PD-1 inhibitors and PD-L1 inhibitors are a group of checkpoint inhibitor anticancer drugs that block the activity of PD-1 and PDL1 immune checkpoint proteins present on the surface of cells. Immune checkpoint inhibitors are emerging as a front-line treatment for several types of cancer.[1]
PD-1 and PD-L1 inhibitors act to inhibit the association of the programmed death-ligand 1 (PD-L1) with its receptor, programmed cell death protein 1 (PD-1). The interaction of these cell surface proteins is involved in the suppression of the immune system and occurs following infection to limit the killing of bystander host cells and prevent autoimmune disease.[2] This immune checkpoint is also active in pregnancy,[3] following tissue allografts,[4] and in different types of cancer.[5]
| Name | Target | Approved |
|---|---|---|
| Nivolumab | PD-1 | 2014 |
| Pembrolizumab | PD-1 | 2014 |
| Atezolizumab | PD-L1 | 2016 |
| Avelumab | PD-L1 | 2017 |
| Durvalumab | PD-L1 | 2017 |
| Cemiplimab | PD-1 | 2018 |
| Dostarlimab | PD-1 | 2021 |
| Retifanlimab | PD-1 | 2023 |
| Toripalimab | PD-1 | 2023 |
History
The concept of blocking PD-1 and PD-L1 for the treatment of cancer was first published in 2001.[6] Pharmaceutical companies began attempting to develop drugs to block these molecules, and the first clinical trial was launched in 2006, evaluating nivolumab. As of 2017, more than 500 clinical trials involving PD-1 and PD-L1 inhibitors have been conducted in more than 20,000 patients.[7] By the end of 2017, PD-1/PD-L1 inhibitors had been approved for the treatment of nine forms of cancer.[8]
Cancer immunotherapy
In the cancer disease state, the interaction of PD-L1 on the tumor cells with PD-1 on a T-cell reduces T-cell function signals to prevent the immune system from attacking the tumor cells.[9] Use of an inhibitor that blocks the interaction of PD-L1 with the PD-1 receptor can prevent the cancer from evading the immune system in this way.[9] Several PD-1 and PD-L1 inhibitors are being trialled within the clinic for use in advanced melanoma, non-small cell lung cancer, renal cell carcinoma, bladder cancer and Hodgkin lymphoma, amongst other cancer types.[5][10]
Immunotherapy with these immune checkpoint inhibitors appears to shrink tumours in a higher number of patients across a wider range of tumour types and is associated with lower toxicity levels than other immunotherapies, with durable responses.[5] However, de-novo and acquired resistance is still seen in a large proportion of patients.[9] Hence PD-L1 inhibitors are considered to be the most promising drug category for many different cancers.[5][11]
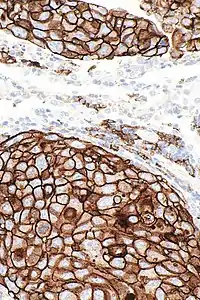
Not all patients respond to PD-1/PD-L1 inhibitors. The FDA has approved several assays to measure the level of PD-L1 expressed by tumor cells, in order to predict the likelihood of response to an inhibitor. PD-L1 levels have been found to be highly predictive of response. Higher mutation burden is also predictive of response to anti-PD-1/PD-L1 agents.[8]
PD-1 and PD-L1 inhibitors are closely related to CTLA4 (cytotoxic T-lymphocyte-associated protein 4) inhibitors, such as ipilimumab. PD-1 and CTLA-4 are both expressed on activated T cells, but at different phases of immune response.[7]
Current clinical trials are evaluating anti-PD-1 and PD-L1 drugs in combination with other immunotherapy drugs blocking LAG3, B7-H3, KIR, OX40, PARP, CD27, and ICOS.[7]
Therapeutics
PD-1
Pembrolizumab (Keytruda, formerly MK-3475 and lambrolizumab) was developed by Merck and first approved by the Food and Drug Administration in 2014 for the treatment of melanoma. It was later approved for metastatic non-small cell lung cancer and head and neck squamous cell carcinoma. In 2017, it became the first immunotherapy drug approved for use based on the genetic mutations of the tumor rather than the site of the tumor. It was shown that patients with higher non-synonymous mutation burden in their tumors respond better to the treatment. Both their objective response rate and progression-free survival was shown to be higher than in patients with low non-synonymous mutation burden.[12]
Nivolumab (Opdivo) was developed by Bristol-Myers Squibb and first approved by the FDA in 2014 for the treatment of melanoma. It was later approved for squamous cell lung cancer, renal cell carcinoma, and Hodgkin's lymphoma.
Cemiplimab (Libtayo) was developed by Regeneron Pharmaceuticals and first approved by the FDA in 2018 for the treatment of cutaneous squamous cell carcinoma (CSCC) or locally advanced CSCC who are not candidates for curative surgery or curative radiation.
Dostarlimab (Jemperli) – was developed by GlaxoSmithKline and was first approved for the treatment of mismatch repair deficient (dMMR) recurrent or advanced endometrial cancer by the FDA in April of 2021.[13] On August 17, 2021, the FDA granted accelerated approval for the treatment of mismatch repair deficient (dMMR) recurrent or advanced solid tumors.[14]
Retifanlimab (Zynyz) was developed by Incyte and first granted accelerated approval by the FDA in March 2023 for the treatment of Merkel cell carcinoma (MCC).
Toripalimab (Loqtorzi) is a humanized IgG4 monoclonal antibody against PD-1 approved in China in 2018 and in the United States in 2023.[15][16][17]
Experimental
Currently, many PD-1 inhibitors are under development:[7]
- Vopratelimab (JTX-4014) by Jounce Therapeutics[18] As of 2020 entered Phase I trial[19]
- Spartalizumab (PDR001) is a PD-1 inhibitor developed by Novartis to treat both solid tumors and lymphomas, which as of 2018 has entered Phase III trials.[20][21][22]
- Camrelizumab (SHR1210) is an anti-PD-1 monoclonal antibody introduced by Jiangsu HengRui Medicine Co., Ltd. that recently received conditional approval in China for the treatment of relapsed or refractory classical Hodgkin lymphoma.[23]
- Sintilimab (IBI308), a human anti-PD-1 antibody developed by Innovent and Eli Lilly for patients with non-small cell lung cancer (NSCLC).[24]
- Tislelizumab (BGB-A317) is a humanized IgG4 anti–PD-1 monoclonal antibody in pivotal Phase 3 and Phase 2 clinical trials in solid tumors and hematologic cancers.[25]
- INCMGA00012 (MGA012) is a humanized IgG4 monoclonal antibody developed by Incyte and MacroGenics.[26]
- AMP-224 by AstraZeneca/MedImmune and GlaxoSmithKline[27]
- AMP-514 (MEDI0680) by AstraZeneca[28]
- Acrixolimab (YBL-006) by Y-Biologics[29]
PD-L1
Atezolizumab (Tecentriq) is a fully humanised IgG1 (immunoglobulin 1) antibody developed by Roche Genentech. In 2016, the FDA approved atezolizumab for urothelial carcinoma and non-small cell lung cancer.
Avelumab (Bavencio) is a fully human IgG1 antibody developed by Merck Serono and Pfizer. Avelumab is FDA approved for the treatment of metastatic merkel-cell carcinoma. It failed phase III clinical trials for gastric cancer.[30]
Durvalumab (Imfinzi) is a fully human IgG1 antibody developed by AstraZeneca. Durvalumab is FDA approved for the treatment of urothelial carcinoma and unresectable non-small cell lung cancer after chemoradiation.[31]
Experimental
At least two PD-L1 inhibitors are in the experimental phase of development.
- KN035 is the only PD-L1 antibody with subcutaneous formulation currently under clinical evaluations in the US, China, and Japan[32]
- Cosibelimab (CK-301) by Checkpoint Therapeutics is a PD-L1 inhibitor developed by Dana Farber, and is currently in Phase 3 trials for NSCLC[33]
- AUNP12 is a 29-mer peptide as the first peptic PD-1/PD-L1 inhibitor developed by Aurigene and Laboratoires Pierre Fabre that is being evaluated in clinical trial, following promising in vitro results.[34]
- CA-170, discovered by Aurigene/Curis as the PD-L1 and VISTA antagonist, was indicted as a potent small molecule inhibitor in vitro. Thus, the compound is currently under phase I clinical trial over mesothelioma patients.[35]
- BMS-986189 is a macrocyclic peptide discovered by Bristol-Myers Squibb of which the pharmacokinetics, safety and tolerability is currently being studied on healthy subjects.[36]
Combinational therapy
Combination with type I Interferons
PD-1/PD-L1 blockade therapy is not effective for all patients, as some may exhibit resistance. To overcome resistance, a strategy involving the combination of PD-1/PD-L1 inhibitors with type I interferons has emerged. The combination of PD-1/PD-L1 inhibitors and type I interferons has shown promise in preclinical and clinical studies (phases I and II). This combination therapy leads to increased infiltration and activation of T cells within tumors, the generation of memory T cells, and improved overall survival in both animal models and patients. Notably, this approach has demonstrated efficacy in melanoma and renal carcinoma patients. [37]
Adverse effects
Immunotherapies as a group have off-target effects and toxicities common to them. Some of these include interstitial pneumonitis, colitis, hepatitis, thyroiditis, skin reactions, low levels of platelets and white blood cells, inflammation of the brain or spinal cord, neuromuscular adverse events[38] including myositis, Guillain-Barré syndrome, myasthenia gravis; myocarditis and cardiac insufficiency, acute adrenal insufficiency, and nephritis.[7] The most common kidney related changes are acute interstitial nephritis, followed by glomerular diseases and then tubular damage.[39] The detailed mechanism of these adverse effects are not fully elucidated;[40] however, they are clearly different from known autoimmune diseases.[41] Immune-mediated adverse reactions are usually attributed to generalised dysregulation of T cells[42] or development of autoantibodies,[43] although memory T cell responses against occult viral infections might also play a role in some patients with advanced melanoma following combined PD-1/CTLA-4 blockade.[44]
When compared with standard chemotherapeutic agents, PD-1/PD-L1 inhibitors had a lower reported incidence of fatigue, sensory neuropathy, diarrhea, bone marrow suppression, loss of appetite, nausea, and constipation.[8]
See also
References
- ↑ Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, Iyer AK (23 August 2017). "PD-1 and PD-L1 Checkpoint Signaling Inhibition for Cancer Immunotherapy: Mechanism, Combinations, and Clinical Outcome". Frontiers in Pharmacology. 8: 561. doi:10.3389/fphar.2017.00561. PMC 5572324. PMID 28878676.
- ↑ Francisco LM, Sage PT, Sharpe AH (July 2010). "The PD-1 pathway in tolerance and autoimmunity". Immunological Reviews. 236: 219–42. doi:10.1111/j.1600-065X.2010.00923.x. PMC 2919275. PMID 20636820.
- ↑ Zhang YH, Tian M, Tang MX, Liu ZZ, Liao AH (September 2015). "Recent Insight into the Role of the PD-1/PD-L1 Pathway in Feto-Maternal Tolerance and Pregnancy". American Journal of Reproductive Immunology. 74 (3): 201–8. doi:10.1111/aji.12365. PMID 25640631. S2CID 206987352.
- ↑ Tanaka K, Albin MJ, Yuan X, Yamaura K, Habicht A, Murayama T, et al. (October 2007). "PDL1 is required for peripheral transplantation tolerance and protection from chronic allograft rejection". Journal of Immunology. 179 (8): 5204–10. doi:10.4049/jimmunol.179.8.5204. PMC 2291549. PMID 17911605.
- 1 2 3 4 Sunshine J, Taube JM (August 2015). "PD-1/PD-L1 inhibitors". Current Opinion in Pharmacology. 23: 32–8. doi:10.1016/j.coph.2015.05.011. PMC 4516625. PMID 26047524.
- ↑ "The Science of PD-1 and Immunotherapy". Dana-Farber Cancer Institute. 13 May 2015.
- 1 2 3 4 5 Iwai Y, Hamanishi J, Chamoto K, Honjo T (April 2017). "Cancer immunotherapies targeting the PD-1 signaling pathway". Journal of Biomedical Science. 24 (1): 26. doi:10.1186/s12929-017-0329-9. PMC 5381059. PMID 28376884.
- 1 2 3 Gong J, Chehrazi-Raffle A, Reddi S, Salgia R (January 2018). "Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations". Journal for Immunotherapy of Cancer. 6 (1): 8. doi:10.1186/s40425-018-0316-z. PMC 5778665. PMID 29357948.
- 1 2 3 Syn NL, Teng MW, Mok TS, Soo RA (December 2017). "De-novo and acquired resistance to immune checkpoint targeting". The Lancet. Oncology. 18 (12): e731–e741. doi:10.1016/s1470-2045(17)30607-1. PMID 29208439.
- ↑ Goldkuhle M, Dimaki M, Gartlehner G, Monsef I, Dahm P, Glossmann JP, et al. (July 2018). Cochrane Haematological Malignancies Group (ed.). "Nivolumab for adults with Hodgkin's lymphoma (a rapid review using the software RobotReviewer)". The Cochrane Database of Systematic Reviews. 2018 (7): CD012556. doi:10.1002/14651858.CD012556.pub2. PMC 6513229. PMID 30001476.
- ↑ Guha M (2014). "Immune checkpoint inhibitors bring new hope to cancer patients". The Pharmaceutical Journal.
- ↑ Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. (April 2015). "Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer". Science. 348 (6230): 124–8. doi:10.1126/science.aaa1348. PMC 4993154. PMID 25765070.
- ↑ "FDA grants accelerated approval to dostarlimab-gxly for DMMR endometrial cancer". FDA. 11 June 2021.
- ↑ "FDA grants accelerated approval to dostarlimab-gxly for DMMR advanced solid tumors". FDA. February 2022.
- ↑ "Toripalimab - Shanghai Junshi Biosciences - AdisInsight". adisinsight.springer.com. Retrieved 2019-08-25.
- ↑ Keam, S.J. (2019). "Toripalimab: First Global Approval". Drugs. 79 (5): 573–578. doi:10.1007/s40265-019-01076-2. PMID 30805896.
- ↑ "FDA approves toripalimab-tpzi for nasopharyngeal carcinoma". US Food and Drug Administration. October 27, 2023.
- ↑ "Our Pipeline | Jounce Therapeutics". Retrieved 2020-09-19.
- ↑ Jounce Therapeutics, Inc. (2020-09-02). "Phase 1 First in Human Study of Programmed Cell Death Receptor-1 (PD-1) Inhibitor Monoclonal Antibody (mAb) JTX-4014 in Adult Subjects With Advanced Refractory Solid Tumor Malignancies".
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Kopp-Kubel S (1978-04-01). "International Nonproprietary Names (INN) for pharmaceutical substances". Bulletin of the World Health Organization. 73 (3): 275–9. doi:10.1093/ajhp/35.4.477a. PMC 2486664. PMID 7614659.
- ↑ "PDR001". Immuno-Oncology News. 2017-10-25. Retrieved 2019-08-24.
- ↑ "NCI Drug Dictionary". National Cancer Institute. 2011-02-02. Retrieved 2019-08-24.
- ↑ Markham A, Keam SJ (August 2019). "Camrelizumab: First Global Approval". Drugs. 79 (12): 1355–1361. doi:10.1007/s40265-019-01167-0. PMID 31313098. S2CID 197422122.
- ↑ "Sintilimab - Eli Lilly/Innovent Biologics - AdisInsight". adisinsight.springer.com. Retrieved 2019-08-25.
- ↑ "Library Association-Annual Meeting". The Library. s1-1 (1): 215. 1889-01-01. doi:10.1093/library/s1-1.1.215-b. ISSN 0024-2160.
- ↑ "Incyte Press Release". investor.incyte.com. Retrieved 2020-04-20.
- ↑ "Study to Assess the Safety, Tolerability, and Pharmacokinetics of AMP-224 in Patients With Advanced Cancer". www.clinicaltrials.gov. Retrieved 2020-04-24.
- ↑ "AstraZeneca stops monotherapy study at centerpiece of $500M buyout". www.fiercebiotech.com. 2 February 2018. Retrieved 2020-04-24.
- ↑ kgi-admin (2023-02-24). "Acrixolimab by Y-Biologics for Solid Tumor: Likelihood of Approval". Pharmaceutical Technology. Retrieved 2023-03-07.
- ↑ Broderick JM (28 November 2017). "Avelumab Falls Short in Phase III Gastric Cancer Trial". OncLive.
- ↑ AstraZeneca press release, 19 February 2018
- ↑ Zhang F, Wei H, Wang X, Bai Y, Wang P, Wu J, et al. (December 2017). "Structural basis of a novel PD-L1 nanobody for immune checkpoint blockade". Cell Discovery. 3 (1): 17004. doi:10.1038/celldisc.2017.4. PMC 5341541. PMID 28280600.
- ↑ "Checkpoint Therapeutics to Participate in Two Upcoming Investor Conferences". finance.yahoo.com. 9 September 2021. Retrieved 2021-09-20.
- ↑ Juneja VR, McGuire KA, Manguso RT, LaFleur MW, Collins N, Haining WN, et al. (April 2017). "PD-L1 on tumor cells is sufficient for immune evasion in immunogenic tumors and inhibits CD8 T cell cytotoxicity". The Journal of Experimental Medicine. 214 (4): 895–904. doi:10.1084/jem.20160801. PMC 5379970. PMID 28302645.
- ↑ Okazaki T, Honjo T (April 2006). "The PD-1-PD-L pathway in immunological tolerance". Trends in Immunology. 27 (4): 195–201. doi:10.1016/j.it.2006.02.001. PMID 16500147.
- ↑ "Pharmacokinetics, Safety, Tolerability and Pharmacodynamics of BMS-986189 in Healthy Subjects - Full Text View - ClinicalTrials.gov". clinicaltrials.gov. 5 February 2018. Retrieved 2019-08-24.
- ↑ Razaghi, Ali; Durand-Dubief, Mickaël; Brusselaers, Nele; Björnstedt, Mikael (2023). "Combining PD-1/PD-L1 blockade with type I interferon in cancer therapy". Frontiers in Immunology. 14. doi:10.3389/fimmu.2023.1249330. ISSN 1664-3224. PMC 10484344. PMID 37691915.
- ↑ Johansen A, Christensen SJ, Scheie D, Højgaard JL, Kondziella D (April 2019). "Neuromuscular adverse events associated with anti-PD-1 monoclonal antibodies: Systematic review". Neurology. 92 (14): 663–674. doi:10.1212/WNL.0000000000007235. PMID 30850443. S2CID 73496636.
- ↑ Wanchoo R, Karam S, Uppal NN, Barta VS, Deray G, Devoe C, et al. (2017). "Adverse Renal Effects of Immune Checkpoint Inhibitors: A Narrative Review". American Journal of Nephrology. 45 (2): 160–169. doi:10.1159/000455014. PMID 28076863.
- ↑ Postow MA, Sidlow R, Hellmann MD (January 2018). "Immune-Related Adverse Events Associated with Immune Checkpoint Blockade". The New England Journal of Medicine. 378 (2): 158–168. doi:10.1056/NEJMra1703481. PMID 29320654. S2CID 5211582.
- ↑ Johnson DB, Sullivan RJ, Ott PA, Carlino MS, Khushalani NI, Ye F, et al. (February 2016). "Ipilimumab Therapy in Patients With Advanced Melanoma and Preexisting Autoimmune Disorders". JAMA Oncology. 2 (2): 234–40. doi:10.1001/jamaoncol.2015.4368. PMID 26633184.
- ↑ Oh DY, Cham J, Zhang L, Fong G, Kwek SS, Klinger M, et al. (March 2017). "Immune Toxicities Elicted by CTLA-4 Blockade in Cancer Patients Are Associated with Early Diversification of the T-cell Repertoire". Cancer Research. 77 (6): 1322–1330. doi:10.1158/0008-5472.CAN-16-2324. PMC 5398199. PMID 28031229.
- ↑ Young A, Quandt Z, Bluestone JA (December 2018). "The Balancing Act between Cancer Immunity and Autoimmunity in Response to Immunotherapy". Cancer Immunology Research. 6 (12): 1445–1452. doi:10.1158/2326-6066.CIR-18-0487. PMC 6281171. PMID 30510057.
- ↑ Hutchinson JA, Kronenberg K, Riquelme P, Wenzel JJ, Glehr G, Schilling HL, et al. (March 2021). "Virus-specific memory T cell responses unmasked by immune checkpoint blockade cause hepatitis". Nature Communications. 12 (1): 1439. Bibcode:2021NatCo..12.1439H. doi:10.1038/s41467-021-21572-y. PMC 7933278. PMID 33664251.