RET inhibitors are targeted therapies that act on tumors with activating alterations in the RET proto-oncogene, such as point mutations or fusions. They fall under the category of the tyrosine kinase inhibitors, which work by inhibiting proteins involved in the abnormal growth of cancer cells. Existing molecules fall in two main categories: the older multikinase inhibitors and the more recent selective inhibitors. Although RET alterations are found at low frequency in a broad range of tumors, the three main indications for RET inhibitors today are non-small cell lung cancer (which harbor RET fusions at a frequency of 1-2%), medullary thyroid cancer (MTC, with activating RET mutations in 25% of cases) and papillary thyroid cancer (PTC, with up to 80% prevalence of fusions depending on the region). As of 2020, up to 48 fusion partners have been catalogued in NSCLC rearrangements, with KIF5B and CCDC6 being the most prevalent. [1] At least 10 different fusion variants have been described for KIF5B-RET, each with different breakpoints within the partner gene, but unclear clinical impact as of 2018. [2]
Multikinase inhibitors
Multikinase inhibitors are molecules that possess a broad range of targets along with RET. These included cabozantinib, lenvatinib, sunitinib and alectinib. Since they were not designed to bind RET specifically, these inhibitors have other targets such as VEGFR, c-MET, and c-KIT. Among them, the VEGFR-related toxicities commonly precluded patients from achieving therapeutic doses with these medications, resulting in incomplete inhibition of RET and suboptimal clinical outcomes. In NSCLC, overall response rates (ORR) were low (16% for lenvatinib, [3] 28% for cabozantinib [4]), and progression-free survival (PFS) hovered around 6 months with a very high percentage of patients requiring dose reductions or discontinuing treatment (73% of patients on cabozantinib). Resistance to these medications included on-target mutations on the V804 gatekeeper residue, [5] as well as off-target mechanisms such as EGFR pathway activation and MDM2 amplifications. [6] Differences in efficacy also arose depending on the fusion partner, with non-KIF5B fusions typically responding better to these multikinase inhibitors than KIF5B-RET-driven tumors.
Compared to the much higher response rates and longer progression-free survivals achieved by selective inhibitors in other kinase fusions such as ALK or ROS1, these molecules offered much more limited clinical benefit, which highlighted a critical need for highly selective RET inhibitors.
Selective RET inhibitors
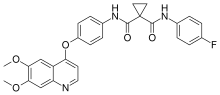
Around 2017, the first selective RET inhibitors selpercatinib (LOXO-292) and pralsetinib (BLU-667) started their first phase I/II clinical trials in solid tumors. They were designed to have high potency for RET, along with low affinity for other related targets such as VEGFR-family kinases to limit off-target toxicities. They were also designed to overcome the V804 gatekeeper mutations that some patients acquired under multikinase inhibitors. In patients who had previously received platinum chemotherapies for their lung cancers, ORRs hovered around 60% with median PFS between 17 months and not-evaluable (NE). [7] [8] Similar promising results came out for thyroid cancers as well, with response rates at 70-80% and median PFS between 18 and 22 months. [9] The encouraging results of the phase I/II trials led to the FDA approvals of selpercatinib (Retevmo™) for RET-driven NSCLC, MTC and PTC in May 2020, and the approval of pralsetinib (Gavreto™) for RET-fusion NSCLC in September 2020, as well as MTC and PTC in December 2020.
Resistance mechanisms to this first generation of selective RET inhibitors include different on-target mutations on the G810 solvent-front residue, [10] as well as off-target alterations such as MET amplifications and KRAS mutations among others. TP53 mutational status appears to have an impact on prognosis and resistance mechanisms, with TP53-mutated tumors showing shorter PFS and mostly off-target resistance mechanisms. [11]
Investigational therapies
Single-compounds
Several other molecules are currently being investigated as selective RET inhibitors. Boston Therapeutics' BOS172738 seemingly falls in the same category as the approved first-generation inhibitors, with selectivity against VEGFR2, similar clinical activity, and susceptibility to the G810 resistance mutation.[12] Turning Point Therapeutics' TPX-0046 is a compound that is claimed to target the G810 mutation, as well as Src family kinases, but is susceptible to the gatekeeper V804 mutation.[13] Other compounds include Helsinn's HM06, which presented data in October 2021 showing significant activity against both the G810 and V804 mutations individually, making it a brain-penetrant second-generation RET inhibitor for which a clinical trial is open in the US since February 2021.
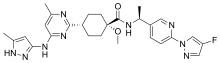
In 2021, Eli Lilly announced preclinical results for LOX-18228 and LOX-19260, two next-generation RET inhibitor candidates capable of tackling the G810 and V804 mutations individually as well as in tandem (G810+V804). The study looked at cell lines and mouse models with KIF5B-RET and CCDC6-RET fusions, as well as lines with the M918T mutation. The compounds showed strong selectivity and efficacy across cells lines. The company renamed one of these candidates LOXO-260, for which a Phase I clinical trial is expected in Q1 2022.[14]
Combinations
While selective inhibitors are not yet (as of 2021) being evaluated in combination with other compounds to treat therapy-naïve patients, they are still being investigated to treat RET fusions arising as resistance mechanisms to other treatments. Notably, around 5% of EGFR-mutated non-small-cell lung cancers develop RET fusions as a resistance mechanism to the third-generation EGFR inhibitor osimertinib. [15] For these patients, the combination of osimertinib and selpercatinib is currently being evaluated in a cohort of the ORCHARD study. [16]
Discontinued compounds
Among older compounds being investigated for RET inhibition, RXDX-105 was being developed by Ignyta as a VEGF-sparing multikinase inhibitor of BRAF, RET and EGFR. It was discontinued after acquisition of the company by Hoffmann-La Roche, citing a poor efficacy profile compared to the selective inhibitors being developed parallel to it. While it boasted a 75% response rate among fusions with non-KIF5B partners (6 out of 8 patients), there were no responses for patients with the KIF5B fusion partner (0 out of 20 patients), which represents more than 65% of RET fusions in NSCLC. [17] Among cited reasons for this difference is the KIF5B promoter inducing higher expression of the KIF5B-RET fusion protein compared to other partners, which would result in incomplete inhibition at clinical doses of RXDX-105 and reduced therapeutic activity.
Diagnostics
In order to identify patients most likely to benefit from RET inhibitors, several companion diagnostic assays are approved. Regardless of the alteration, tissue-based NGS remains the gold standard with very high specificity and sensitivity. In the case of rearrangements, RT-PCR is a proven technique with high specificity and sensitivity, but it will miss fusions with rare partners. FISH can be used where other techniques are not available, but the relative subjectivity of the test along with the proximity of common partners to the RET gene can make it difficult to discern rearrangements. Plasma-based NGS assays are becoming more and more prevalent because of their ease of use and high specificity, although they are limited by how much circulating tumor DNA is present in the sample, which itself depends upon how much DNA the tumors shed into the blood. This means that while a positive result may be taken as certainty, a negative result might simply mean not enough material was collected, and should be confirmed with another technique to rule out a false-negative.
References
- ↑ Ou, Sai-Hong Ignatius; Zhu, Viola W. (2020). "Catalog of 5′ fusion partners in RET+ NSCLC Circa 2020". JTO Clinical and Research Reports. 1 (2): 100037. doi:10.1016/j.jtocrr.2020.100037. ISSN 2666-3643. PMC 8474217. PMID 34589933.
- ↑ Ferrara, Roberto; Auger, Nathalie; Auclin, Edouard; Besse, Benjamin (2018). "Clinical and Translational Implications of RET Rearrangements in Non–Small Cell Lung Cancer". Journal of Thoracic Oncology. 13 (1): 27–45. doi:10.1016/j.jtho.2017.10.021. ISSN 1556-0864. PMID 29128428.
- ↑ Hida, Toyoaki; Velcheti, Vamsidhar; Reckamp, Karen L.; Nokihara, Hiroshi; Sachdev, Pallavi; Kubota, Tomoki; Nakada, Takuya; Dutcus, Corina E.; Ren, Min; Tamura, Tomohide (2019). "A phase 2 study of lenvatinib in patients with RET fusion-positive lung adenocarcinoma". Lung Cancer. 138: 124–130. doi:10.1016/j.lungcan.2019.09.011. ISSN 0169-5002. PMID 31710864.
- ↑ Drilon, Alexander; Rekhtman, Natasha; Arcila, Maria; Wang, Lu; Ni, Andy; Albano, Melanie; Van Voorthuysen, Martine; Somwar, Romel; Smith, Roger S; Montecalvo, Joseph; Plodkowski, Andrew; Ginsberg, Michelle S; Riely, Gregory J; Rudin, Charles M; Ladanyi, Marc; Kris, Mark G (2016). "Cabozantinib in patients with advanced RET -rearranged non-small-cell lung cancer: an open-label, single-centre, phase 2, single-arm trial". The Lancet Oncology. 17 (12): 1653–1660. doi:10.1016/S1470-2045(16)30562-9. ISSN 1470-2045. PMC 5143197. PMID 27825636.
- ↑ Wirth, Lori J.; Kohno, Takashi; Udagawa, Hibiki; Matsumoto, Shingo; Ishii, Genichiro; Ebata, Kevin; Tuch, Brian B.; Zhu, Edward Y.; Nguyen, Michele; Smith, Steve; Hanson, Lauren M.; Burkard, Michael R.; Cable, LouAnn; Blake, James F.; Condroski, Kevin R.; Brandhuber, Barbara J.; Andrews, Steve; Rothenberg, S. Michael; Goto, Koichi (2019). "Emergence and Targeting of Acquired and Hereditary Resistance to Multikinase RET Inhibition in Patients With RET-Altered Cancer". JCO Precision Oncology. 3 (3): 1–7. doi:10.1200/PO.19.00189. ISSN 2473-4284. PMC 7446343. PMID 32923848.
- ↑ Bronte, Giuseppe; Ulivi, Paola; Verlicchi, Alberto; Cravero, Paola; Delmonte, Angelo; Crinò, Lucio (2019). "
Targeting RET-rearranged non-small-cell lung cancer: future prospects
". Lung Cancer: Targets and Therapy. 10: 27–36. doi:10.2147/LCTT.S192830. ISSN 1179-2728. PMC 6433115. PMID 30962732. S2CID 102347736. - ↑ Drilon, Alexander; Oxnard, Geoffrey R.; Tan, Daniel S.W.; Loong, Herbert H.F.; Johnson, Melissa; Gainor, Justin; McCoach, Caroline E.; Gautschi, Oliver; Besse, Benjamin; Cho, Byoung C.; Peled, Nir; Weiss, Jared; Kim, Yu-Jung; Ohe, Yuichiro; Nishio, Makoto; Park, Keunchil; Patel, Jyoti; Seto, Takashi; Sakamoto, Tomohiro; Rosen, Ezra; Shah, Manisha H.; Barlesi, Fabrice; Cassier, Philippe A.; Bazhenova, Lyudmila; De Braud, Filippo; Garralda, Elena; Velcheti, Vamsidhar; Satouchi, Miyako; Ohashi, Kadoaki; Pennell, Nathan A.; Reckamp, Karen L.; Dy, Grace K.; Wolf, Jürgen; Solomon, Benjamin; Falchook, Gerald; Ebata, Kevin; Nguyen, Michele; Nair, Binoj; Zhu, Edward Y.; Yang, Luxi; Huang, Xin; Olek, Elizabeth; Rothenberg, S. Michael; Goto, Koichi; Subbiah, Vivek (2020). "Efficacy of Selpercatinib in RET Fusion–Positive Non–Small-Cell Lung Cancer". New England Journal of Medicine. 383 (9): 813–824. doi:10.1056/NEJMoa2005653. ISSN 0028-4793. PMC 7506467. PMID 32846060.
- ↑ FDA (9 September 2020). "FDA approves pralsetinib for lung cancer with RET gene fusions". fda.gov. Retrieved 15 October 2020.
- ↑ Wirth, Lori J.; Sherman, Eric; Robinson, Bruce; Solomon, Benjamin; Kang, Hyunseok; Lorch, Jochen; Worden, Francis; Brose, Marcia; Patel, Jyoti; Leboulleux, Sophie; Godbert, Yann; Barlesi, Fabrice; Morris, John C.; Owonikoko, Taofeek K.; Tan, Daniel S.W.; Gautschi, Oliver; Weiss, Jared; de la Fouchardière, Christelle; Burkard, Mark E.; Laskin, Janessa; Taylor, Matthew H.; Kroiss, Matthias; Medioni, Jacques; Goldman, Jonathan W.; Bauer, Todd M.; Levy, Benjamin; Zhu, Viola W.; Lakhani, Nehal; Moreno, Victor; Ebata, Kevin; Nguyen, Michele; Heirich, Dana; Zhu, Edward Y.; Huang, Xin; Yang, Luxi; Kherani, Jennifer; Rothenberg, S. Michael; Drilon, Alexander; Subbiah, Vivek; Shah, Manisha H.; Cabanillas, Maria E. (2020). "Efficacy of Selpercatinib in RET-Altered Thyroid Cancers". New England Journal of Medicine. 383 (9): 825–835. doi:10.1056/NEJMoa2005651. ISSN 0028-4793. PMC 10777663. PMID 32846061.
- ↑ Solomon, Benjamin J.; Tan, Lavinia; Lin, Jessica J.; Wong, Stephen Q.; Hollizeck, Sebastian; Ebata, Kevin; Tuch, Brian B.; Yoda, Satoshi; Gainor, Justin F.; Sequist, Lecia V.; Oxnard, Geoffrey R.; Gautschi, Oliver; Drilon, Alexander; Subbiah, Vivek; Khoo, Christine; Zhu, Edward Y.; Nguyen, Michele; Henry, Dahlia; Condroski, Kevin R.; Kolakowski, Gabrielle R.; Gomez, Eliana; Ballard, Joshua; Metcalf, Andrew T.; Blake, James F.; Dawson, Sarah-Jane; Blosser, Wayne; Stancato, Louis F.; Brandhuber, Barbara J.; Andrews, Steve; Robinson, Bruce G.; Rothenberg, S. Michael (2020). "RET Solvent Front Mutations Mediate Acquired Resistance to Selective RET Inhibition in RET-Driven Malignancies". Journal of Thoracic Oncology. 15 (4): 541–549. doi:10.1016/j.jtho.2020.01.006. ISSN 1556-0864. PMC 7430178. PMID 31988000.
- ↑ Lin, J.J.; Liu, S.V.; McCoach, C.E.; Zhu, V.W.; Tan, A.C.; Yoda, S.; Peterson, J.; Do, A.; Prutisto-Chang, K.; Dagogo-Jack, I.; Sequist, L.V.; Wirth, L.J.; Lennerz, J.K.; Hata, A.N.; Mino-Kenudson, M.; Nardi, V.; Ou, S.-H.I.; Tan, D.S.-W.; Gainor, J.F. (2020). "Mechanisms of Resistance to Selective RET Tyrosine Kinase Inhibitors in RET Fusion-Positive Non-Small Cell Lung Cancer". Annals of Oncology. 31 (12): 1725–1733. doi:10.1016/j.annonc.2020.09.015. ISSN 0923-7534. PMC 9538591. PMID 33007380.
- ↑ Schoffski, Patrick; Cho, Byoung Chul; Italiano, Antoine; Loong, Herbert H. F.; Massard, Christophe; Medina Rodriguez, Laura; Shih, Jin-Yuan; Subbiah, Vivek; Verlingue, Loic; Andreas, Karen; Basson, Craig T.; Clawson, Alicia; Ho, Peter T.C.; Knight, Shelley; Scheuber, Anita; Keegan, Mitchell (2021-05-20). "BOS172738, a highly potent and selective RET inhibitor, for the treatment of RET-altered tumors including RET-fusion+ NSCLC and RET-mutant MTC: Phase 1 study results". Journal of Clinical Oncology. American Society of Clinical Oncology (ASCO). 39 (15_suppl): 3008. doi:10.1200/jco.2021.39.15_suppl.3008. ISSN 0732-183X. S2CID 236336165.
- ↑ A. Drilon. "TPX-0046 is a novel and potent RET/SRC inhibitor for RET-driven cancers" (PDF). tptherapeutics.com. Retrieved 15 October 2020.
- ↑ Kolakowski, Gabrielle R. (10 April 2021). "Pre-clinical characterization of potent and selective next-generation RET inhibitors". Aacr 2021 (Session PO.ET06.07). Retrieved 14 March 2021.
- ↑ Rich, Thereasa A.; Reckamp, Karen L.; Chae, Young Kwang; Doebele, Robert C.; Iams, Wade T.; Oh, Michael; Raymond, Victoria M.; Lanman, Richard B.; Riess, Jonathan W.; Stinchcombe, Thomas E.; Subbiah, Vivek; Trevarthen, David R.; Fairclough, Stephen; Yen, Jennifer; Gautschi, Oliver (2019). "Analysis of Cell-Free DNA from 32,989 Advanced Cancers Reveals Novel Co-occurring Activating RET Alterations and Oncogenic Signaling Pathway Aberrations". Clinical Cancer Research. 25 (19): 5832–5842. doi:10.1158/1078-0432.CCR-18-4049. ISSN 1078-0432. PMC 6774853. PMID 31300450. S2CID 196349232.
- ↑ "Phase 2 Platform Study in Patients With Advanced Non-Small Lung Cancer Who Progressed on First-Line Osimertinib Therapy (ORCHARD) - Full Text View - ClinicalTrials.gov". clinicaltrials.gov. Retrieved 20 October 2020.
- ↑ Drilon, Alexander; Fu, Siqing; Patel, Manish R.; Fakih, Marwan; Wang, Ding; Olszanski, Anthony J.; Morgensztern, Daniel; Liu, Stephen V.; Cho, Byoung Chul; Bazhenova, Lyudmila; Rodriguez, Cristina P.; Doebele, Robert C.; Wozniak, Antoinette; Reckamp, Karen L.; Seery, Tara; Nikolinakos, Petros; Hu, Zheyi; Oliver, Jennifer W.; Trone, Denise; McArthur, Katherine; Patel, Rupal; Multani, Pratik S.; Ahn, Myung-Ju (2019). "A Phase I/Ib Trial of the VEGFR-Sparing Multikinase RET Inhibitor RXDX-105". Cancer Discovery. 9 (3): 384–395. doi:10.1158/2159-8290.CD-18-0839. ISSN 2159-8274. PMC 6397691. PMID 30487236.