| Myelomalacia | |
|---|---|
| MRI image shows spinal bleeding (myelomalacia). |
Myelomalacia is a pathological term referring to the softening of the spinal cord.[1] Possible causes of myelomalacia include cervical myelopathy, hemorrhagic infarction, or acute injury, such as that caused by intervertebral disc extrusion.[2]
In advanced stages, this disorder causes flaccid paraplegia (impairment of motor function in lower extremities), total areflexia (below normal or absence of reflexes) of the pelvic limbs and anus, loss of deep pain perception caudal (toward the coccyx, or tail) to the site of spinal cord injury, muscular atrophy (wasting away of muscle tissue), depressed mental state, and respiratory difficulty due to intercostal (muscles that run between the ribs) and diaphragmatic paralysis.[3] Gradual cranial migration of the neurological deficits (problems relating to the nervous system), is known as ascending syndrome and is said to be a typical feature of diffuse myelomalacia. Although clinical signs of myelomalacia are observed within the onset (start) of paraplegia, sometimes they may become evident only in the post-operative period, or even days after the onset of paraplegia. Death from myelomalacia may occur as a result of respiratory paralysis when the ascending lesion (abnormal damaged tissue) reaches the motor nuclei of the phrenic nerves (nerves between the C3-C5 region of the spine) in the cervical (neck) region.[4]
Classification
Myelomalacia affects the neurological functions in the spinal cord. Once breached, the ramification of the damage directly affects the motor functions of the body. Because the central nervous system is affected, the condition is classified under the neurological field of study.
Spinal cord injury
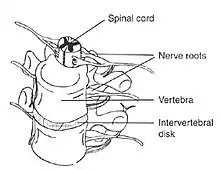
When myelomalacia occurs, the damage done to the spinal cord may range from minimal to extensive. The spinal cord and the brain work together, making them the key components of the central nervous system.[5] Damage to this system affects specific functions of the body, primarily relating to the function of muscles. The areas most commonly injured include the cervical vertebrae (C1-C7), and the lumbar spine (L1-L5).[6]
Symptoms
Depending on the extent of the spinal cord injury, the symptoms may vary.[7] Though every case is different, several cases reported loss of motor functions in the extremities, areflexia or sudden jerks of the limbs, loss of pain perception, or even paralysis; all of which are possible indicators of a damaged and softened spinal cord.[7] In the most severe cases, paralysis of the respiratory system manifests in death.
Cause
The most common way the disorder occurs is from a result of hemorrhaging (bleeding within) or inadequate blood supply to the spinal cord, making it weak and susceptible to damage.
Because myelomalacia involves a damaged spinal cord, it may occur in any individual. Those most at risk are the geriatric population due to weaker bone density. Once the spinal injury has occurred, one of two things may happen. Firstly, hemorrhaging within the spinal cord may cause compression, which damages the spinal cord even further. Another consequence of myelomalacia is improper circulation of blood to the area damaged, resulting in further damage to the spinal cord.

Sport Athletes
Due to extensive physical contact and activity, many athletes become victim to myelomalacia.[1] Any accidents or injuries attained during athletic competition to the spinal cord may result in myelomalacia. Accounts of awkward landing on the ground or being hit intensively have attested to spinal cord injury.
Geriatric
With the growth in the elderly population of humans, there has been a rise to myelomalacia. Because the human body begins to deteriorate with age, and because human population is living many years longer, there has been a growth in cases of myelomalacia. As the bones in the body begin to weaken in a process known as osteopenia, the body is more vulnerable to damage. A simple fall may damage the spinal cord and myelomalacia may soon ensue.
Diagnosing
There are two tests that can provide a definite diagnosis of myelomalacia; magnetic resonance imaging (MRI), or myelography.[8] Diffuse hyperintensity on T2-weighted imaging, and hypointensity on T1-weighted imaging of the spinal cord can be an indication of the onset or progression of myelomalacia
Treatment
There is no known treatment to reverse nerve damage due to myelomalacia. In some cases, surgery to alleviate the injury to the area may slow or stop further damage. As motor function degenerates, muscle spasticity and atrophy may occur. Medications such as NSAIDs and gabapentinoids may be prescribed to reduce swelling of the spinal cord, pain, and spasticity.[9]
Research is underway to consider the potential of stem cells for treatment of neurodegenerative diseases. There are, however, no approved stem cell therapies for myelomalacia.[10]
See also
References
- 1 2 Platt SR, McConnell JF, Bestbier M (2006). "Magnetic resonance imaging characteristics of ascending hemorrhagic myelomalacia in a dog". Veterinary Radiology & Ultrasound. 47 (1): 78–82. doi:10.1111/j.1740-8261.2005.00109.x. PMID 16429989.
- ↑ Quencer RM, Sheldon JJ, Post MJ, Diaz RD, Montalvo BM, Green BA, Eismont FJ (July 1986). "MRI of the chronically injured cervical spinal cord". AJR. American Journal of Roentgenology. 147 (1): 125–32. doi:10.2214/ajr.147.1.125. PMID 3487204.
- ↑ McMinn P, Stratov I, Nagarajan L, Davis S (January 2001). "Neurological manifestations of enterovirus 71 infection in children during an outbreak of hand, foot, and mouth disease in Western Australia". Clinical Infectious Diseases. 32 (2): 236–42. doi:10.1086/318454. JSTOR 4482452. PMID 11170913.
- ↑ Langdon FW (1994). "Myelomalacia, With Especial Reference To Diagnosis and Treatment". The Journal of Nervous and Mental Disease. 32 (5): 233–44. doi:10.1097/00005053-190504000-00002.
- ↑ Dubreuil CI, Winton MJ, McKerracher L (July 2003). "Rho activation patterns after spinal cord injury and the role of activated Rho in apoptosis in the central nervous system". The Journal of Cell Biology. 162 (2): 233–43. doi:10.1083/jcb.200301080. JSTOR 1621683. PMC 2172802. PMID 12860969.
- ↑ Anderson MJ (February 1993). "Differences in growth of neurons from normal and regenerated teleost spinal cord in vitro". In Vitro Cellular & Developmental Biology. 29A (2): 145–52. doi:10.1007/BF02630946. JSTOR 4296977. PMID 8473272.
- 1 2 Potter K, Saifuddin A (May 2003). "Pictorial review: MRI of chronic spinal cord injury". The British Journal of Radiology. 76 (905): 347–52. doi:10.1259/bjr/11881183. PMID 12763953.
- ↑ Jackson RP, Becker GJ, Jacobs RR, Montesano PX, Cooper BR, McManus GE (December 1989). "The neuroradiographic diagnosis of lumbar herniated nucleus pulposus: I. A comparison of computed tomography (CT), myelography, CT-myelography, discography, and CT-discography". Spine. 14 (12): 1356–61. doi:10.1097/00007632-198912000-00012. PMID 2694388.
- ↑ Hirpara KM, Butler JS, Dolan RT, O'Byrne JM, Poynton AR (2012). "Nonoperative modalities to treat symptomatic cervical spondylosis". Advances in Orthopedics. 2012: 294857. doi:10.1155/2012/294857. PMC 3168941. PMID 21991426.
- ↑ "Stem Cell Basics". National Institutes of Health.