GnRH neurons, or gonadotropin-releasing hormone expressing neurons, are the cells in the brain that control the release of reproductive hormones from the pituitary. These brain cells control reproduction by secreting GnRH into the hypophyseal portal capillary bloodstream, so are sometimes referred to as “sex neurons”. This small capillary network carries GnRH to the anterior pituitary, causing release of luteinizing hormone (LH) and follicle stimulating hormone (FSH) into the wider bloodstream. When GnRH neurons change their pattern of release from the juvenile to the adult pattern of GnRH secretion, puberty is initiated. Failure of GnRH neurons to form the proper connections, or failure to successfully stimulate the pituitary with GnRH, means that puberty is not initiated. These disruptions to the GnRH system cause reproductive disorders like hypogonadotropic hypogonadism or Kallmann Syndrome.
Origins of GnRH neurons
In 1989, two research groups independently discovered that GnRH neurons, which in adults are scattered throughout the hypothalamus, do not originate in this region of the brain. Instead, they migrate into the brain along olfactory axon fibers from the nose.[1][2] Most GnRH neurons are born from stem cells in the nasal placode (embryonic nasal tissue). More recently, it was discovered that a subset of GnRH neurons can trace their origins not from the nasal placode, but from the neural crest earlier in embryogenesis.[3] This subset of cells migrates into the nasal placode, where they intermix with GnRH neurons born in this region, and migrate together into the brain.
Journey from nose to brain
On their journey from nose to brain, GnRH neurons pass through nasal tissue, the early skull, and move through several regions of the forebrain before reaching their destinations.[4] Along the way, secreted and membrane-bound molecules guide them in the right direction and help to set their movement speed. GnRH neurons that fail to enter the brain, or that migrate to the wrong region, are not functional and can even undergo programmed cell death. This failure of GnRH neurons to migrate into the brain is the main cause of Kallmann Syndrome.[5] GABA, which depolarizes embryonic GnRH neurons, slows movement but helps them to move straight along their pathway.[6] SDF activates hyperpolarizing GIRK channels, accelerating movement speeds. Other guidance cues like semaphorins[7][8] and HGF[9] regulate movement of GnRH neurons as well.
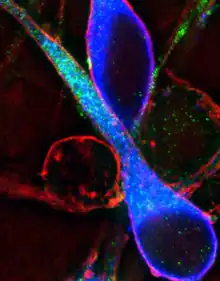
Movement of GnRH neurons
Scientists have discovered how guidance molecules cause GnRH neurons to speed up or slow down. Normally, any calcium ions in the cell are rapidly pulled into organelles like the mitochondria or endoplasmic reticulum. Guidance molecules cause the release of these calcium ions back into the cell cytoplasm, where calcium sensing proteins re-organize the cell’s actin[10] and microtubule[11] cytoskeleton, which are the molecular filaments that give a cell its shape. This causes contractions in the cell (similar to muscle contractions) that link to adhesive proteins on the cell surface,[12] pulling the cell forward.
GnRH Physiology
The shift to high frequency electrical activity in GnRH neurons is the signal that initiates puberty. GnRH neurons receive input from classical neurotransmitters like glutamate and GABA.[13] These neurotransmitters cause electrical activity that is regulated through development to cause broad changes in calcium ion entry into the cell through voltage-sensitive ion channels. This triggers the release of GnRH into the hypophyseal portal capillary bloodstream, where the GnRH hormone activates the pituitary to release luteinizing hormone and follicle stimulating hormone. In addition to classical neurotransmitters, some guidance molecules can change the wiring of GnRH neurons to the portal capillary system, altering the strength of the signal to the pituitary gland.[14]
Regulation of GnRH neurons
GnRH neurons integrate information from the body to regulate reproduction. The strongest activator of GnRH neurons is a hormone called Kisspeptin.[15] GnRH neurons also integrate information from the body through hormones like neuropeptide Y[16] and adiponectin.[17] These hormones provide the GnRH neurons with information about the body’s status to help determine whether reproduction should be prioritized or suppressed.
References
- ↑ Schwanzel-Fukuda, M; Pfaff, DW (1989). "Origin of luteinizing hormone-releasing hormone neurons". Nature. 338 (6211): 161–4. Bibcode:1989Natur.338..161S. doi:10.1038/338161a0. PMID 2645530. S2CID 4310861.
- ↑ Wray, S; Grant, P; Gainer, H (1989). "Evidence that cells expressing luteinizing hormone-releasing hormone mRNA in the mouse are derived from progenitor cells in the olfactory placode". Proceedings of the National Academy of Sciences. 86 (20): 8132–6. Bibcode:1989PNAS...86.8132W. doi:10.1073/pnas.86.20.8132. PMC 298229. PMID 2682637.
- ↑ Forni, PE; Taylor-Burds, C; Melvin, VS; Williams, T; Wray, S (2011). "Neural crest and ectodermal cells intermix in the nasal placode to give rise to GnRH-1 neurons, sensory neurons, and olfactory ensheathing cells". Journal of Neuroscience. 31 (18): 6915–27. doi:10.1523/JNEUROSCI.6087-10.2011. PMC 3101109. PMID 21543621.
- ↑ Wray, S (2010). "From nose to brain: development of gonadotrophin-releasing hormone-1 neurones". Journal of Neuroendocrinology. 22 (7): 743–53. doi:10.1111/j.1365-2826.2010.02034.x. PMC 2919238. PMID 20646175.
- ↑ Valdes-Socin, H (2014). "Reproduction, smell, and neurodevelopmental disorders: genetic defects in different hypogonadotropic hypogonadal syndromes" (PDF). Frontiers in Endocrinology. 5: 109. doi:10.3389/fendo.2014.00109. PMC 4088923. PMID 25071724.
- ↑ Casoni, F; Hutchins, BI; Donohue, D; Fornaro, M; Condie, BG; Wray, S (2012). "SDF and GABA interact to regulate axophilic migration of GnRH neurons". Journal of Cell Science. 125 (21): 5015–25. doi:10.1242/jcs.101675. PMC 3533389. PMID 22976302.
- ↑ Giacobini, P (2008). "Semaphorin 4D regulates gonadotropin hormone-releasing hormone-1 neuronal migration through PlexinB1-Met complex". Journal of Cell Biology. 183 (3): 555–66. doi:10.1083/jcb.200806160. PMC 2575794. PMID 18981235.
- ↑ Messina, Andrea; Ferraris, Nicoletta; Wray, Susan; Cagnoni, Gabriella; Donohue, Duncan E.; Casoni, Filippo; Kramer, Phillip R.; Derijck, Alwin A.; Adolfs, Youri (2011-12-15). "Dysregulation of Semaphorin7A/β1-integrin signaling leads to defective GnRH-1 cell migration, abnormal gonadal development and altered fertility". Human Molecular Genetics. 20 (24): 4759–4774. doi:10.1093/hmg/ddr403. ISSN 0964-6906. PMC 3221532. PMID 21903667.
- ↑ Giacobini, P (2007). "Hepatocyte growth factor acts as a motogen and guidance signal for gonadotropin hormone-releasing hormone-1 neuronal migration" (PDF). Journal of Neuroscience. 27 (2): 431–45. doi:10.1523/JNEUROSCI.4979-06.2007. PMC 6672060. PMID 17215404.
- ↑ Hutchins, BI; Klenke, U; Wray, S (2013). "Calcium release-dependent actin flow in the leading process mediates axophilic migration". Journal of Neuroscience. 33 (28): 11361–71. doi:10.1523/JNEUROSCI.3758-12.2013. PMC 3724331. PMID 23843509.
- ↑ Hutchins, BI; Wray, S (2014). "Capture of microtubule plus-ends at the actin cortex promotes axophilic neuronal migration by enhancing microtubule tension in the leading process". Frontiers in Cellular Neuroscience. 8: 400. doi:10.3389/fncel.2014.00400. PMC 4245908. PMID 25505874.
- ↑ Parkash, J (2012). "Suppression of β1-integrin in gonadotropin-releasing hormone cells disrupts migration and axonal extension resulting in severe reproductive alterations". Journal of Neuroscience. 32 (47): 16992–7002. doi:10.1523/JNEUROSCI.3057-12.2012. PMC 5238668. PMID 23175850.
- ↑ Constantin, S; Klenke, U; Wray, S (2010). "The calcium oscillator of GnRH-1 neurons is developmentally regulated". Endocrinology. 151 (8): 3863–73. doi:10.1210/en.2010-0118. PMC 2940530. PMID 20555030.
- ↑ Giacobini, P (2014). "Brain endothelial cells control fertility through ovarian-steroid-dependent release of semaphorin 3A". PLOS Biology. 12 (3): e1001808. doi:10.1371/journal.pbio.1001808. PMC 3949669. PMID 24618750.
- ↑ de Roux, N; Genin, E; Carel, JC; Matsuda, F; Chaussain, JL; Milgrom, E (2003). "Hypogonadotropic hypogonadism due to loss of function of the KiSS1-derived peptide receptor GPR54". Proceedings of the National Academy of Sciences. 100 (19): 10972–6. Bibcode:2003PNAS..10010972D. doi:10.1073/pnas.1834399100. PMC 196911. PMID 12944565.
- ↑ Klenke, U; Constantin, S; Wray, S (2010). "Neuropeptide Y directly inhibits neuronal activity in a subpopulation of gonadotropin-releasing hormone-1 neurons via Y1 receptors". Endocrinology. 151 (6): 2736–46. doi:10.1210/en.2009-1198. PMC 2875836. PMID 20351316.
- ↑ Klenke, U; Taylor-Burds, C; Wray, S (2014). "Metabolic influences on reproduction: adiponectin attenuates GnRH neuronal activity in female mice". Endocrinology. 155 (5): 1851–63. doi:10.1210/en.2013-1677. PMC 3990841. PMID 24564393.