
Phonophoresis, also known as sonophoresis, is the method of using ultrasound waves to increase skin permeability in order to improve the effectiveness of transdermal drug delivery. This method intersects drug delivery and ultrasound therapy. By assisting transdermal drug delivery, phonophoresis can be a painless treatment and an alternative to a needle.
Background
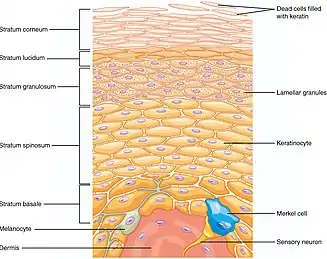
The primary purpose of phonophoresis is to assist in transdermal drug delivery, usually with the help of a coupling agent or medium. Transdermal drug delivery sometimes does not permeate the skin to reach a targeted area within the body because of the stratum corneum layer of the skin, a layer that prevents foreign substances from penetrating the body.[1][2][3] Transdermal drug delivery is patient-compliance,[4] usually avoids digestive system degradation,[5] and has the ability to use drugs with short half-lives.[6]
Treatment
Treatment methods
Phonophoresis can be performed using two main methods: The first is simultaneous treatment, where the drug can be applied at the same time as the ultrasound. The second method is pretreatment, where the ultrasound is used briefly before drug delivery.[5][6][7][4] This is to ensure that the skin is permeable prior to the drug being applied.
When using an ultrasound, cavities will develop due to the pressure change. Stable cavitation describes the repetitive oscillations of a cavity bubble, while inertial cavitation describes the collapse of a cavity bubble.[5] If the developed cavities fall apart, the effect on the stratum corneum lipids will increase the permeability of the skin.[6][3] These areas of increased permeability are often called localized transport regions, where there is lower electrical resistivity.[8] One potential method is to use cavitation seed at the surface of the skin.[9] Another potential method is to use ultrasound-responsive liquid-core nuclei (URLN).[3]
Frequency
Low-frequency ultrasound is seen as the optimal level of ultrasound frequency. This is typically characterized as 20 to 100 kHz (sometimes 18 to 100 kHz).[4] Low frequency makes cavitation more likely. For reference, high frequency ultrasound is typically in the range of 1 to 3 MHz.[5]
Coupling agents
The drug should be able to work together with the coupling agent.[6] In a 2019 study, they used the drug diclofenac in coordination with thiocolchioside gel to treat patients who suffer from acute lower back pain.[10] An application of a drug serving as a coupling agent is the use of piroxicam gel mixtures and dexamethasone sodium phosphate gel mixtures to treat patients who suffer from carpal tunnel syndrome.[11]
Applications
Physical conditions
Various conditions that can be addressed include cervical spine pain,[12] acute lower back pain,[10] carpal tunnel syndrome,[11] muscle injury,[13] rheumatoid arthritis,[14] and venous thrombosis.[2] Examples of drugs that have been used with sonophoresis include hydrocortisone, mannitol, dexamethasone, and lidocaine.[6]
Several products have been marketed to use phonophoresis for transdermal drug delivery.[6]
Other uses
A potential future application of phonophoresis is to use it with vaccines, as phonophoresis is considered a less painful alternative to needles.[8][6][4][1] Another potential use is in cancer therapeutics; one such application that has been explored is the delivery of cisplatin for patients who have cervical cancer.[15] Genetic skin diseases and wound healing may be assisted by phonophoresis.[6]
Risks
At an optimal frequency, phonophoresis will be painless and have minimal to no risk. The heat that is emitted from ultrasound use can also be damaging to the surface of the skin,[7] and cavitation can potentially lead to tissue damage.[7] Nanoparticle toxicity is another potential risk.[7]
References
- 1 2 Yang, Y., Xia, L., Ning, X., Hu, T., Xu, C., & Liu, W. (2021). "Enhanced Drug Permeation into Human Keloid Tissues by Sonophoresis-Assisted Microneedling". SLAL Technology. 26 (6): 660–666. doi:10.1177/24726303211024568. PMID 34219535. S2CID 235732832.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 Zhai, H., Zhang, C., Ou, H., & Chen, M. (2021). "Transdermal delivery of heparin using low- frequency sonophoresis in combination with sponge spicules for venous thrombosis treatment". Biomaterials Science. 9 (16): 5612–5625. doi:10.1039/D1BM00703C. PMID 34254062. S2CID 235809367.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 Donghee, P., Jongho, W., Gyounjung, L., Yongheum, L., Chul-Woo, K., & Jongbum, Seo. (2022). "Sonophoresis with ultrasound-responsive liquid-core nuclei for transdermal drug delivery". Skin Research and Technology. 28 (2): 291–298. doi:10.1111/srt.13129. PMC 9907662. PMID 35034386. S2CID 247599798.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 Lavon, I., & Kost, J. (2004). "Ultrasound and transdermal drug delivery". Drug Discovery Today. 9 (15): 670–676. doi:10.1016/S1359-6446(04)03170-8. PMID 15279850.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 Machet, L., & Boucaud, A. (2002). "Phonophoresis: efficiency, mechanisms and skin tolerance". International Journal of Pharmaceutics. 243 (1–2): 1–15. doi:10.1016/S0378-5173(02)00299-5. PMID 12176291.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 5 6 7 8 Rao, R., & Nanda, S. (2009). "Sonophoresis: recent advancements and future trends". Journal of Pharmacy and Pharmacology. 61 (6): 689–705. doi:10.1211/jpp.61.06.0001. PMID 19505359. S2CID 4247361.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 Seah, B., & Teo, B. (2018). "Recent advances in ultrasound-based transdermal drug delivery". International Journal of Nanomedicine. 13: 7749–7763. doi:10.2147/IJN.S174759. PMC 6251463. PMID 30538456.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 Ogura, M., Paliwal, S., & Mitragotri, S. (2008). "Low-frequency sonophoresis: Current status and future prospects". Advanced Drug Delivery Reviews. 60 (10): 1218–1223. doi:10.1016/j.addr.2008.03.006. PMID 18450318.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Donghee, P., Jongho, W., Unchul, S., Hyeon, P., Gillsoo, S., Jiyoung, J., Hyunjin, P., Chul Woo, K., & Jong Bum, Seo. (2019). "Transdermal Drug Delivery Using a Specialized Cavitation Seed for Ultrasound". IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control. 66 (6): 1057–1064. doi:10.1109/TUFFC.2019.2907702. PMID 30946663. S2CID 96432587.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 Altan, L., Kasapoglu Aksoy, M., & Kosegil Ozturk, E. (2019). "Efficacy of diclofenac & thiocolchioside gel phonophoresis comparison with ultrasound therapy on acute low back pain; a prospective, double-blind, randomized clinical study". Ultrasonics. 91: 201–205. doi:10.1016/j.ultras.2018.08.008. PMID 30139568. S2CID 52076491.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 Boonhong, J., & Thienkul, W. (2019). "Effectiveness of Phonophoresis Treatment in Carpal Tunnel Syndrome: A Randomized Double-blind, Controlled Trial". PM&R. 12 (1): 8–15. doi:10.1002/pmrj.12171. PMID 31006972. S2CID 128352578.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Aiyegbusi, A.I., Sanni, H.O., & Akinbo, S.R. (2019). "Intrasound Therapy: An Effective Alternative to Sodium Diclofenac Phonophoresis in the Management of Mechanical Chronic Cervical Spine Pain". Journal of Applied Sciences and Environmental Management. 23 (2): 371. doi:10.4314/jasem.v23i2.26. S2CID 86999653.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Haupenthal, D., Zortea, D., Zaccaron, R., Silveira, G., Correa, M., Mendes, C., Casagrande, L., Duarte, M., Pinho, R., Feuser, P., Avila, R., and Silveira, P. (2020). "Effects of phonophoresis with diclofenac linked gold nanoparticles in model of traumatic muscle injury". Materials Science and Engineering. 110: 110681. doi:10.1016/j.msec.2020.110681. PMID 32204109. S2CID 212931024.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Vaidya, J., & Shende, P. (2020). "Potential of Sonophoresis as a Skin Penetration Technique in the Treatment of Rheumatoid Arthritis with Transdermal Patch". AAPS PharmSciTech. 21 (5): 180. doi:10.1208/s12249-020-01725-w. PMID 32601758. S2CID 220261137.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Ma, S., Liu, C., Zhang, T., Jiang, L., & Wang, R. (2020). "Sonophoresis Enhanced Transdermal Delivery of Cisplatin in the Xenografted Tumor Model of Cervical Cancer". OncoTargets and Therapy. 13: 889–902. doi:10.2147/OTT.S238126. PMC 6996214. PMID 32099393.
{{cite journal}}: CS1 maint: multiple names: authors list (link)