The respiratory tract antimicrobial defense system is a layered defense mechanism which relies on components of both the innate and adaptive immune systems to protect the lungs and the rest of the respiratory tract against inhaled microorganisms.
In the first line of defense, inhaled bacteria are trapped by mucus and are swept toward the pharynx and are swallowed.[1] Bacteria which penetrate the mucous layer are dealt with a second line of defense which includes antimicrobial peptides that are secreted by the surface epithelium of the respiratory tract which kill many strains of bacteria.[2] Those bacteria that are resistant to antimicrobial peptides are killed by a variety of reactive oxygen species produced by phagocytes. In a third line of defense and as a last resort, persistent bacterial infections which escape the innate immune system are eliminated by the adaptive immune system.
Lactoferrin
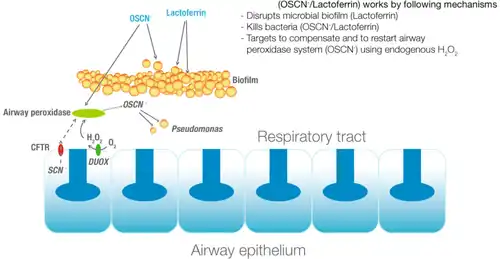
Lactoferrin (LF) is a multifunctional protein which is an essential part of the respiratory tract antimicrobial defense system.[3] LF proteolysis produces the small peptides lactoferricin and kaliocin-1 both with antimicrobial activity.[4]
Reactive oxygen species, oxygenated compounds
Phagocytes possess a superoxide-producing NADPH oxidase enzyme complex.[5] Other cells in the respiratory tract also produce superoxide and hydrogen peroxide through the activity of dual oxidase 2 proteins, also known as Duox2.[6][7]
The superoxide generated by these enzymes complexes dismutates into hydrogen peroxide which in turn is used by myeloperoxidase to produce bactericidal hypochlorous acid.[8] In addition, the submucosal glands of the respiratory tract secrete myeloperoxidase and lactoperoxidase (LPO)[9] that catalyzes the oxidation of thiocyanate and detoxify hydrogen peroxide or ROS to the antimicrobial hypothiocyanite.[10][11]
The oxygenated compounds produced by the lactoperoxidase system does not attack DNA and is not mutagenic and is known to be safe.[12] Hypothiocyanite generated through this pathway displays broad spectrum bactericidal activity including potent antibacterial action on H. pylori.[13]
Cystic fibrosis
Thiocyanate secretion[14] in cystic fibrosis patients is decreased resulting in a reduced production of the antimicrobial hypothiocyanite and consequently contributes to the increased risk of airway infection.[15][16]
Therapeutic applications
Lactoferrin with hypothiocyanite for the treatment of cystic fibrosis has been granted orphan drug status by the EMEA[17] and the FDA.[18]
References
- ↑ Boucher RC (January 2003). "Regulation of airway surface liquid volume by human airway epithelia". Pflügers Arch. 445 (4): 495–8. doi:10.1007/s00424-002-0955-1. PMID 12548395. S2CID 2831774.
- ↑ Ganz T (March 2002). "Antimicrobial polypeptides in host defense of the respiratory tract". J. Clin. Invest. 109 (6): 693–7. doi:10.1172/JCI15218. PMC 150915. PMID 11901174.
- ↑ Sánchez L, Calvo M, Brock JH (May 1992). "Biological role of lactoferrin". Arch. Dis. Child. 67 (5): 657–61. doi:10.1136/adc.67.5.657. PMC 1793702. PMID 1599309.
- ↑ Tomita M, Takase M, Bellamy W, Shimamura S (October 1994). "A review: the active peptide of lactoferrin". Acta Paediatr Jpn. 36 (5): 585–91. doi:10.1111/j.1442-200x.1994.tb03250.x. PMID 7825467. S2CID 29553971.
- ↑ Nauseef WM (October 2004). "Assembly of the phagocyte NADPH oxidase". Histochem. Cell Biol. 122 (4): 277–91. doi:10.1007/s00418-004-0679-8. PMID 15293055. S2CID 31639185.
- ↑ Thomas EL, Bates KP, Jefferson MM (September 1980). "Hypothiocyanite ion: detection of the antimicrobial agent in human saliva". J. Dent. Res. 59 (9): 1466–72. doi:10.1177/00220345800590090201. PMID 6931123. S2CID 7717994.
- ↑ Thomas EL, Aune TM (May 1978). "Lactoperoxidase, peroxide, thiocyanate antimicrobial system: correlation of sulfhydryl oxidation with antimicrobial action". Infect. Immun. 20 (2): 456–63. doi:10.1128/IAI.20.2.456-463.1978. PMC 421877. PMID 352945.
- ↑ Klebanoff SJ (May 2005). "Myeloperoxidase: friend and foe". J. Leukoc. Biol. 77 (5): 598–625. doi:10.1189/jlb.1204697. PMID 15689384.
- ↑ Wijkstrom-Frei C, El-Chemaly S, Ali-Rachedi R, Gerson C, Cobas MA, Forteza R, Salathe M, Conner GE (August 2003). "Lactoperoxidase and human airway host defense". Am. J. Respir. Cell Mol. Biol. 29 (2): 206–12. CiteSeerX 10.1.1.325.1962. doi:10.1165/rcmb.2002-0152OC. PMID 12626341.
- ↑ Conner GE, Salathe M, Forteza R (December 2002). "Lactoperoxidase and hydrogen peroxide metabolism in the airway". Am. J. Respir. Crit. Care Med. 166 (12 Pt 2): S57–61. doi:10.1164/rccm.2206018. PMID 12471090.
- ↑ Conner GE, Wijkstrom-Frei C, Randell SH, Fernandez VE, Salathe M (January 2007). "The Lactoperoxidase System Links Anion Transport To Host Defense in Cystic Fibrosis". FEBS Lett. 581 (2): 271–8. doi:10.1016/j.febslet.2006.12.025. PMC 1851694. PMID 17204267.
- ↑ White WE, Pruitt KM, Mansson-Rahemtulla B (February 1983). "Peroxidase-Thiocyanate-Peroxide Antibacterial System Does Not Damage DNA". Antimicrob. Agents Chemother. 23 (2): 267–72. doi:10.1128/aac.23.2.267. PMC 186035. PMID 6340603.
- ↑ Haukioja A, Ihalin R, Loimaranta V, Lenander M, Tenovuo J (September 2004). "Sensitivity of Helicobacter pylori to an innate defence mechanism, the lactoperoxidase system, in buffer and in human whole saliva". J. Med. Microbiol. 53 (Pt 9): 855–60. doi:10.1099/jmm.0.45548-0. PMID 15314191.
- ↑ Xu Y, Szép S, Lu Z (December 2009). "The antioxidant role of thiocyanate in the pathogenesis of cystic fibrosis and other inflammation-related diseases". Proc. Natl. Acad. Sci. U.S.A. 106 (48): 20515–9. doi:10.1073/pnas.0911412106. PMC 2777967. PMID 19918082.
- ↑ Moskwa P, Lorentzen D, Excoffon KJ, Zabner J, McCray PB, Nauseef WM, Dupuy C, Bánfi B (January 2007). "A Novel Host Defense System of Airways Is Defective in Cystic Fibrosis". Am. J. Respir. Crit. Care Med. 175 (2): 174–83. doi:10.1164/rccm.200607-1029OC. PMC 2720149. PMID 17082494.
- ↑ Minarowski Ł, Sands D, Minarowska A, Karwowska A, Sulewska A, Gacko M, Chyczewska E (2008). "Thiocyanate concentration in saliva of cystic fibrosis patients". Folia Histochem. Cytobiol. 46 (2): 245–6. doi:10.2478/v10042-008-0037-0. PMID 18519245.
- ↑ "Public summary of positive opinion for orphan designation of hypothiocyanite / lactoferrin for the treatment of cystic fibrosis" (PDF). Pre-authorisation Evaluation of Medicines for Human Use. European Medicines Agency. 2009-09-07. Archived from the original (PDF) on 2010-05-30. Retrieved 2010-01-23.
- ↑ "Meveol: orphan drug status granted by the FDA for the treatment of cystic fibrosis". United States Food and Drug Administration. 2009-11-05. Archived from the original on 2009-12-24. Retrieved 2010-01-23.