translocations between this 17q21.2 locus and several other loci have been associated with acute promyelocytic leukemia.[15] Three case reports have found that chromosome translocations between FIP1L1 and RARA gene loci are associated with two cases of acute promyelocytic leukemia and one case of juvenile myelomonocytic leukemia. Relatively little is known about function of or therapy for these translocations except that: a) the fusion gene was generated juxtaposing exons 15 and 3 of FIP1L1 and RARA, respectively; b) retinoic acid, a ligand for the RARA protein, is exceptionally potent in causing a human eosinophil line to die by apoptosis; c) the disease responses to retinoic acid as well as more aggressive therapies could not be evaluated because of severity and rapid progression of the diseases; d) and in vitro studies indicate that the FIP1L1-RARA fusion protein represses the activation of RARA-activated genes.[8][16]
References
- 1 2 3 GRCh38: Ensembl release 89: ENSG00000145216 - Ensembl, May 2017
- ↑ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ↑ Wiemann S, Weil B, Wellenreuther R, Gassenhuber J, Glassl S, Ansorge W, Bocher M, Blocker H, Bauersachs S, Blum H, Lauber J, Dusterhoft A, Beyer A, Kohrer K, Strack N, Mewes HW, Ottenwalder B, Obermaier B, Tampe J, Heubner D, Wambutt R, Korn B, Klein M, Poustka A (Mar 2001). "Toward a catalog of human genes and proteins: sequencing and analysis of 500 novel complete protein coding human cDNAs". Genome Res. 11 (3): 422–35. doi:10.1101/gr.GR1547R. PMC 311072. PMID 11230166.
- ↑ "Entrez Gene: FIP1L1 FIP1 like 1 (S. cerevisiae)".
- 1 2 "FIP1L1 factor interacting with PAPOLA and CPSF1 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov.
- ↑ "Pre-mRNA 3'-end-processing factor FIP1 (Q6UN15) < InterPro < EMBL-EBI". www.ebi.ac.uk.
- 1 2 3 4 5 6 7 8 Vega F, Medeiros LJ, Bueso-Ramos CE, Arboleda P, Miranda RN (2015). "Hematolymphoid neoplasms associated with rearrangements of PDGFRA, PDGFRB, and FGFR1". American Journal of Clinical Pathology. 144 (3): 377–92. doi:10.1309/AJCPMORR5Z2IKCEM. PMID 26276769. S2CID 10435391.
- 1 2 3 4 Iwasaki J, Kondo T, Darmanin S, Ibata M, Onozawa M, Hashimoto D, Sakamoto N, Teshima T (2014). "FIP1L1 presence in FIP1L1-RARA or FIP1L1-PDGFRA differentially contributes to the pathogenesis of distinct types of leukemia". Annals of Hematology. 93 (9): 1473–81. doi:10.1007/s00277-014-2085-1. hdl:2115/59854. PMID 24763514. S2CID 25915058.
- 1 2 3 4 Reiter A, Gotlib J (2017). "Myeloid neoplasms with eosinophilia". Blood. 129 (6): 704–714. doi:10.1182/blood-2016-10-695973. PMID 28028030.
- 1 2 Gotlib J (2015). "World Health Organization-defined eosinophilic disorders: 2015 update on diagnosis, risk stratification, and management". American Journal of Hematology. 90 (11): 1077–89. doi:10.1002/ajh.24196. PMID 26486351. S2CID 42668440.
- 1 2 Helbig G (February 2018). "Imatinib for the treatment of hypereosinophilic syndromes". Expert Review of Clinical Immunology. 14 (2): 163–170. doi:10.1080/1744666X.2018.1425142. PMID 29303368. S2CID 6580949.
- ↑ Séguéla PE, Iriart X, Acar P, Montaudon M, Roudaut R, Thambo JB (2015). "Eosinophilic cardiac disease: Molecular, clinical and imaging aspects". Archives of Cardiovascular Diseases. 108 (4): 258–68. doi:10.1016/j.acvd.2015.01.006. PMID 25858537.
- 1 2 Butt NM, Lambert J, Ali S, Beer PA, Cross NC, Duncombe A, Ewing J, Harrison CN, Knapper S, McLornan D, Mead AJ, Radia D, Bain BJ (2017). "Guideline for the investigation and management of eosinophilia" (PDF). British Journal of Haematology. 176 (4): 553–572. doi:10.1111/bjh.14488. PMID 28112388. S2CID 46856647.
- ↑ Roufosse F (2015). "Management of Hypereosinophilic Syndromes". Immunology and Allergy Clinics of North America. 35 (3): 561–75. doi:10.1016/j.iac.2015.05.006. PMID 26209900.
- ↑ "RARA retinoic acid receptor alpha [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov.
- ↑ Menezes J, Acquadro F, Perez-Pons de la Villa C, García-Sánchez F, Álvarez S, Cigudosa JC (2011). "FIP1L1/RARA with breakpoint at FIP1L1 intron 13: a variant translocation in acute promyelocytic leukemia". Haematologica. 96 (10): 1565–6. doi:10.3324/haematol.2011.047134. PMC 3186322. PMID 21750086.
Further reading
- Hartley JL, Temple GF, Brasch MA (2001). "DNA cloning using in vitro site-specific recombination". Genome Res. 10 (11): 1788–95. doi:10.1101/gr.143000. PMC 310948. PMID 11076863.
- Strausberg RL, Feingold EA, Grouse LH, et al. (2003). "Generation and initial analysis of more than 15,000 full-length human and mouse cDNA sequences". Proc. Natl. Acad. Sci. U.S.A. 99 (26): 16899–903. Bibcode:2002PNAS...9916899M. doi:10.1073/pnas.242603899. PMC 139241. PMID 12477932.
- Cools J, DeAngelo DJ, Gotlib J, et al. (2003). "A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome". N. Engl. J. Med. 348 (13): 1201–14. doi:10.1056/NEJMoa025217. PMID 12660384.
- Griffin JH, Leung J, Bruner RJ, et al. (2003). "Discovery of a fusion kinase in EOL-1 cells and idiopathic hypereosinophilic syndrome". Proc. Natl. Acad. Sci. U.S.A. 100 (13): 7830–5. Bibcode:2003PNAS..100.7830G. doi:10.1073/pnas.0932698100. PMC 164673. PMID 12808148.
- Pardanani A, Ketterling RP, Brockman SR, et al. (2004). "CHIC2 deletion, a surrogate for FIP1L1-PDGFRA fusion, occurs in systemic mastocytosis associated with eosinophilia and predicts response to imatinib mesylate therapy". Blood. 102 (9): 3093–6. doi:10.1182/blood-2003-05-1627. PMID 12842979.
- Cools J, Quentmeier H, Huntly BJ, et al. (2004). "The EOL-1 cell line as an in vitro model for the study of FIP1L1-PDGFRA-positive chronic eosinophilic leukemia". Blood. 103 (7): 2802–5. doi:10.1182/blood-2003-07-2479. PMID 14630792.
- Ota T, Suzuki Y, Nishikawa T, et al. (2004). "Complete sequencing and characterization of 21,243 full-length human cDNAs". Nat. Genet. 36 (1): 40–5. doi:10.1038/ng1285. PMID 14702039.
- Sakashita E, Tatsumi S, Werner D, et al. (2004). "Human RNPS1 and its associated factors: a versatile alternative pre-mRNA splicing regulator in vivo". Mol. Cell. Biol. 24 (3): 1174–87. doi:10.1128/MCB.24.3.1174-1187.2004. PMC 321435. PMID 14729963.
- Kaufmann I, Martin G, Friedlein A, et al. (2005). "Human Fip1 is a subunit of CPSF that binds to U-rich RNA elements and stimulates poly(A) polymerase". EMBO J. 23 (3): 616–26. doi:10.1038/sj.emboj.7600070. PMC 1271804. PMID 14749727.
- Pardanani A, Brockman SR, Paternoster SF, et al. (2004). "FIP1L1-PDGFRA fusion: prevalence and clinicopathologic correlates in 89 consecutive patients with moderate to severe eosinophilia". Blood. 104 (10): 3038–45. doi:10.1182/blood-2004-03-0787. PMID 15284118.
- Beausoleil SA, Jedrychowski M, Schwartz D, et al. (2004). "Large-scale characterization of HeLa cell nuclear phosphoproteins". Proc. Natl. Acad. Sci. U.S.A. 101 (33): 12130–5. Bibcode:2004PNAS..10112130B. doi:10.1073/pnas.0404720101. PMC 514446. PMID 15302935.
- Gerhard DS, Wagner L, Feingold EA, et al. (2004). "The status, quality, and expansion of the NIH full-length cDNA project: the Mammalian Gene Collection (MGC)". Genome Res. 14 (10B): 2121–7. doi:10.1101/gr.2596504. PMC 528928. PMID 15489334.
- Wiemann S, Arlt D, Huber W, et al. (2004). "From ORFeome to biology: a functional genomics pipeline". Genome Res. 14 (10B): 2136–44. doi:10.1101/gr.2576704. PMC 528930. PMID 15489336.
- Zhao X, Oberg D, Rush M, et al. (2005). "A 57-nucleotide upstream early polyadenylation element in human papillomavirus type 16 interacts with hFip1, CstF-64, hnRNP C1/C2, and polypyrimidine tract binding protein". J. Virol. 79 (7): 4270–88. doi:10.1128/JVI.79.7.4270-4288.2005. PMC 1061554. PMID 15767428.
- Rual JF, Venkatesan K, Hao T, et al. (2005). "Towards a proteome-scale map of the human protein-protein interaction network". Nature. 437 (7062): 1173–8. Bibcode:2005Natur.437.1173R. doi:10.1038/nature04209. PMID 16189514. S2CID 4427026.
- Mehrle A, Rosenfelder H, Schupp I, et al. (2006). "The LIFEdb database in 2006". Nucleic Acids Res. 34 (Database issue): D415–8. doi:10.1093/nar/gkj139. PMC 1347501. PMID 16381901.
- Cools J, Stover EH, Gilliland DG (2006). "Detection of the FIP1L1-PDGFRA Fusion in Idiopathic Hypereosinophilic Syndrome and Chronic Eosinophilic Leukemia". Detection of the FIP1L1-PDGFRA fusion in idiopathic hypereosinophilic syndrome and chronic eosinophilic leukemia. Vol. 125. pp. 177–87. doi:10.1385/1-59745-017-0:177. ISBN 978-1-59745-017-1. PMID 16502585.
{{cite book}}:|journal=ignored (help) - Stover EH, Chen J, Folens C, et al. (2006). "Activation of FIP1L1-PDGFRalpha requires disruption of the juxtamembrane domain of PDGFRalpha and is FIP1L1-independent". Proc. Natl. Acad. Sci. U.S.A. 103 (21): 8078–83. Bibcode:2006PNAS..103.8078S. doi:10.1073/pnas.0601192103. PMC 1472432. PMID 16690743.
- Beausoleil SA, Villén J, Gerber SA, et al. (2006). "A probability-based approach for high-throughput protein phosphorylation analysis and site localization". Nat. Biotechnol. 24 (10): 1285–92. doi:10.1038/nbt1240. PMID 16964243. S2CID 14294292.