微睡眠
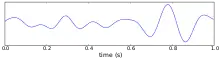
微睡眠(英語:)是指一小段维持几秒到半分钟不等的陷入睡眠或者睡意昏沉的时间,在此期间,人不对任何感官知觉有所反应而处于无意识状态。[1][2]微睡眠主要表现为在一小会儿失去意识后重新清醒,或者在清醒和昏睡的状态之间快速切换。在行为学中,微睡眠的主要表征为眼帘下垂、睑闭迟缓、缓缓点头。[2]在电生理层面,微睡眠被定义为腦電圖代表着清醒状态背景活动的8–13 Hz的α波活动为4–7 Hz的θ波活动所取代。[3]一些专家通过以上述的若干行为学指标来判断微睡眠状态,其余多以脑电图特征为鉴定依据。[4]
尽管睡眠正常的人在重复单调工作时也可能会产生微睡眠,但微睡眠往往是睡眠不足的后果。[5]微睡眠在例如开车、使用重型设备等需要高度警觉的环境下极其危险。人们经历微睡眠时往往意识不到自己的微睡眠状态,反倒以为自己一直专注工作或者只是觉得自己走了一会儿神。[6]
与神经系统关联
微睡眠时,大脑和睡意相关的区域活跃度增加,和醒意相关的区域活跃度下降。但因为存在单调的工作也可以导致微睡眠较为复杂的神经调节,且每个人的大脑结构有所差异,故客观判断与微睡眠相关的神经活动较为困难。因此建立对照用实验组并进行对照检验极其重要。
一项对正常休息过的人同时透过眼视频测试、行为反应测试、脑电图、功能性核磁共振测试的实验中[2],20名参与者需要看着操纵杆在屏幕上以上下左右四个方向移动长达50分钟,动,过半数参与者在盯着操纵杆这一持续视觉运动任务时发生了脑电图意义上的微睡眠,同时负责保持醒意的丘脑、中腦、后扣带皮层活动减弱。[2]
Chou (2011)的实验检测了五位受试者从微睡眠状态被刺激苏醒时的神经激活模式[5],发现视觉区、額葉區、边缘叶在收到直接刺激时的激活,以及前皮质、颞叶、主要運動皮質區、岛叶在醒后的激活,由此得出“思考判断能力滞后与苏醒后恢复,并有可能导致危险”的结论。
睡眠及睡意的产生由多种化学物质调节。多巴胺被认为促进了睡意,而腺苷被认为提升了醒意,共同参与微睡眠在内的睡眠调节。微睡眠状态下,腦橋─膝狀核─枕葉波) 加强,抑制了基底核的视觉处理。视觉处理通路被抑制后,负责释放多巴胺的上丘细胞并不透过基底核的相同通路去抑制,导致了微睡眠发生和神经处理能力的下降。[7]
生理学研究
微睡眠和许多疾病关联。睡眠呼吸暂停是最为流行的与微睡眠相关疾病,影响了1,000到1,500万人。[8]其他关联疾病包括發作性嗜睡病、嗜睡症、精神分裂症等造成白天过度嗜睡的疾病。微睡眠片刻往往被患者忽视,不常作为临床诊断指标,多项睡眠测试常被用来侦测微睡眠。[9]
由于反复出现的微睡眠常常会影响正常的日常生活,多数临床研究致力于利用药物手段减少微睡眠在内的日间过剩的睡意。莫达非尼在此方面几乎无副作用,故而在药物选择上十分流行;新药研发中往往会有和莫达非尼及安慰劑的效果比较。莫达非尼也有用来治疗或正被测试治疗精神分裂症、发作性昏睡、猝倒症、睡眠呼吸暂停。在莫达非尼扩大治疗对象和新药与之比较疗效的过程中,各类造成嗜睡疾病的药物干预手段的研究正在完善。
微睡眠有时是药物治疗的副作用,例如用于治疗帕金森病的多巴胺刺激药物,昏睡是普拉克索、羅匹尼羅等多巴胺抑制剂的负面作用之一。这些药物可以在50%开车中的帕金森病人中导致突然起效的睡意。[10]因此临床研究也致力于减轻这种负面作用。
多数微睡眠在临床上并不显著。感到困倦的人往往喜欢去使用一项无需处方的刺激剂,例如含咖啡中的咖啡因。高频率的低剂量咖啡因的摄入在对延长清醒情况下保持注意力确实有效,因为咖啡因是腺苷的竞争性拮抗剂,实验也从而证实腺苷在保持清醒中的作用。[11]其它刺激剂还包括阿得拉尔、苯丙胺、可卡因和烟草等。[12][13]
测试途径
侦测微睡眠的方法有很多,惟尚无对最优侦测和分类微睡眠方案的定论。简单的方式诸如心理測驗、语言测试、行为测试(如打哈欠测试和眼视频测试);复杂的也有如软件辅助的脑电图、核磁共振、眼电图、多导睡眠图。多项测试可能可以使得诊断更为准确。[2]
| 方式 | 描述 |
|---|---|
| 多項生理睡眠檢查(PSG) | 多項生理睡眠檢查,缩写为PSG,检查了睡眠期间的多项身体机能,包括了透过脑电图检测大脑活动、透过眼电图检测眼部活动以及对骨骼肌和心律的检测。 |
| 脑电图(EEG) | 脑电图,缩写EEG,透过不同置于头皮上的多电极记录了大脑在20-40分钟内的自发电活动[14]微睡眠期间,腦電圖中的α波活动为更低频率的θ波活动所取代。[15] |
| 功能性磁共振成像(fMRI) | 功能性核磁共振技术即用核磁共振技术扫描血液流动以检测大脑有哪些活跃区域、何种活动情况。[16] |
| 心理测试 | 包括心理测时法、Karolinska睡意量表[17]、维持清醒测试[18]、多重睡眠潜伏期测试等。[19] |
| 眼电图(EOG) | 眼电图测量视网膜的静息电势。[20] |
| 眼视频测试 | 透过观察眨眼等眼部活动判断微睡眠状态。[21][22] |
| 打哈欠测试 | 测量一段时间内打哈欠的次数。[23] |
| 语言测试 | 观测人说话时的表情和节律来判断睡眠状态。[17][24][25] |
尽管有人试图透过主要是脑电图或者眼动测试来进行微睡眠总分类,现阶段仍然存在不同条件下侦测到的不同种类的微睡眠。[26]Karolinska睡意量表之类的主观自述类型的心理测试尽管和脑电图被认为有正关联,但很难区别睡意的程度而存在局限性。[27]未来的研究需要更加注重小而微的客观现象,例如更短间隔内的脑电波细节等,来揭示电活动和行为活动的关系,以获得更高的侦测准确率。[28]如此,微睡眠可以自然而然地和不同的清醒状态区别出来。[29]
社会危害性


在美国,单单疲劳驾驶一项每年就造成1,550死40,000伤,使得睡眠不足成为重要的公共安全议题。[30][31]微睡眠主要表现为在一小会儿失去意识后重新清醒,或者在清醒和昏睡的状态之间快速切换。在行车途中,疲劳驾驶的司机会可能会经历无知觉的几秒钟,这便是微睡眠的具体例子。司机很难发现自己失去了的几秒钟,但微睡眠期间的驾驶却有极大造成交通事故的风险。[32]
历史上,不少交通事故在微睡眠期间发生。[33]微睡眠状态下的驾驶被指间接造成了2003年发生瀑布列车事故:火车司机心脏病发,而值班守卫却被监察者指在微睡眠状态,只是列车异常速度无法被正常响应。2009年的造成飞机坠毁大西洋的法國航空447號班機空難中,机长曾报告说:“我昨夜没睡够。只有一个小时,那不够。”遂甩手给两位副驾驶,后者未能在飞机遇到危险的时候合理处置,造成了事故。[34][35]切尔诺贝利核事故中,反应堆开始过热的主要原因就是睡意昏沉的操作人员错误地关闭了制冷系统,最终导致了一系列事故发生。[36]
因此,微睡眠常常在用来检测司机的睡意以及预防工伤和公共安全事故。相关数据如下:
- 44%深夜开车的司机会陷入危机行车安全的睡意中。[37]
- 极度劳累的工作流程会提升至多35%的事故发生率。[38]
- 长期微睡眠增加工人伤亡概率及缺勤率,降低工人生产效率。[39]
- 美国疾病控制与预防中心研究指出,来自12州的74,571的成年受访者中,仅35.3%称自己24小时能有7小时睡眠,48.0%称自己打鼾,37.9%称自己近前一月至少一次无意识陷入睡眠,4.7%称自己前一月至少一次在开车时陷入睡意。[30]
- 美国国家公路交通安全管理局估计疲劳驾驶发生于2.5%致命道路交通事故及2%的致伤事故中。[40]
- 1993年到2009年的16年间,疲劳驾驶造成的空难造成了250人死亡。[41]
例如无聊的课程等单调事务也会导致微睡眠状态的发生,这时微睡眠也叫白日类催眠状态。[42]
附录:药理文献摘选
| 文献标题 | 药物干涉方式 | 研究疾病 |
|---|---|---|
| Effects of BF2.649 in the Treatment of Excessive Daytime Sleepiness in Narcolepsy.[43] | 药物:BF2.649[註 1]、药物:莫达非尼、药物:安慰剂 | 发作性睡病 |
| Efficacy and Safety Study of BF2.649 in the Treatment of Excessive Daytime Sleepiness in Narcolepsy[44] | 药物:BF2.649、莫达非尼、安慰剂 | 发作性睡病、过度日间睡意、猝倒症等睡眠障碍 |
| Dose Range Finding Study of BF2.649 Versus Placebo to Treat Excessive Daytime Sleepiness in Parkinson's Disease Patients[45] | 药物:安慰剂、药物:BF 2.649 5 mg、药物:BF 2.649 10 mg、药物:BF 2.649 20 mg、药物:BF2.649 40 mg | 过度日间睡意、帕金森氏症 |
| A Study Of A Novel Compound For Excessive Daytime Sleepiness Associated With Narcolepsy[46] | 药物:安慰剂、药物:PF-03654746 | 过度日间睡意、发作性睡病 |
| Treatment of Refractory Excessive Daytime Sleepiness in Patients With Obstructive Sleep Apnea/Hypopnea Syndrome (OSA/HS) Using Nasal Continuous Positive Airway Pressure (nCPAP) Therapy (0249-015)[47] | 比较药剂:MK0249, 药物:比较药剂:安慰剂, 药物:比较药剂:莫达非尼 | 阻塞性睡眠呼吸暂停、浅呼吸综合症、过度日间睡意 |
| Pitolisant to Assess Weekly Frequency of Cataplexy Attacks and EDS in Narcoleptic Patients (HARMONY CTP)[48] | 药物:BF2.649, 药物:安慰剂 | 伴猝倒症及过度日间睡意的发作性睡病 |
| Comparison of Modafinil and Methylphenidate in Treatment of Excessive Daytime Sleepiness in Patients With Parkinson's Disease[49] | 药物:莫达非尼、药物:哌甲酯 | 帕金森病 |
| Modafinil Augmentation Therapy for Excessive Daytime Sleepiness and Negative Symptoms in Patients With Schizophrenia[50] | 药物:莫达非尼、药物:安慰剂 | 精神分裂症 |
| Efficacy and Safety of BF2.649 in Excessive Daytime Sleepiness (EDS) in Parkinson's Disease[51] | 药物:BF2.649 | 帕金森病 |
| Trial of Xyrem for Excessive Daytime Sleepiness and Sleep Disturbance in Parkinson's Disease (PD)[52] | 药物:Γ-羟基丁酸钠 | 帕金森病 |
参考资料
文内注记
- 也称Pitolisant。
文内脚注
- International Classification of Sleep Disorders Diagnostic and Coding Manual, (PDF). [2011-07-26]. (原始内容 (PDF)存档于2011-07-26)., page 343
- Poudel, G. R., Innes, C. R., Bones, P. J., Watts, R., & Jones, R. D. (2012). Losing the struggle to stay awake: Divergent thalamic and cortical activity during microsleeps. Human Brain Mapping: 00:000-000
- Paul, Amit; Linda Ng Boyle; Jon Tippin; Matthew Rizzo. (PDF). Proceedings of the Third International Driving Symposium on Human Factors in Driver Assessment, Training and Vehicle Design. 2005 [2008-02-10]. (原始内容 (PDF)存档于2014-10-09).
- Poudel, G.R.; Innes, C. R. H.; Bones, P.J.; Watts, R.; Jones, R. D.,. (PDF). Human Brain Mapping. [2013-03-20]. doi:10.1002/hbm.22178. (原始内容 (PDF)存档于2014-03-31).
- Chou, Y. H., Chuang, C. C., Zao, J. K., Ko, L. W., & Lin, C. T. (2011, August). An fMRI study of abrupt-awake episodes during behavioral microsleeps. In Engineering in Medicine and Biology Society, EMBC, 2011 Annual International Conference of the IEEE (pp. 5060-5063). IEEE.
- Higgins, Laura; Fette Bernie. (PDF). [2013-06-12]. (原始内容 (PDF)存档于2011-08-20).
- Silkis, I. G. (2010). Analysis of the effects of neuromodulators on the generation of spontaneous pontine-geniculate-occipital (PGO) waves. Neurochemical Journal, 4(3), 170-177.
- Kanagala, R., Murali, N. S., Friedman, P. A., Ammash, N. M., Gersh, B. J., Ballman, K. V., ... & Somers, V. K. (2003). Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation, 107(20), 2589-2594.
- Tufik, S., Santos-Silva, R., Taddei, J. A., & Bittencourt, L. R. A. (2010). Obstructive sleep apnea syndrome in the Sao Paulo epidemiologic sleep study. Sleep Medicine Reviews, 11(5), 441-446.
- Hobson, D. E., Lang, A. E., Martin, W. W., Razmy, A., Rivest, J., & Fleming, J. (2002). "Excessive daytime sleepiness and sudden-onset sleep in Parkinson disease. "JAMA: The Journal of the American Medical Association, 287(4), 455–463. Chicago
- Wyatt, J. K., Cajochen, C., Cecco, A. R. D., Czeisler, C. A., & Dijk, D. J. (2004). "Low-dose repeated caffeine administration for circadian-phase-dependent performance degradation during extended wakefulness." SLEEP-NEW YORK THEN WESTCHESTER-, 27(3), 374–382.
- Jacobs, A. (2005). "The Adderall advantage." New York Times, 31.
- Gawin, F. H., & Ellinwood, E. H. (1988). "Cocaine and other stimulants: actions, abuse, and treatment." The New England Journal of Medicine.
- Davidson, P. R., Jones, R. D., & Peiris, M. T. R. (2006, January). Detecting Behavioral Microsleeps using EEG and LSTM Recurrent Neural Networks. InEngineering in Medicine and Biology Society, 2005. IEEE-EMBS 2005. 27th Annual International Conference of the (pp. 5754-5757). IEEE.
- Boyle, L. N., Tippin, J., Paul, A., & Rizzo, M. (2008). Driver performance in the moments surrounding a microsleep. Transportation research part F: traffic psychology and behaviour, 11(2), 126-136.
- Chou, Y. H., Chuang, C. C., Zao, J. K., Ko, L. W., & Lin, C. T. (2011, August). An fMRI study of abrupt-awake episodes during behavioral microsleeps. InEngineering in Medicine and Biology Society, EMBC, 2011 Annual International Conference of the IEEE (pp. 5060-5063). IEEE.
- Krajewski, J., Wieland, R., & Batliner, A. (2008). An acoustic framework for detecting fatigue in speech based Human-Computer-Interaction. In Computers Helping People with Special Needs (pp. 54-61). Springer Berlin Heidelberg.
- Gast, H., Schindler, K., Rummel, C., Herrmann, U. S., Roth, C., Hess, C. W., & Mathis, J. (2011). EEG correlation and power during maintenance of wakefulness test after sleep-deprivation. Clinical Neurophysiology, 122(10), 2025-2031.
- Blaivas, A. J., Patel, R., Hom, D., Antigua, K., & Ashtyani, H. (2007). Quantifying microsleep to help assess subjective sleepiness. Sleep Medicine Reviews,8(2), 156-159.
- Sommer, D., Chen, M., Golz, M., Trutschel, U., & Mandic, D. (2005). Fusion of state space and frequency-domain features for improved microsleep detection. In Artificial Neural Networks: Formal Models and Their Applications–ICANN 2005 (pp. 753-759). Springer Berlin Heidelberg.
- Poudel, G. R., Innes, C. R., Bones, P. J., & Jones, R. D. (2010, August). The relationship between behavioural microsleeps, visuomotor performance and EEG theta. In Engineering in Medicine and Biology Society (EMBC), 2010 Annual International Conference of the IEEE (pp. 4452-4455). IEEE.
- Malla, A. M., Davidson, P. R., Bones, P. J., Green, R., & Jones, R. D. (2010, August). Automated video-based measurement of eye closure for detecting behavioral microsleep. In Engineering in Medicine and Biology Society (EMBC), 2010 Annual International Conference of the IEEE (pp. 6741-6744). IEEE.
- Noor, H. A. M., & Ibrahim, R. (2010). Fatigue detector using eyelid blinking and mouth yawning. In Computer Vision and Graphics (pp. 134-141). Springer Berlin Heidelberg.
- Krajewski, J., Batliner, A., & Wieland, R. (2008, December). Multiple classifier applied on predicting microsleep from speech. In Pattern Recognition, 2008. ICPR 2008. 19th International Conference on (pp. 1-4). IEEE.
- Krajewski, J., Golz, M., Sommer, D., & Wieland, R. (2009, January). Genetic algorithm based feature selection applied on predicting microsleep from speech. In 4th European Conference of the International Federation for Medical and Biological Engineering (pp. 184-187). Springer Berlin Heidelberg.
- Galley, N., Schleicher, R., & Galley, L. (2003). Oculomotor Indicators of Driver Fatigue. Driver Behaviour and Training: v. III, 1, 97.
- Shahid, A., Wilkinson, K., & Marcu, S. (2012). Karolinska Sleepiness Scale (KSS). In STOP, THAT and One Hundred Other Sleep Scales (pp. 209-210). Springer New York.
- Cvetkovic, D., & Cosic, I. (2011). Sleep Onset Process as an Altered State of Consciousness. In States of Consciousness (pp. 157-185). Springer Berlin Heidelberg.
- Baars, B. J. (2013). A scientific approach to silent consciousness. Frontiers in Psychology, 4.
- Insufficient Sleep Is a Public Health Epidemic. https://www.cdc.gov/features/dssleep/ (页面存档备份,存于)
- US Department of Transportation, National Highway Traffic Safety Administration, National Center on Sleep Disorders Research, National Heart Lung and Blood Institute. Drowsy driving and automobile crashes [National Highway Traffic Safety Administration Web Site]. Available at http://www.nhtsa.gov/people/injury/drowsy_driving1/Drowsy.html#NCSDR/NHTSAExternal (页面存档备份,存于) Web Site Icon Accessed February 10, 2011.
- . sleepdex.org. [15 May 2015]. (原始内容存档于2016-11-25).
- Blaivas AJ, Patel R, Hom D, Antigua K, Ashtyani H. . Sleep Medicine Reviews. 2007, 8 (2): 156–9 [2019-01-13]. PMID 17239659. doi:10.1016/j.sleep.2006.06.011. (原始内容存档于2019-05-22).
- BEA final report, section 1.5, page 24 (PDF page 26 of 224): "The crew had left Paris on Thursday 28 May 2009 in the morning and arrived in Rio de Janeiro in the evening of the same day"
- "Revealed: Pilot of Air France jet that crashed in Atlantic Ocean killing 228 people had just ONE HOUR sleep before flight", The Daily Mail (UK), 2013-03-15.
- Coren, Stanley. Sleep Thieves: An Eye-Opening Exploration into the Science & Mysteries of Sleep. New York: The Free Press, 1996. p. x, 241–44
- Åkerstedt, T., Hallvig, D., Anund, A., Fors, C., Schwarz, J., & Kecklund, G. (2013). "Having to stop driving at night because of dangerous sleepiness–awareness, physiology and behaviour." Journal of Sleep Research.
- Sirois, B., Trutschel, U., Edwards, D., Sommer, D., & Golz, M. (2010, January). "Predicting Accident Probability from Frequency of Microsleep Events." In World Congress on Medical Physics and Biomedical Engineering, September 7–12, 2009, Munich, Germany (pp. 2284–2286). Springer Berlin Heidelberg.
- Swanson, L. M., ARNEDT, J., Rosekind, M. R., Belenky, G., Balkin, T. J., & Drake, C. (2011). "Sleep disorders and work performance: findings from the 2008 National Sleep Foundation Sleep in America poll." Journal of Sleep Research, 20(3), 487-494.
- National Highway Traffic Safety Administration. Traffic Safety Facts Crash Stats: Drowsy Driving. Washington, DC: DOT; 2011. DOT HS 811 4492011.
- "Pilot fatigue is like 'having too much to drink'." CNN, May 15, 2009. http://www.cnn.com/2009/TRAVEL/05/15/pilot.fatigue.buffalo.crash/ (页面存档备份,存于)
- Gurstelle, E. B., & De Oliveira, J. L. (2004). "Daytime parahypnagogia: a state of consciousness that occurs when we almost fall asleep." Medical Hypotheses, 62(2), 166–168.
- Effects of BF2.649 in the Treatment of Excessive Daytime Sleepiness in Narcolepsy. http://clinicaltrials.gov/ct2/show/record/NCT01638403 (页面存档备份,存于)
- Efficacy and Safety Study of BF2.649 in the Treatment of Excessive Daytime Sleepiness in Narcolepsy. http://ClinicalTrials.gov/show/NCT01067222 (页面存档备份,存于)
- Dose Range Finding Study of BF2.649 Versus Placebo to Treat Excessive Daytime Sleepiness in Parkinson's Disease Patients . http://ClinicalTrials.gov/show/NCT00642928 (页面存档备份,存于)
- A Study Of A Novel Compound For Excessive Daytime Sleepiness Associated With Narcolepsy. http://ClinicalTrials.gov/show/NCT01006122 (页面存档备份,存于)
- Treatment of Refractory Excessive Daytime Sleepiness in Patients With Obstructive Sleep Apnea/Hypopnea Syndrome (OSA/HS) Using Nasal Continuous Positive Airway Pressure (nCPAP) Therapy (0249-015). http://ClinicalTrials.gov/show/NCT00620659 (页面存档备份,存于)
- Pitolisant to Assess Weekly Frequency of Cataplexy Attacks and EDS in Narcoleptic Patients (HARMONY CTP). http://ClinicalTrials.gov/show/NCT01800045 (页面存档备份,存于)
- Comparison of Modafinil and Methylphenidate in Treatment of Excessive Daytime Sleepiness in Patients With Parkinson's Disease. http://ClinicalTrials.gov/show/NCT00393562 (页面存档备份,存于)
- Modafinil Augmentation Therapy for Excessive Daytime Sleepiness and Negative Symptoms in Patients With Schizophrenia . http://ClinicalTrials.gov/show/NCT00546403 (页面存档备份,存于)
- Efficacy and Safety of BF2.649 in Excessive Daytime Sleepiness (EDS) in Parkinson's Disease. http://ClinicalTrials.gov/show/NCT01066442 (页面存档备份,存于)
- Trial of Xyrem for Excessive Daytime Sleepiness and Sleep Disturbance in Parkinson's Disease (PD). http://ClinicalTrials.gov/show/NCT00641186 (页面存档备份,存于)
参阅作品
- Ogilvie RD. . Sleep Med Rev. June 2001, 5 (3): 247–270 [2019-01-13]. PMID 12530990. doi:10.1053/smrv.2001.0145. (原始内容存档于2019-05-23).
- Tirunahari VL, Zaidi SA, Sharma R, Skurnick J, Ashtyani H. . Sleep Med. Rev. January 2003, 4 (1): 63–7 [2019-01-13]. PMID 14592362. doi:10.1016/s1389-9457(02)00250-2. (原始内容存档于2019-05-22).
- Faber J, Novák M, Svoboda P, Tatarinov V, Tichý T. . Sb Lek. 2003, 104 (4): 375–85. PMID 15320529 (捷克语).