| Popliteal artery entrapment syndrome | |
|---|---|
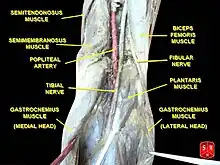 | |
| Normal course of the popliteal artery at the back of the knee | |
| Symptoms | Numbness, discoloration, absent pulses, coolness |
| Complications | Distal artery stenosis, limb amputation, arterial thromboembolism |
| Duration | Chronic |
| Causes | Congenital or functional |
| Risk factors | Young athlete males. |
| Treatment | Open surgical decompression |
| Prognosis | Favorable |
The popliteal artery entrapment syndrome (PAES) is an uncommon pathology that occurs when the popliteal artery is compressed by the surrounding popliteal fossa myofascial structures.[1] This results in claudication and chronic leg ischemia. This condition mainly occurs more in young athletes than in the elderlies.[2] Elderlies, who present with similar symptoms, are more likely to be diagnosed with peripheral artery disease with associated atherosclerosis.[2] Patients with PAES mainly present with intermittent feet and calf pain associated with exercises and relieved with rest.[3] PAES can be diagnosed with a combination of medical history, physical examination, and advanced imaging modalities such as duplex ultrasound, computer tomography, or magnetic resonance angiography. Management can range from non-intervention to open surgical decompression with a generally good prognosis.[4] Complications of untreated PAES can include stenotic artery degeneration, complete popliteal artery occlusion, distal arterial thromboembolism, or even formation of an aneurysm.
History
In 1879, the syndrome was first described in a 64 years old male by Anderson Stuart, a medical student.[1] In 1959, Hamming and Vink first described the management of the PAES in a 12-year-old patient. The patient was treated with myotomy of the medial head of the gastrocnemius muscle and concomitant endarterectomy of the popliteal artery. They later reported four more cases and claimed that the incidence of this pathology in patients younger than 30 years old with claudication was 40%. Servello was the first to draw attention to diminished distal pulses observed with forced plantar- or dorsiflexion in patients with this syndrome.[5] In 1981, Bouhoutsos and Daskalakis reported 45 cases of this syndrome in a population of 20,000 Greek soldiers.[6] Over the last few decades, the increasing frequency with which popliteal artery entrapment is reported, strongly suggests greater awareness of the syndrome.[7]
Epidemiology
In the general population, popliteal artery entrapment syndrome (PAES) has an estimated prevalence of 0.16%.[8] It is most commonly found in young, physically active males.[2] In fact, sixty percent of all cases of this syndrome occur in athletically active males under the age of 30.[9] The predilection of this syndrome presents in a male to female ratio of 15:1.[8] This discrepancy in prevalence may be overestimated due the findings that males are generally found to be more physically active than females or because a large portion of the data is from military hospitals that treat mostly male populations.[9] People, who participate in running, soccer, football, basketball, or rugby, are at increased risk.[10]
Newborns and young children are also at increased PAES risk due to congenital causes. During embryonic development, the medial head of gastrocnemius migrates medially and superiorly. This migration can cause structural abnormalities, such as irregular positioning of the popliteal artery, and can account for the rare instances of entrapment caused by the popliteus muscle.[9] Less than 3% of all people are born with this anatomical defect that progresses into PAES, and of those who are born with the anatomical defect, the majority never develop symptoms.[10] Bilateral presentation of PAES is found in approximately 30% of cases.[11]
Pathophysiology and classification
PAES can be classified as either congenital or functional.[3] Analysis of human embryological development has shown that the popliteal artery and the medial head of the gastrocnemius muscle arise at approximately the same time. Because of that, abnormal development of muscle's position in relation to the nearby vessels can result in potential vascular compromise.[3] The varying types of PAES can be classified based on aberrant migration and resultant attachments of the medial head of the gastrocnemius muscle. Type VI PAES (functional PAES) describes a subtype that is due to repeated microtrauma resulting in the destruction of the internal elastic lamina and damage to the smooth muscles resulting in fibrosis and scar formation.
| Type I | The popliteal artery courses more medially around a normally positioned medial head of the gastrocnemius muscle.[3] |
| Type II | The medial head of the gastrocnemius muscle attaches more laterally to the femur.[3] |
| Type III | Aberrant additional tendon of the gastrocnemius muscle encircles a normally positioned popliteal artery.[3] |
| Type IV | The popliteal artery is compressed by the popliteus muscle or a fibrous brand.[3] |
| Type V | The compression of both the popliteal artery and vein by any of the above causes.[3] |
| Type VI | The normally positioned popliteal artery is entrapped by the gastrocnemius muscle hypertrophy.[3] |
Additionally, a more practical classification system was introduced by Heidelberg et al.[12] This system classifies PAES into three main types:
Medical history and physical examination
Patients with PAES are typically healthy young males without previous history of cardiovascular risk factors such as smoking, hypertension, hypercholesterolemia, or diabetes.[13] Typically, patients present with intermittent claudication that is worsened with exercise and relieved with rest.[3] Associated symptoms include numbness, discoloration, pallor, and coolness in the affected lower extremity.[13] Physical examination of suspected PAES may show hypertrophy of the calf muscles, as well as diminished, unequal, or absent pulses in the lower extremity upon plantar- or dorsiflexion.[14]
Diagnosis
Differential diagnosis
- Chronic exertional compartment syndrome: Chronic pain and swelling of the affected muscle secondary to increase intramuscular pressure during exercise.[15]
- Unresolved muscle strain: An injury or damage to the muscle or its attaching tendons.[16]
- Medial tibial stress syndrome: Pain occurs over the shin bone (the tibia) with running or other sport-related activity.[17]
- Fibular and tibial stress fracture: Non-displaced microscopic fracture of the fibular and tibia occurs in many athletes, especially runners, and also in non-athletes who suddenly increase their activity level.[18]
- Fascial defects: The protrusion of the muscle through the surrounding fascia leads to pain and swelling of the area.[19]
- Sciatic nerve entrapment syndrome: The sciatic nerve becomes entrapped by muscles or other structures.[20]
- Vascular claudication (secondary to atherosclerosis): The obstruction of arterial flow leads to muscular ischemia and causes pain in the buttock and calf. More common in the elderly with cardiovascular risk factors.[21]
- Lumbar disc herniation: A bulging disc or a herniated disc in the lower back which causes radiating pain from the buttock into the leg and sometimes into the foot.[22]
Evaluation

PAES should be suspected in young healthy male patients with clinical symptoms consistent with compression of the vascular structures and without significant cardiovascular risk factors such as smoking.[13] Multiple imaging modalities are used to confirm the diagnosis of PAES.[23] Based on a systemic review by Sinha et al, digital subtraction angiography (DSA) is the most common imaging used for PAES diagnosis, followed by ankle–brachial index (18 percent), computed tomography angiography (CTA) (12 percent), magnetic resonance angiography (MRA) (12 percent), duplex ultrasonography (DU) (10 percent), exercise ankle-brachial index (4 percent), and other modalities (4 percent).[23] According to a recent study by Willimas et al, a combination of DU and MRA is far superior in diagnosing PAES.[24]
Provocative maneuvers can be used to improve visualization of PAES on the imagines.[25] The patient is initially positioned supine with the legs straight, and then instructed to forcefully plantar-flex. A plantarflexion force of 0 to 70 percent maximum has been shown to maximize the sensitivity and specificity for PAES diagnosis.[25] The DU can be a quick, inexpensive, and noninvasive initial screening for PAES. Flow velocities in the popliteal artery will increase, as the popliteal artery is compressed, which is reflected on the DU. If DU is negative but there is still strong suspicion for PAES, MRA or CTA with provocative maneuvers are needed as follow-up imaging. MRA would demonstrate a focal occlusion or narrowing of the mid-popliteal artery, post-stenotic dilatation, or aneurysm of the distal popliteal artery. If MRA or CTA is[13] non-conclusive, DSA may be used as a further option with a high sensitivity (> 97%) for PAES diagnosis.[23]
Additionally, functional PAES in which the gastrocnemius hypertrophy causes arterial compression during exercise can be best evaluated with dynamic CT.[23] For dynamic CT, initial images are taken with the patient still. Further images are taken following a series of provocative maneuvers.
Management
- Asymptomatic patients: the management is typically expectant. PAES may be found incidentally on the imaging, but the patient may be symptom-free, thus, no intervention is required.[13]
- Symptomatic patients: open surgical decompression is the mainstay of treatment for PAES.[26] The release of entrapment is achieved by performing division of the medial head of the gastrocnemius or musculotendinous band. The surgery can be performed with either posterior or medical approaches. Previous studies show a medial approach is beneficial for type I and II while a posterior approach is better for type III and IV.[4] Additionally, the use of Botulinum Toxin A has been used as an alternative noninvasive treatment for functional PAES.[27] A diagnosis of functional PAES is made if symptoms are improved after Botulinum injection. However, If symptoms are persisted, the patient can undergo an additional Botulinum injection or proceed with surgical decompression.[27]
The outcome following the surgery is usually favorable. Successful resolution of PAES occurs in 77 percent of cases.[23] Surgical complications include deep vein thrombosis, hematoma, wound infection, or seroma.[23] After the surgery, patient is usually monitored using arterial duplex ultrasonography 1, 3, 6, and 12 months, and annually after that.[3]
Complications of untreated PAES
Early detection and management of PAES can lead to a favorable outcome.[23] However, prolonged compression of popliteal artery can lead to extensive arterial damage and permanent claudication or limb loss.[28] Complications of PAES may include:[13]
- Distal arterial thromboembolism.
- Popliteal artery thrombosis.
- Popliteal artery stenosis.
- Limbs amputation.
Nonetheless, the course of PAES is often slow and takes time, thus, limbs loss is rarely seen, even in PAES patients.[13]
References
- 1 2 Gokkus, Kemal; Sagtas, Ergin; Bakalim, Tamer; Taskaya, Ertugrul; Aydin, Ahmet Turan (2014-07-14). "Popliteal entrapment syndrome. A systematic review of the literature and case presentation". Muscles, Ligaments and Tendons Journal. 4 (2): 141–148. doi:10.32098/mltj.02.2014.09. ISSN 2240-4554. PMC 4187583. PMID 25332925.
- 1 2 3 Sharma, Aditya (2014). "Conditions Presenting with Symptoms of Peripheral Arterial Disease". Seminars in Interventional Radiology. 31 (4): 281–291. doi:10.1055/s-0034-1393963. PMC 4232436. PMID 25435652.
- 1 2 3 4 5 6 7 8 9 10 11 Júnior, Francisco Cialdine Frota Carneiro; Carrijo, Eduardo Nazareno dos Anjos; Araújo, Samuel Tomaz; Nakano, Luis Carlos Uta; de Amorim, Jorge Eduardo; Cacione, Daniel Guimarães (2018-01-09). "Popliteal Artery Entrapment Syndrome: A Case Report and Review of the Literature". The American Journal of Case Reports. 19: 29–34. doi:10.12659/AJCR.905170. ISSN 1941-5923. PMC 5769514. PMID 29311538.
- 1 2 Gourgiotis, Stavros; Aggelakas, John; Salemis, Nikolaos; Elias, Charalabos; Georgiou, Charalabos (February 2008). "Diagnosis and surgical approach of popliteal artery entrapment syndrome: a retrospective study". Vascular Health and Risk Management. 4 (1): 83–88. doi:10.2147/vhrm.2008.04.01.83. ISSN 1176-6344. PMC 2464757. PMID 18629362.
- ↑ Servello, Manfredi (1962-11-01). "Clinical Syndrome of Anomalous Position of the Popliteal Artery". Circulation. 26 (5): 885–890. doi:10.1161/01.CIR.26.5.885. PMID 13988163. S2CID 261140.
- ↑ Bouhoutsos, J; Daskalakis, E (July 1981). "Muscular abnormalities affecting the popliteal vessels". British Journal of Surgery. 68 (7): 501–506. doi:10.1002/bjs.1800680720. PMID 7248723. S2CID 44852078.
- ↑ Stager, Andrew; Clement, Douglas (1999-07-01). "Popliteal Artery Entrapment Syndrome". Sports Medicine. 28 (1): 61–70. doi:10.2165/00007256-199928010-00006. ISSN 1179-2035. PMID 10461713. S2CID 26958095.
- 1 2 "Popliteal Artery Occlusive Disease: Background, Problem, Epidemiology". 2016-04-10.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 Stager, Andrew; Clement, Douglas (2012-09-23). "Popliteal Artery Entrapment Syndrome". Sports Medicine. 28 (1): 61–70. doi:10.2165/00007256-199928010-00006. ISSN 0112-1642. PMID 10461713. S2CID 26958095.
- 1 2 "Popliteal Artery Entrapment Syndrome (PAES) | Cleveland Clinic". Cleveland Clinic. Retrieved 2016-12-19.
- ↑ Drigny, Joffrey; Reboursière, Emmanuel; Desvergée, Antoine; Ruet, Alexis; Hulet, Christophe (June 2019). "Concurrent Exertional Compartment Syndrome and Functional Popliteal Artery Entrapment Syndrome: A Case Report". PM&R. 11 (6): 669–672. doi:10.1002/pmrj.12081. ISSN 1934-1482. PMID 30689303. S2CID 195661793.
- 1 2 3 4 Papaioannou, S; Tsitouridis, K; Giataganas, G; Rodokalakis, G; Kyriakou, V; Papastergiou, Ch; Arvaniti, M; Tsitouridis, I (2009). "Evaluation of popliteal arteries with CT angiography in popliteal artery entrapment syndrome". Hippokratia. 13 (1): 32–37. ISSN 1108-4189. PMC 2633250. PMID 19240818.
- 1 2 3 4 5 6 7 Davis, Donald D.; Shaw, Palma M. (2022), "Popliteal Artery Entrapment Syndrome", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28722994, retrieved 2022-12-04
- ↑ "ClinicalKey". www.clinicalkey.com. Retrieved 2022-12-04.
- ↑ Bong MR, Polatsch DB, Jazrawi LM et al. Chronic exertional compartment syndrome: diagnosis and management.Bull Hosp Jt Dis. 2005;62(3-4):77-84.
- ↑ Noonan, Thomas J.; Garrett, William E. Jr (July 1999). "Muscle Strain Injury: Diagnosis and Treatment". JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 7 (4): 262–269. doi:10.5435/00124635-199907000-00006. ISSN 1067-151X. PMID 10434080.
- ↑ McClure, Charles J.; Oh, Robert (2022), "Medial Tibial Stress Syndrome", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30860714, retrieved 2022-12-04
- ↑ "UpToDate". www.uptodate.com. Retrieved 2022-12-04.
- ↑ Dyson, Kathryn; Palan, Jeya; Mangwani, Jitendra (2019). "Bilateral non-traumatic lower leg fascial defects causing peroneal muscle herniation and novel use of a GraftJacket to repair the fascial defect". Journal of Clinical Orthopaedics and Trauma. 10 (5): 879–883. doi:10.1016/j.jcot.2018.09.009. ISSN 0976-5662. PMC 6739491. PMID 31528061.
- ↑ Hicks, Brandon L.; Lam, Jason C.; Varacallo, Matthew (2022), "Piriformis Syndrome", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28846222, retrieved 2022-12-04
- ↑ "UpToDate". www.uptodate.com. Retrieved 2022-12-04.
- ↑ Al Qaraghli, Mustafa I.; De Jesus, Orlando (2022), "Lumbar Disc Herniation", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32809713, retrieved 2022-12-04
- 1 2 3 4 5 6 7 Sinha, Sidhartha; Houghton, Jon; Holt, Peter J.; Thompson, Matt M.; Loftus, Ian M.; Hinchliffe, Robert J. (2012-01-01). "Popliteal entrapment syndrome". Journal of Vascular Surgery. 55 (1): 252–262.e30. doi:10.1016/j.jvs.2011.08.050. ISSN 0741-5214. PMID 22116047.
- ↑ Williams, Charles; Kennedy, Dominic; Bastian-Jordan, Matthew; Hislop, Matthew; Cramp, Brendan; Dhupelia, Sanjay (September 2015). "A new diagnostic approach to popliteal artery entrapment syndrome". Journal of Medical Radiation Sciences. 62 (3): 226–229. doi:10.1002/jmrs.121. ISSN 2051-3895. PMC 4592677. PMID 26451245.
- 1 2 Hislop, Matthew; Kennedy, Dominic; Cramp, Brendan; Dhupelia, Sanjay (2014). "Functional Popliteal Artery Entrapment Syndrome: Poorly Understood and Frequently Missed? A Review of Clinical Features, Appropriate Investigations, and Treatment Options". Journal of Sports Medicine. 2014: 105953. doi:10.1155/2014/105953. ISSN 2356-7651. PMC 4590902. PMID 26464888.
- ↑ Dovell, G; Hinchliffe, RJ (January 2018). "Surgery for popliteal artery entrapment syndrome: use of an intraoperative tibial nerve stimulator and duplex ultrasound". Annals of the Royal College of Surgeons of England. 100 (1): 78–79. doi:10.1308/rcsann.2017.0099. ISSN 0035-8843. PMC 5838662. PMID 29022807.
- 1 2 "ClinicalKey". www.clinicalkey.com. Retrieved 2022-12-04.
- ↑ Shahi, Niti; Arosemena, Mariano; Kwon, Jeontaik; Abai, Babak; Salvatore, Dawn; DiMuzio, Paul (2019-08-01). "Functional Popliteal Artery Entrapment Syndrome: A Review of Diagnosis and Management". Annals of Vascular Surgery. 59: 259–267. doi:10.1016/j.avsg.2018.12.105. ISSN 0890-5096. PMID 31028851. S2CID 135466438.