.jpg.webp)
Chronic fatigue syndrome (CFS) is an illness with a long history of controversy. Some professionals within the medical community do not recognize CFS as a genuine condition, nor is there agreement on its prevalence.[1][2][3] There has been much disagreement over the pathophysiology of chronic fatigue syndrome, how it should be diagnosed, and how to treat it.[4]
The diagnosis is controversial, and its etiology is still not fully understood. Alternative names to describe the condition(s) have been used over time throughout the world. Patient groups have criticized the name "chronic fatigue syndrome", saying that it trivializes the illness.
Naming
A 2007 article in The New York Times reported that patients prefer the terms myalgic encephalomyelitis or myalgic encephalopathy to "chronic fatigue syndrome". They believe the term fatigue trivializes the illness and discourages research into potential treatments.[5]
According to a survey of medical trainees at a school in the United States, a condition described as "chronic fatigue syndrome" is considered less serious than a condition described as "myalgic encephalopathy".[6] In 2004, a paper reported that the overwhelming majority of the CFS patients questioned in surveys wanted the name changed from chronic fatigue syndrome.[7]
In 2015 the National Academy of Medicine recommended changing the name to Systemic Exertion Intolerance Disease (SEID) in their report "Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness"'.
Cause, diagnosis and treatment
Recognition
Historically, many professionals within the medical community were unfamiliar with CFS, or they did not recognize it as a real condition, and disagreed on its prevalence or seriousness.[1][2][8] A 2005 study in the UK surveyed 811 general practitioners' attitudes and knowledge of CFS. 72% accepted CFS as a recognizable clinical entity, but 48% did not feel confident diagnosing it, and 41% did not feel confident in treatment.[9] The CFS Advisory Committee (Part of the US Department of Health) in 2007 found that a survey of 1,500 US primary care providers showed that 90% believed CFS can impair quality of life, 20% strongly or somewhat agreed that CFS is only in the patient's head, and 70% said not enough information is available to diagnose CFS.[10] A 2008 Norwegian study that explored barriers to quality care faced by patients with chronic fatigue syndrome concluded, "Current medical scepticism and ignorance regarding CFS shapes the context of medical care and the illness experiences of CFS patients, who may feel they neither get a proper assessment nor management."[11]
Training may influence attitudes to CFS. One study conducted a relatively brief seminar presenting factual information on CFS to a cohort of fourth year medical students. The authors concluded the information provided was associated with a more favorable attitude toward CFS.[12] In the UK, the 2002 Chief Medical Officer's report stated that all doctors should consider CFS as a serious chronic illness and treat patients accordingly.[13] In 2006, the US Centers for Disease Control and Prevention (CDC) launched a national program to educate the American public and health care professionals about CFS.[14]
Contrasting viewpoints
There has been much disagreement over proposed cause(s), diagnosis, and treatment of the illness.[15][16][4] Contrasting viewpoints have been expressed by different CFS researchers. One influential 1993 Lancet paper argued that CFS was a form of neurasthenia to be classified as a psychiatric condition, and a subsequent 1998 paper concluded that behavioral, cognitive, and affective factors all played a role in perpetuating fatigue.[17][18] More recently, a 2005 population-based study, which used a similar methodology to the earlier 1998 study, found important differences between CFS and psychiatrically explained chronic fatigue which could affect the development of therapy and explanatory models. They concluded that the 1998 model adequately represented chronic fatigue secondary to psychiatric conditions, but not CFS.[19]
Contested causation may have serious negative effects on healthcare for individuals, as it may erode patient-provider trust, test the provider's self-assurance and capacity to share power with the patient, and raise problematic issues of reparation, compensation and blame.[20]
In 2011, a major divide still existed as to whether funding should be directed towards biomedical or psychological research.[21]
XMRV retrovirus

In 2009, the journal Science[22] published a study that identified the XMRV retrovirus in blood samples of a population of people with CFS. After the Science publication, media attention generated interest in the XMRV virus worldwide. Doubts over the legitimacy of CFS had long caused patient frustration about the marginalization of the debilitating illness, and persons with CFS and their support organizations were optimistic the cause of their symptoms had been found.[23]
Many countries reacted quickly to protect the blood supply from the XMRV retrovirus by banning persons with CFS from donating blood. The United States funded a 1.3 million dollar study to try to validate the findings, and some people with the illness started taking antiviral drugs in hopes of symptomatic improvement.[23]
Many studies failed to reproduce this finding,[24][25][26] and recriminations of misconduct from the various stakeholders grew angry and bitter.[23]
In 2011, the editor of Science formally retracted its XMRV paper[27] while the Proceedings of the National Academy of Sciences similarly retracted a 2010 paper which had appeared to support the finding of a connection between XMRV and CFS.[28] Studies eventually concluded that neither people nor the blood supply had been infected with the XMRV virus, and the origin of the virus was likely a lab contaminant in the supplies used by the polymerase chain reaction (PCR) process of the studies that found virus in blood.[29]
PACE trial
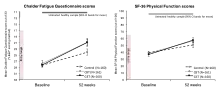
PACE was a large trial investigating the efficacy and safety of three treatments adjunctive to specialist medical care (SMC): cognitive behavioural therapy (CBT), graded exercise therapy (GET), and adaptive pacing therapy (APT). The results were published in February 2011 and concluded that CBT and GET were each "moderately" effective compared to SMC alone, while APT was not found to be effective when added to SMC.[30]
.jpg.webp)
The trial generated considerable adverse criticism. Letters to the editor critiqued the definitions of secondary outcomes, questioned post-hoc protocol changes, and expressed concern over generalisability of the results. Patient groups and the IACFS/ME (an organization of researchers and health care professionals interested in CFS)[31] criticized the trial for over-simplified and exaggerated conclusions, for using a flawed psychosocial illness model that ignores biological evidence, for testing a non-representative version of pacing, and because the results seriously conflict with their member surveys which show that pacing is effective and CBT or GET can cause deterioration in many patients who use the treatments.[32][33][34] One notable researcher submitted a 442-page letter to the Medical Research Council outlining his criticisms of the trial, and a shorter 43-page complaint to the Lancet. The MRC and the Lancet rejected the submissions. A Lancet editorial responded to the adverse criticism by suggesting that some critics could be part of "an active campaign to discredit the research."[35][21] In 2011, Lancet Editor Richard Horton defended the trial, calling the critics "a fairly small, but highly organized, very vocal and very damaging group of individuals who have, I would say, actually hijacked this agenda and distorted the debate so that it actually harms the overwhelming majority of patients."[36][37]
More recent criticisms of the trial have come from the scientific community. For example, biostatistician Bruce Levin of Columbia University described the study as "the height of clinical trial amateurism", and Ronald Davis of Stanford University wrote, "I'm shocked that the Lancet published it... The PACE study has so many flaws and there are so many questions you'd want to ask about it that I don't understand how it got through any kind of peer review".[38] In an analysis of the study's design, the mathematician Professor Rebecca Goldin wrote that "There were problems with the study on almost all levels... the flaws in this design were enough to doom its results from the start."[39] Professor Jonathan Edwards of University College London (UCL) has written that the PACE trial "is an unblinded trial with subjective outcome measures. That makes it a non-starter in the eyes of any physician or clinical pharmacologist familiar with problems of systematic bias in trial execution."[40]
The full research data for the PACE trial was requested by both patients acting as citizen scientists, and by other researchers but was initially denied until a 2016 tribunal ordered the data be released.[41] Several researchers published a re-analysis of the PACE trial data, but drawing the conclusion that the CBT and GET treatments were not effective and possibly not safe.[42][43][44][45] The full PACE trial outcome data showed that the treatments did not result in patients being able to return to work or study,[46] and that they were not able to walk significantly further after treatment.[45] This new information was one of several factors that lead to the UK deciding to complete a full review and update to its diagnostic and treatment guidelines for CFS/ME.[41]
Support for patients in the UK and US

A 2006 investigation by a group from the Parliament of the United Kingdom found there was not enough support in the UK for CFS patients in terms of access to government benefits and health care.[47] Individuals with the condition describe the struggle for healthcare and legitimacy due to what they consider to be bureaucratic denial of the condition because of its lack of a known etiology. Institutions maintain the exclusion of patient support by rhetorical arguments of the open-endedness of science to delay new findings of fact. This has resulted in an expensive and prolonged conflict for all involved.[2][48]
Research funding diversion at the CDC
In 1998, William Reaves, a director at the Centers for Disease Control (CDC), alleged deceptive Congressional testimony was given by officials at the agency concerning CFS research activities conducted by the organization; specifically, funds for programs intended for CFS research were diverted to other projects and not reported. He also stated he was retaliated against by his superior, Brian Mahy, after he reported the irregularities.[49][50]
A Government Accounting Office (GAO) investigation disclosed almost 13 million dollars for CFS research had been redirected or improperly accounted for by the CDC. The agency stated the funds were redistributed in order to respond to other public health emergencies. The director of a U.S. national patient advocacy group charged the CDC had a bias against studying the disease.[49]
In response, the CDC pledged reforms to accounting practices to reduce misuse of funds earmarked for specific diseases. Additionally, the money diverted from CFS research was to be restored over a period of three years.[49]
Potential harms to patients
A review in 2019 identified seven possible types of medical harm that patients with CFS may face, and concluded that biopsychosocial model had a focus that was "too narrow" and did not fit the "patient narrative".[51][44] A UK treatment programme of psycho-behavioral interventions was found to fail to meet the needs of patients with chronic fatigue syndrome, and to lack oversight.[52] A number of different authors have raised concerns about medical harm to patients, particularly resulting from the use of cognitive behavioral therapy (CBT) as a primary treatment, the use of graded exercise therapy (GET), and delays in diagnosis.[53][43][54]
Concerns have also been raised about a clinical trial of the Lightning Process in children,[55] a treatment not approved for use in adults,[56][57] and a series of publications have been corrected due to inaccurate ethics statements.[57]
Historical perceptions

Epidemic cases of myalgic encephalomyelitis were called mass hysteria by psychiatrists McEvedy and Beard in 1970,[58] provoking criticism in letters to the editor of the British Medical Journal by attending physicians, researchers, and nurses who fell ill.[59][60][61][62][63][64][65][66][67] The psychiatrists were criticized for not investigating the patients they described,[68] and their conclusions have been refuted.[69][70][71] In 1978 a symposium held at the Royal Society of Medicine (RSM) concluded that epidemic myalgic encephalomyelitis was a distinct disease entity.[72]
However, the idea that CFS may be culturally mediated persisted in some quarters. In her 1997 book Hystories: Hysterical Epidemics and Modern Culture, literary critic and feminist Elaine Showalter argues that chronic fatigue syndrome is a "hysterical narrative", a modern manifestation of hysteria, a self-perpetuating "cultural symptom of anxiety and stress" historically assigned to women.[73]
Political
A 2006 report by the UK Parliamentary Group on Scientific Research into Myalgic Encephalomyelitis stated that: "CFS/ME is defined as a psychosocial illness by the Department for Work and Pensions (DWP) and medical insurance companies. Therefore, claimants are not entitled to the higher level of benefit payments. We recognise that if CFS/ME remains as one illness and/or both remain defined as psychosocial then it would be in the financial interest of both the DWP and the medical insurance companies." The Group called for investigation of what they called, "numerous cases where advisors to the DWP have also had consultancy roles in medical insurance companies. Particularly the Company UNUMProvident. Given the vested interest private medical insurance companies have in ensuring CFS/ME remain classified as a psychosocial illness there is blatant conflict of interest here." The Secretary of State for Work and Pensions responded that "Entitlement to Disability Living Allowance depends on the effects that severe physical or mental disability has on a person's need for personal care and/or their ability to walk, and not on particular disabilities or diagnoses. The benefit is available to people with myalgic encephalomyelitis (which can have a physical basis or a psychological basis, or can be due to a combination of factors) on exactly the same terms as other severely disabled people, and they can qualify for it provided that they meet the usual entitlement conditions."[74]
Reports of researcher harassment in the UK

Researchers who advocate classifying CFS as a psychosocial illness have been criticized by those who believe that their work draws attention and funding away from research into biomedical treatments. In 2012, several prominent UK researchers adopting the psychosocial perspective reported to the press that they had been verbally abused by patients, and one reported receiving death threats.[21] In 2019, PACE trial author Prof. Michael Sharpe said that he was subject to near daily intimidation and abuse from people upset with his work, because they believe it means the illness is psychological. He said that he believes that CFS is a "biological condition that can be perpetuated by social and psychological factors".[75] Blease and Geragty (2018) investigated the assertions, and submitted that the claims of researcher harassment were used to argue against releasing the full anonymised data from the PACE trial at the 2016 Freedom of Information tribunal. The tribunal judge stated the claims of harassment had been "wildly exaggerated by the trial authors and their expert witnesses", and ordered the release of the data.[41]
Blease and Geragty found "no compelling evidence" the vast majority of ME/CFS patients or their advocacy organizations had adopted "militant political policies or behaviours", and reported ME/CFS activists used public discourse and scientific publications analogous to 1980s "AIDS" activists. They concluded the medical establishment's negative perceptions of persons with ME/CFS, and indifference to patient's opinions conceptualized the ME/CFS community's discontent.[41]
References
- 1 2 Wallace PG (October 1991). "Post-viral fatigue syndrome. Epidemiology: a critical review". British Medical Bulletin. 47 (4): 942–51. doi:10.1093/oxfordjournals.bmb.a072522. PMID 1794092.
- 1 2 3 Mounstephen A, Sharpe M (May 1997). "Chronic fatigue syndrome and occupational health". Occupational Medicine. 47 (4): 217–27. doi:10.1093/occmed/47.4.217. PMID 9231495.
- ↑ Solomon L, Reeves WC (November 2004). "Factors influencing the diagnosis of chronic fatigue syndrome". Archives of Internal Medicine. 164 (20): 2241–5. doi:10.1001/archinte.164.20.2241. PMID 15534161.
- 1 2 Hooge J (1992). "Chronic fatigue syndrome: cause, controversy and care". British Journal of Nursing. 1 (9): 440–1, 443, 445–6. doi:10.12968/bjon.1992.1.9.440. PMID 1446147.
- ↑ Tuller D (17 July 2007). "Chronic Fatigue Syndrome No Longer Seen as 'Yuppie Flu'". The New York Times. Retrieved 15 June 2009.
- ↑ Jason LA, Taylor RR, Plioplys S, Stepanek Z, Shlaes J (2002). "Evaluating attributions for an illness based upon the name: chronic fatigue syndrome, myalgic encephalopathy and Florence Nightingale disease". Am J Community Psychol. 30 (1): 133–48. doi:10.1023/A:1014328319297. PMID 11928774. S2CID 27350772.
- ↑ Jason LA, Holbert C, Torres-Harding S, Taylor RR (2004). "Stigma and the Term Chronic Fatigue Syndrome". Journal of Disability Policy Studies. 14 (4): 222–228. CiteSeerX 10.1.1.486.4577. doi:10.1177/10442073040140040401. S2CID 72397898.
- ↑ Jason LA, Richman JA, Friedberg F, Wagner L, Taylor R, Jordan KM (1997). "Politics, science, and the emergence of a new disease. The case of chronic fatigue syndrome". Am Psychol. 52 (9): 973–83. doi:10.1037/0003-066X.52.9.973. PMID 9301342.
- ↑ Bowen J, Pheby D, Charlett A, McNulty C (2005). "Chronic Fatigue Syndrome: a survey of GPs' attitudes and knowledge". Fam Pract. 22 (4): 389–93. doi:10.1093/fampra/cmi019. PMID 15805128.
- ↑ Oleske JM (28–29 November 2007). Chronic Fatigue Syndrome Advisory Committee (CFSAC) meeting. Hubert H. Humphrey Building, Washington, D.C.: U.S. Department of Health & Human Services. Retrieved 18 April 2008.
- ↑ Gilje AM, Söderlund A, Malterud K (May 2008). "Obstructions for quality care experienced by patients with chronic fatigue syndrome (CFS)-A case study". Patient Educ Couns. 73 (1): 36–41. doi:10.1016/j.pec.2008.04.001. PMID 18486415.
- ↑ Friedberg F, Sohl SJ, Halperin PJ (May 2008). "Teaching medical students about medically unexplained illnesses: A preliminary study". Med Teach. 30 (6): 618–21. doi:10.1080/01421590801946970. PMID 18608944. S2CID 23465440.
- ↑ CFS/ME Working Group (11 January 2002). "A report of the CFS/ME working group: report to the chief medical officer of an independent working group". London: Department of Health. Retrieved 26 May 2009.
- ↑ "Chronic Fatigue Syndrome Mission / Goals". Centers for Disease Control and Prevention. 11 May 2006. Retrieved 18 August 2009.
- ↑ Sharpe M (September 1996). "Chronic fatigue syndrome". The Psychiatric Clinics of North America. 19 (3): 549–73. doi:10.1016/S0193-953X(05)70305-1. PMID 8856816.
- ↑ Horton-Salway M (December 2007). "The ME Bandwagon and other labels: constructing the genuine case in talk about a controversial illness" (PDF). The British Journal of Social Psychology. 46 (Pt 4): 895–914. doi:10.1348/014466607X173456. PMID 17535450.
- ↑ David A, Wessely S (November 1993). "Chronic fatigue, ME, and ICD-10". Lancet. 342 (8881): 1247–8. doi:10.1016/0140-6736(93)92234-K. PMID 7901572. S2CID 19204618.
- ↑ Vercoulen JH, Swanink CM, Galama JM, Fennis JF, Jongen PJ, Hommes OR, et al. (December 1998). "The persistence of fatigue in chronic fatigue syndrome and multiple sclerosis: development of a model". Journal of Psychosomatic Research. 45 (6): 507–17. doi:10.1016/S0022-3999(98)00023-3. PMID 9859853.
- ↑ Song S, Jason LA (2005). "A population based study of CFS experienced in differing patient groups. An effort to replicate Vercoulen et al.'s model of CFS" (PDF). Journal of Mental Health. 14 (3): 277–289. doi:10.1080/09638230500076165. S2CID 72869012.
- ↑ Engel CC, Adkins JA, Cowan DN (2002). "Caring for medically unexplained physical symptoms after toxic environmental exposures: effects of contested causation". Environ. Health Perspect. 110 (Suppl 4): 641–7. doi:10.1289/ehp.02110s4641. PMC 1241219. PMID 12194900.
- 1 2 3 Hawkes N (June 2011). "Dangers of research into chronic fatigue syndrome". BMJ. 342: d3780. doi:10.1136/bmj.d3780. PMID 21697226. S2CID 27301336.
- ↑ Lombardi VC, Ruscetti FW, Das Gupta J, Pfost MA, Hagen KS, Peterson DL, Ruscetti SK, Bagni RK, Petrow-Sadowski C, Gold B, Dean M, Silverman RH, Mikovits JA (October 2009). "Detection of an infectious retrovirus, XMRV, in blood cells of patients with chronic fatigue syndrome". Science. 326 (5952): 585–9. Bibcode:2009Sci...326..585L. doi:10.1126/science.1179052. PMC 3073172. PMID 19815723. (Retracted, see doi:10.1126/science.334.6063.1636-a)
- 1 2 3 Callaway E (March 2011). "Virology: Fighting for a cause". Nature. 471 (7338): 282–5. Bibcode:2011Natur.471..282C. doi:10.1038/471282a. PMID 21412308. S2CID 1416235.
- ↑ Erlwein O, Kaye S, McClure MO, Weber J, Wills G, Collier D, Wessely S, Cleare A (January 2010). Nixon DF (ed.). "Failure to detect the novel retrovirus XMRV in chronic fatigue syndrome". PLOS ONE. 5 (1): e8519. Bibcode:2010PLoSO...5.8519E. doi:10.1371/journal.pone.0008519. PMC 2795199. PMID 20066031.
- ↑ Groom HC, Boucherit VC, Makinson K, Randal E, Baptista S, Hagan S, Gow JW, Mattes FM, Breuer J, Kerr JR, Stoye JP, Bishop KN (February 2010). "Absence of xenotropic murine leukaemia virus-related virus in UK patients with chronic fatigue syndrome". Retrovirology. 7 (1): 10. doi:10.1186/1742-4690-7-10. PMC 2839973. PMID 20156349.
- ↑ van Kuppeveld FJ, de Jong AS, Lanke KH, Verhaegh GW, Melchers WJ, Swanink CM, Bleijenberg G, Netea MG, Galama JM, van der Meer JW (February 2010). "Prevalence of xenotropic murine leukaemia virus-related virus in patients with chronic fatigue syndrome in the Netherlands: retrospective analysis of samples from an established cohort". BMJ. 340: c1018. doi:10.1136/bmj.c1018. PMC 2829122. PMID 20185493.
- ↑ Alberts B (December 2011). "Retraction". Science. 334 (6063): 1636. Bibcode:2011Sci...334.1636A. doi:10.1126/science.334.6063.1636-a. PMID 22194552.
- ↑ Lo SC, Pripuzova N, Li B, Komaroff AL, Hung GC, Wang R, Alter HJ (January 2012). "Retraction for Lo et al., Detection of MLV-related virus gene sequences in blood of patients with chronic fatigue syndrome and healthy blood donors". Proceedings of the National Academy of Sciences of the United States of America. 109 (1): 346. Bibcode:2012PNAS..109..346.. doi:10.1073/pnas.1119641109. PMC 3252929. PMID 22203980.
- ↑ Johnson AD, Cohn CS (October 2016). "Xenotropic Murine Leukemia Virus-Related Virus (XMRV) and the Safety of the Blood Supply". Clinical Microbiology Reviews. 29 (4): 749–57. doi:10.1128/CMR.00086-15. PMC 5010753. PMID 27358491.
- ↑ White PD, Goldsmith KA, Johnson AL, Potts L, Walwyn R, DeCesare JC, et al. (March 2011). "Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial". Lancet. 377 (9768): 823–36. doi:10.1016/S0140-6736(11)60096-2. PMC 3065633. PMID 21334061.
- ↑ "IACFS/ME Statement on the PACE Trial: The Issue of Illness 'Reversal'". The International Association for Chronic Fatigue Syndrome/ME (IACFS/ME). 24 February 2011. Archived from the original on 18 July 2011. Retrieved 3 August 2011.
- ↑ "PACE: 'surprising and disappointing'". Action for ME. 18 February 2011.
- ↑ Britton T (18 February 2011). "ME Association press statement about the results of the PACE study". ME Association.
- ↑ McCleary K. "Falling off the PACE" (PDF). The CAA (CFIDS) Association of America. Archived from the original (PDF) on 25 June 2011. Retrieved 26 July 2011.
- ↑ [No authors listed] (Editorial) (May 2011). "Patients' power and PACE". Lancet. 377 (9780): 1808. doi:10.1016/S0140-6736(11)60696-X. PMID 21592553. S2CID 32809857.
- ↑ "Comparison of treatments for chronic fatigue syndrome - the PACE trial". ABC Radio National. 15 April 2011. Retrieved 24 May 2020.
- ↑ Rehmeyer J (13 November 2015). "The Debate Over Chronic Fatigue Syndrome Is Suddenly Shifting". Slate Magazine.
- ↑ "An open letter to Dr. Richard Horton and The Lancet". www.virology.ws. Retrieved 2 May 2016.
- ↑ Goldin R (21 March 2016). "PACE: The research that sparked a patient rebellion and challenged medicine". Sense About Statistics. Archived from the original on 21 December 2016.
- ↑ Edwards J (August 2017). "PACE team response shows a disregard for the principles of science". Journal of Health Psychology. 22 (9): 1155–1158. doi:10.1177/1359105317700886. PMID 28805520.
- 1 2 3 4 Blease C, Geraghty KJ (September 2018). "Are ME/CFS Patient Organizations "Militant"? : Patient Protest in a Medical Controversy". Journal of Bioethical Inquiry. 15 (3): 393–401. doi:10.1007/s11673-018-9866-5. PMID 29971693. S2CID 49677273.
- ↑ Vink M (August 2017). "PACE trial authors continue to ignore their own null effect". Journal of Health Psychology. 22 (9): 1134–1140. doi:10.1177/1359105317703785. PMID 28805519. S2CID 206713549.
- 1 2 Vink M, Vink-Niese A (8 October 2018). "Graded exercise therapy for myalgic encephalomyelitis/chronic fatigue syndrome is not effective and unsafe. Re-analysis of a Cochrane review". Health Psychology Open. 5 (2): 2055102918805187. doi:10.1177/2055102918805187. PMC 6176540. PMID 30305916.
- 1 2 Twisk FN, Maes M (2009). "A review on cognitive behavorial therapy (CBT) and graded exercise therapy (GET) in myalgic encephalomyelitis (ME) / chronic fatigue syndrome (CFS): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many patients with ME/CFS". Neuro Endocrinology Letters. 30 (3): 284–99. PMID 19855350.
- 1 2 Wilshire CE, Kindlon T, Courtney R, Matthees A, Tuller D, Geraghty K, Levin B (March 2018). "Rethinking the treatment of chronic fatigue syndrome-a reanalysis and evaluation of findings from a recent major trial of graded exercise and CBT". BMC Psychology. 6 (1): 6. doi:10.1186/s40359-018-0218-3. PMC 5863477. PMID 29562932.
- ↑ Vink M, Vink-Niese F (September 2019). "Work Rehabilitation and Medical Retirement for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. A Review and Appraisal of Diagnostic Strategies". Diagnostics. 9 (4): 124. doi:10.3390/diagnostics9040124. PMC 6963831. PMID 31547009.
- ↑ Gibson I (February 2007). "A new look at chronic fatigue syndrome/myalgic encephalomyelitis". Journal of Clinical Pathology. 60 (2): 120–1. doi:10.1136/jcp.2006.042432. PMC 1860614. PMID 16935965.
- ↑ Dumit J (February 2006). "Illnesses you have to fight to get: facts as forces in uncertain, emergent illnesses". Social Science & Medicine. 62 (3): 577–90. doi:10.1016/j.socscimed.2005.06.018. PMID 16085344.
- 1 2 3 Dove A (August 2000). "GAO reports on CFS funding controversy". Nature Medicine. 6 (8): 846. doi:10.1038/78579. PMID 10932206. S2CID 1431198.
- ↑ Mays P (6 July 1999). "CDC Diverts Chronic Fatigue Funds". AP NEWS. Retrieved 25 June 2020.
- ↑ Geraghty KJ, Blease C (December 2019). "Myalgic encephalomyelitis/chronic fatigue syndrome and the biopsychosocial model: a review of patient harm and distress in the medical encounter". Disability and Rehabilitation. 41 (25): 3092–3102. doi:10.1080/09638288.2018.1481149. PMID 29929450. S2CID 49342524.
- ↑ Geraghty K, Scott MJ (February 2020). "Treating medically unexplained symptoms via improving access to psychological therapy (IAPT): major limitations identified". BMC Psychology. 8 (1): 13. doi:10.1186/s40359-020-0380-2. PMC 7001321. PMID 32020880.
- ↑ Kindlon T, Goudsmit EM (February 2010). "Graded exercise for chronic fatigue syndrome: too soon to dismiss reports of adverse reactions". Journal of Rehabilitation Medicine. 42 (2): 184, author reply 184–6. doi:10.2340/16501977-0493. PMID 20140417. Retrieved 17 July 2020.
- ↑ Geraghty KJ, Blease C (January 2018). "Cognitive behavioural therapy in the treatment of chronic fatigue syndrome: A narrative review on efficacy and informed consent". Journal of Health Psychology. 23 (1): 127–138. doi:10.1177/1359105316667798. PMID 27634687. S2CID 31832147.
- ↑ Coyne JC (27 September 2017). "Parents should have been warned about unprofessional providers in Esther Crawley's SMILE trial". Coyne of the Realm. Retrieved 18 July 2020.
- ↑ "Medical Treatments: Children:Written question - HL15894". UK Parliament. 21 May 2019. Archived from the original on 18 July 2020. Retrieved 18 July 2020.
- 1 2 Tuller D (13 December 2019). "BMJ should retract flawed paper on chronic fatigue syndrome". STAT. Retrieved 18 July 2020.
Unfortunately for BMJ, in addition to the mess over the Lightning Process study, Crawley was also directed earlier this year to correct the ethics statements in eleven other published papers – five of them in BMJ journals.
- ↑ McEvedy CP, Beard AW (January 1970). "Concept of benign myalgic encephalomyelitis". British Medical Journal. 1 (5687): 11–5. doi:10.1136/bmj.1.5687.11. PMC 1700895. PMID 5411596.
- ↑ Scott BD (January 1970). "Epidemic malaise". British Medical Journal. 1 (5689): 170. doi:10.1136/bmj.1.111.170. PMC 1699088. PMID 5370039.
- ↑ Compston ND, Dimsdale HE, Ramsay AM, Richardson AT (February 1970). "Epidemic Malaise". British Medical Journal. 1 (5692): 362–363. doi:10.1136/bmj.1.5692.362-a. PMC 1699022.
- ↑ Acheson ED (February 1970). "Epidemic Malaise". British Medical Journal. 1 (5692): 363–4. doi:10.1136/bmj.1.5692.363-b. PMC 1698971.
- ↑ Gosling PH (February 1970). "Epidemic malaise". British Medical Journal. 1 (5694): 499–500. doi:10.1136/bmj.1.5694.499-b. PMC 1699452. PMID 5435167.
- ↑ Purke GJ (February 1970). "Epidemic malaise". British Medical Journal. 1 (5694): 500. doi:10.1136/bmj.1.5694.500. PMC 1699458. PMID 5435168.
- ↑ Hopkins EJ (February 1970). "Epidemic malaise". British Medical Journal. 1 (5694): 500–1. doi:10.1136/bmj.1.5694.500-a. PMC 1699426. PMID 5435169.
- ↑ Galpine JF (February 1970). "Epidemic malaise". British Medical Journal. 1 (5694): 501. doi:10.1136/bmj.1.5694.501. PMC 1699416. PMID 5435170.
- ↑ Poskanzer DC (May 1970). "Epidemic malaise". British Medical Journal. 2 (5706): 420–1. doi:10.1136/bmj.2.5706.420-b. PMC 1700311. PMID 5420612.
- ↑ Parish JG (July 1970). "Epidemic malaise". British Medical Journal. 3 (5713): 47–8. doi:10.1136/bmj.3.5713.47-c. PMC 1700986. PMID 4316803.
- ↑ Hooper M (May 2007). "Myalgic encephalomyelitis: a review with emphasis on key findings in biomedical research". Journal of Clinical Pathology. 60 (5): 466–71. doi:10.1136/jcp.2006.042408. PMC 1994528. PMID 16935967.
- ↑ Evengård B, Schacterle RS, Komaroff AL (November 1999). "Chronic fatigue syndrome: new insights and old ignorance". Journal of Internal Medicine. 246 (5): 455–69. doi:10.1046/j.1365-2796.1999.00513.x. PMID 10583715.
- ↑ David AS, Wessely S, Pelosi AJ (March 1988). "Postviral fatigue syndrome: time for a new approach". British Medical Journal. 296 (6623): 696–9. doi:10.1136/bmj.296.6623.696. PMC 2545306. PMID 3128374.
- ↑ Stricklin A, Sewell M, Austad C (January 1990). "Objective measurement of personality variables in epidemic neuromyasthenia patients". South African Medical Journal = Suid-Afrikaanse Tydskrif vir Geneeskunde. 77 (1): 31–4. PMID 2294610.
- ↑ No authors listed (June 1978). "Epidemic myalgic encephalomyelitis". British Medical Journal. 1 (6125): 1436–7. doi:10.1136/bmj.1.2791.1436-a. PMC 1604957. PMID 647324.
- ↑ Showalter E (1997). Hystories: hysterical epidemics and modern media. New York: Columbia University Press. pp. 132. ISBN 978-0-231-10459-3.
- ↑ "Inquiry into the status of CFS/ME and research into causes and treatment". United Kingdom Parliamentary Group on Scientific Research into Myalgic Encephalomyelitis. 1 November 2006. Retrieved 25 June 2010.
- ↑ Kelland K (13 March 2019). "Sick and tired: Online activists are silencing us, scientists say". Reuters.
Further reading
- Johnson H (1996). Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic. Crown Publishers, New York. ISBN 978-0-517-70353-3.