 | |
| Names | |
|---|---|
| IUPAC name
Tris(3-hydroxy-2-methyl-4H-pyran-4-one)gallium | |
| Identifiers | |
3D model (JSmol) |
|
| DrugBank | |
PubChem CID |
|
| UNII | |
| |
| |
| Properties | |
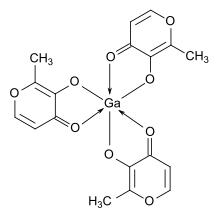
| Ga(C6H5O3)3 | |
| Molar mass | 445.03 g/mol |
| Appearance | White to pale beige crystalline solid or powder |
| Density | 1.56 g/cm3, solid |
| Melting point | 220 °C (decomposes) |
| 24(2) mM; 10.7(9) mg/mL (25 °C) | |
| Structure | |
| Orthorhombic; space group Pbca | |
| Distorted octahedral | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
Infobox references | |
Gallium maltolate is a coordination complex consisting of a trivalent gallium cation coordinated to three maltolate ligands. The compound is a potential therapeutic agent for cancer, infectious disease, and inflammatory disease.[1][2][3][4] A cosmetic skin cream containing gallium maltolate is marketed under the name Gallixa. It is a colorless solid with significant solubility in both water and lipids (octanol-water partition coefficient = 0.41).[1]
Mechanism of action
Gallium maltolate delivers gallium with higher oral bioavailability than that of gallium salts such as gallium nitrate and gallium trichloride.[1] In vitro studies have found gallium to be antiproliferative due primarily to its ability to mimic ferric iron (Fe3+). Ferric iron is essential for DNA synthesis, as it is present in the active site of the enzyme ribonucleotide reductase, which catalyzes the conversion of ribonucleotides to the deoxyribonucleotides required for DNA. Gallium is taken up by the rapidly proliferating cells, but it is not functional for DNA synthesis, so the cells cannot reproduce and they ultimately die by apoptosis. Normally reproducing cells take up little gallium (as is known from gallium scans), and gallium is not incorporated into hemoglobin, accounting for the relatively low toxicity of gallium.[5]
Research
Gallium (III) ion shows anti-inflammatory activity in animal models of inflammatory disease.[2][5][6] Orally administered gallium maltolate has demonstrated efficacy against two types of induced inflammatory arthritis in rats.[6] Experimental evidence suggests that the anti-inflammatory activity of gallium may be due, at least in part, to down-regulation of pro-inflammatory T-cells and inhibition of inflammatory cytokine secretion by macrophages.[2][5][6] Because many iron compounds are pro-inflammatory, the ability of gallium to act as a non-functional iron mimic may contribute to its anti-inflammatory activity.[2]
Gallium maltolate has also been proposed for the treatment for primary liver cancer (hepatocellular carcinoma; HCC). In vitro experiments demonstrated efficacy against HCC cell lines,[4] and encouraging clinical results have been reported.[7]
Gallium compounds are active against infection-related biofilms, particularly those caused by Pseudomonas aeruginosa.[8][9] In related research, locally administered gallium maltolate has shown efficacy against P. aeruginosa in a mouse burn/infection model.[10] The potential of this approach may be somewhat limited by the relatively rapid appearance of gallium-resistant isolates.[11][12]
Oral gallium maltolate has been investigated as a treatment for Rhodococcus equi foal pneumonia, a common and often fatal disease of newborn horses. R. equi can also infect humans with AIDS or who are otherwise immunocompromized.[13][14]
Topically applied gallium maltolate has been studied for use in neuropathic pain (severe postherpetic neuralgia and trigeminal neuralgia).[6] It has been hypothesized that any effect on pain may be related to gallium's anti-inflammatory mechanisms, and possibly from its interactions with certain matrix metalloproteinases and substance P, whose activities are zinc-mediated and which have been implicated in the etiology of pain.[6]
References
- 1 2 3 Bernstein, L.R.; Tanner, T.; Godfrey, C.; Noll, B. (2000). "Chemistry and pharmacokinetics of gallium maltolate, a compound with high oral gallium bioavailability". Metal-Based Drugs. 7 (1): 33–48. doi:10.1155/MBD.2000.33. PMC 2365198. PMID 18475921.
- 1 2 3 4 Bernstein, L.R. (2005). "Therapeutic gallium compounds" (PDF). In Gielen, M.; Tiekink, E.R.T. (eds.). Metallotherapeutic Drugs and Metal-Based Diagnostic Agents: The Use of Metals in Medicine. New York: Wiley. pp. 259–277. ISBN 978-0-470-86403-6.
- ↑ Chitambar, C.R.; Purpi, D.P.; Woodliff, J.; Yang, M.; Wereley J.P. (2007). "Development of Gallium Compounds for Treatment of Lymphoma: Gallium Maltolate, a Novel Hydroxypyrone Gallium Compound, Induces Apoptosis and Circumvents Lymphoma Cell Resistance to Gallium Nitrate" (PDF). J. Pharmacol. Exp. Ther. 322 (3): 1228–1236. doi:10.1124/jpet.107.126342. PMID 17600139. S2CID 12427694.
- 1 2 Chua, M.-Z.; Bernstein, L.R.; Li, R.; So, S.K. (2006). "Gallium maltolate is a promising chemotherapeutic agent for the treatment of hepatocellular carcinoma" (PDF). Anticancer Research. 26 (3A): 1739–1743. PMID 16827101.
- 1 2 3 Bernstein, L.R. (1998). "Mechanisms of therapeutic activity for gallium" (PDF). Pharmacol. Rev. 50 (4): 665–682. PMID 9860806.
- 1 2 3 4 5 Bernstein, Lawrence (2013). "Gallium, therapeutic effects" (PDF). In Kretsinger, R.H.; Uversky, V.N.; Permyakov, E.A. (eds.). Encyclopedia of Metalloproteins. New York: Springer. pp. 823–835. ISBN 978-1-4614-1532-9.
- ↑ Chitambar, C.R. (2012). "Gallium-containing anticancer compounds". Future Med Chem. 4 (10): 1257–1272. doi:10.4155/fmc.12.69. PMC 3574811. PMID 22800370.
- ↑ Kaneko, Y.; Thoendel, M.; Olakanmi, O.; Britigan, B.E.; Singh, P.K. (2007). "The transition metal gallium disrupts Pseudomonas aeruginosa iron metabolism and has antimicrobial and antibiofilm activity". J. Clin. Invest. 117 (4): 877–888. doi:10.1172/JCI30783. PMC 1810576. PMID 17364024.
- ↑ Parsek, M.; Singh, P. (2003). "Bacterial biofilms: an emerging link to disease pathogenesis". Annu. Rev. Microbiol. 57: 677–701. doi:10.1146/annurev.micro.57.030502.090720. PMID 14527295.
- ↑ DeLeon K.; Balldin F.; Watters C.; Hamood A.; Griswold J.; Sreedharan S.; Rumbaugh K.P. (2009). "Gallium maltolate treatment eradicates Pseudomonas aeruginosa infection in thermally injured mice". Antimicrobial Agents and Chemotherapy. 53 (4): 1331–1337. doi:10.1128/AAC.01330-08. PMC 2663094. PMID 19188381.
- ↑ Tovar-García, Arturo; Angarita-Zapata, Vanesa; Cazares, Adrián; Jasso-Chávez, Ricardo; Belmont-Díaz, Javier; Sanchez-Torres, Viviana; López-Jacome, Luis Esaú; Coria-Jiménez, Rafael; Maeda, Toshinari; García-Contreras, Rodolfo (2020-04-01). "Characterization of gallium resistance induced in a Pseudomonas aeruginosa cystic fibrosis isolate". Archives of Microbiology. 202 (3): 617–622. doi:10.1007/s00203-019-01777-y. ISSN 1432-072X. PMID 31773196. S2CID 208302170.
- ↑ García-Contreras, Rodolfo; Lira-Silva, Elizabeth; Jasso-Chávez, Ricardo; Hernández-González, Ismael L.; Maeda, Toshinari; Hashimoto, Takahiro; Boogerd, Fred C.; Sheng, Lili; Wood, Thomas K.; Moreno-Sánchez, Rafael (December 2013). "Isolation and characterization of gallium resistant Pseudomonas aeruginosa mutants". International Journal of Medical Microbiology. 303 (8): 574–582. doi:10.1016/j.ijmm.2013.07.009. PMID 23992635.
- ↑ Harrington, J.R.; Martens, R.J.; Cohen, N.D.; Bernstein, L.R. (2006). "Antimicrobial activity of gallium against virulent Rhodococcus equi in vitro and in vivo". J. Vet. Pharmacol. Ther. 29 (2): 121–127. doi:10.1111/j.1365-2885.2006.00723.x. PMID 16515666.
- ↑ Martens, R.J.; Mealey, K.; Cohen, N.D.; Harrington, J.R.; Chaffin, M.K.; Taylor, R.J.; Bernstein, L.R. (2007). "Pharmacokinetics of gallium maltolate after intragastric administration in neonatal foals". Am. J. Vet. Res. 68 (10): 1041–1044. doi:10.2460/ajvr.68.10.1041. PMID 17916007.