 | |
| Clinical data | |
|---|---|
| Trade names | Zaditor[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a604033 |
| Pregnancy category |
|
| Routes of administration | By mouth (tablets), topical eye drops |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 60% |
| Protein binding | 75% |
| Metabolism | Hepatic |
| Elimination half-life | 12 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.047.348 |
| Chemical and physical data | |
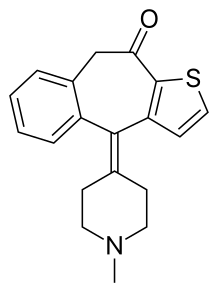
| Formula | C19H19NOS |
| Molar mass | 309.43 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Ketotifen is an antihistamine medication and a mast cell stabilizer commonly used to treat allergic conditions such as conjunctivitis, asthma, and urticaria (hives). Ketotifen is available in ophthalmic (eye drops or drug-eluting contact lenses) and oral (tablets or syrup) forms: the ophthalmic form relieves eye itchiness and irritation associated with seasonal allergies, while the oral form helps prevent systemic conditions such as asthma attacks and allergic reactions. In addition to treating allergies, ketotifen has shown efficacy in managing systemic mast cell diseases such as mastocytosis and mast cell activation syndrome (MCAS), which involve abnormal accumulation or activation of mast cells throughout the body. Ketotifen is also used for other allergic-type conditions like atopic dermatitis (eczema) and food allergies.
Ketotifen acts by blocking the H1 histamine receptors, which are found on various cells in the body, such as smooth muscle, endothelium, and nerve cells, so that ketotifen prevents the binding of histamine to these receptors and thus reduces the symptoms of histamine-mediated allergic reactions, such as itching, sneezing, wheezing, and swelling. Ketotifen also prevents the release of histamine and other inflammatory substances from immune cells called mast cells; this action helps reduce symptoms of allergic conditions by blocking the activation of these cells. In addition to its antihistaminic activity, ketotifen also functions as a leukotriene antagonist, which blocks inflammation-causing chemicals known as leukotrienes; it also acts as a phosphodiesterase inhibitor that regulates blood vessel dilation.
While generally well-tolerated, ketotifen can have side effects, including drowsiness, weight gain, dry mouth, irritability, increased nosebleeds when taken orally, and temporary burning or stinging sensations in the eyes when used topically. Ketotifen has contraindications for individuals with certain medical conditions, such as acute porphyrias or epilepsy. Controversies surrounding ketotifen include its classification as a first-generation or second-generation antihistamine due to varying criteria of classification.
Research on ketotifen continues to explore its impact on appetite regulation and effectiveness against specific medical conditions like irritable bowel syndrome. Despite inconclusive evidence regarding its efficacy in asthma treatment compared to other medications like montelukast, long-term administration of oral ketotifen has shown positive outcomes in reducing corticosteroid use while improving clinical symptoms related to asthma management.
Medical uses
Ketotifen, an antihistamine medication and a mast cell stabilizer, is most commonly sold as a salt with fumaric acid, ketotifen fumarate, and is available in two forms: in its ophthalmic form (eye drops), it is used to treat allergic conjunctivitis;[1] in its oral form (tablets or syrup), it is used to prevent asthma attacks or anaphylaxis,[2][3] as well as various mast cell, allergic-type disorders.[4][5][6]
Ketotifen is a medication that can be administered topically as an ophthalmic solution in the form of eye drops, or as disposable drug-eluting contact lenses.[7][8] Ketotifen is also available for oral administration through tablets or syrup. The topical form allows direct application to the eyes, while the oral forms provide systemic distribution throughout the body via absorption in the gastrointestinal tract.[9]
Ketotifen ophthalmic solution relieves and prevents eye itchiness and/or irritation associated with most seasonal allergies. It starts working within minutes after administering the drops. Ketotifen in the form of eye drops has not been studied in children under 3 years old,[1] whereas drug-eluting contact lenses have not been studied in children under 11.[8]
Drug-eluting contact lenses, which release ketotifen medication, are used to help prevent itchy eyes caused by allergies. The lenses can also correct vision problems like nearsightedness and farsightedness. These lenses are meant for people who don't have red eyes, can comfortably wear contact lenses, and have less than 1 degree of astigmatism.[8]
Oral ketotifen is used to treat asthma, allergic rhinitis, allergic conjunctivitis, atopic dermatitis, chronic urticaria (hives), cold-induced urticaria, cholinergic urticaria, exercise-induced urticaria, systemic mast cell diseases such as mastocytosis and mast cell activation syndrome (MCAS), as well as allergic and nonallergic anaphylaxis. Ketotifen has also shown efficacy in managing angioedema and food allergies. As a mast cell stabilizer to treat MCAS, oral ketotifen prevents the release of histamine and other inflammatory substances from mast cells, which are immune cells that react to allergens, therefore, ketotifen, by blocking a calcium channel essential for mast cell activation, helps reduce symptoms of allergic conditions such as asthma, hay fever, and conjunctivitis caused by mast cell activation. In Canada, Europe, and Mexico, oral ketotifen is commonly prescribed for these indications.[10][6][2] In patients with MCAS, ketotifen reduce episodes of flushing, gastrointestinal symptoms (such as abdominal pain, diarrhea), respiratory symptoms (such as wheezing), and other systemic manifestations. Still, treatment plans for MCAS typically involve a combination of medications targeting different aspects of mast cell activation along with lifestyle modifications to minimize triggers.[11]
Oral ketotifen is available at compounding pharmacies in the United States with a prescription requirement, still, the use of ketotifen is only approved by the FDA for adults and older children with asthma or allergic conditions. The recommended dosage for this population is 1 mg taken orally twice daily. However, the FDA advises evaluation regarding its use in managing chronic hives (urticaria).[6][2]
Oral ketotifen can be used as a long-term control medication for asthma and wheeze in children, and it has been shown to improve the control of asthma by reducing the need for bronchodilators, decreasing symptoms, preventing exacerbations, and reducing the use of rescue oral steroids, ketotifen has also been found to be effective when used alone or in combination with other medications. Oral ketotifen is an alternative to inhaled therapy for asthma in children, especially for younger children who may have difficulty using inhalers.[12]
The mean elimination half-life of ketotifen is 12 hours.[13] Besides its anti-histaminic activity, it is also a functional leukotriene antagonist (a medication that blocks the action of leukotrienes, which are chemicals that cause inflammation and narrowing of the airways in some allergic and respiratory conditions)[14] and a phosphodiesterase inhibitor (a medication that blocks the enzymes that regulate the levels of cAMP and cGMP, which are molecules that control blood vessel dilation and smooth muscle relaxation in the body).[15]
Contraindications
The eye drops are generally contraindicated for individuals who have a known hypersensitivity to ketotifen or any other ingredient in the formulation, as well as for those who experience irritation from wearing contact lenses. Eye drops are not recommended for use in children under 3 years of age,[16][17][18] whereas drug-eluting contact lenses are not recommended for under 11 years of age.[8]
For oral ketotifen, the contraindication is for known hypersensitivity to any component of the product. Caution should be taken on the following conditions: acute porphyrias (a group of rare disorders that occur when the body cannot make enough of a substance called heme, which is needed for red blood cells to carry oxygen, this causes a build-up of chemicals called porphyrins, which can damage the nerves and the skin), epilepsy (a disorder causing recurrent seizures), prostatic hypertrophy (in adults), pyloroduodenal obstruction (a condition where the passage of food from the stomach to the small intestine is blocked by something, such as a muscle, an ulcer, a tumor, or a gallstone), susceptibility to angle-closure glaucoma (a condition where the iris, the colored part of the eye, bulges and blocks the drainage of fluid from the eye, causing high pressure and damage to the optic nerve, a nerve that connects the eye to the brain), and urinary retention (inability to urinate).[16]
The use of ketotifen eye drops during pregnancy and lactation is considered safe, as absorption through the eye is limited. It is unlikely to cause any adverse effects in breastfeeding infants after maternal use. To minimize the amount of medication transferred to breast milk when using eye drops, apply pressure on the tear duct near the corner of the eye for at least one minute and remove any excess solution with a tissue.[19] Ketotifen safety when taken via the oral route (tablets or syrup) during pregnancy and lactation remains unknown; therefore, it is not recommended to use ketotifen orally during these periods until sufficient safety data becomes available.[19]
Side effects
Common side effects of ophthalmic use are eye redness and swelling. Less common are eye discharge, eye discomfort, eye pain, hives, increased itching of eyes, and rash. Ophthalmic use of ketotifen may also cause burning, stinging, or itching of the eyes, blurred vision, or increased sensitivity to light.[17]
Side effects of systemic (oral) use include drowsiness, weight gain (5.0–5.4 kilograms (11.0–11.9 lb)), dry mouth, irritability, and increased nosebleeds.[20] Systemic use of ketotifen may also cause abdominal pain, nausea, vomiting, constipation, diarrhea, headache, dizziness, or fatigue. In rare cases, systemic use of ketotifen may cause serious side effects such as anaphylaxis, liver dysfunction, blood disorders, or seizures. Systemic use of ketotifen may interact with other drugs that cause sedation, such as alcohol, antihistamines, opioids, benzodiazepines, or antidepressants. Systemic use of ketotifen may affect the results of some laboratory tests, such as skin tests for allergies or blood glucose levels.[21]
Overdose
The symptoms of ketotifen overdose are dose-dependent and may vary from mild to severe. The onset of symptoms may be delayed for several hours after ingestion, and the duration of symptoms may last for more than 24 hours.[22][23]
The most common symptom of ketotifen overdose is significant sedation, which may impair the mental and physical abilities of the patient. Other symptoms may include confusion, disorientation, agitation, hallucinations, ataxia (impairment of voluntary muscle movement), tremor (involuntary regular muscle contraction), myoclonus (involuntary, irregular muscle twitch), nystagmus (dysfunction of eye movement), dysarthria (poor speech), and slurred speech.[22][23]
Other symptoms of ketotifen overdose may include tachycardia (fast, pounding, or irregular heartbeat or pulse), hypotension (low blood pressure), convulsions, hyperexcitability (particularly in children), reversible coma, unusual tiredness or weakness, blurred vision, dizziness or fainting, loss of consciousness.[23]
The symptoms of ketotifen overdose may be described according to the affected system of the body. The cardiovascular effects of ketotifen overdose may include tachycardia, hypotension, arrhythmias, and cardiac arrest. The respiratory effects may include respiratory depression, apnea, and pulmonary edema. The gastrointestinal effects may include nausea, vomiting, abdominal pain, diarrhea, and pancreatitis. The renal effects may include acute renal failure and urinary retention. The hepatic effects may include hepatitis and jaundice. The hematologic effects may include anemia, leukopenia, thrombocytopenia, and coagulopathy. The neurologic effects of ketotifen overdose may include convulsions, hyperexcitability, coma, and death. The risk of seizures is higher in children, especially those with a history of epilepsy or febrile seizures. The risk of coma and death is higher in adults, especially those with pre-existing medical conditions or concomitant use of other drugs that cause sedation or lower the seizure threshold.[22][23]
No fatal overdoses of ketotifen have been reported. In case of an overdose, if ingestion is recent, gastric lavage or activated charcoal can be used as a treatment. Other treatments should be supportive and administered as necessary based on symptoms. The patient is monitored closely for vital signs, oxygen saturation, electrocardiogram, blood glucose, electrolytes, renal and liver function, and coagulation status. The patient is given intravenous fluids, oxygen, and vasopressors if needed. The patient is given benzodiazepines or barbiturates to control seizures, and naloxone to reverse respiratory depression. The patient is given bicarbonate to correct metabolic acidosis, and vitamin K to correct coagulopathy. The patient is given hemodialysis or hemoperfusion if the overdose is severe or if there is renal failure.[22][23]
Interactions
In systemic (oral) administration, ketotifen may interact with amphetamine and benzphetamine, which may decrease the activities of ketotifen.[24][25]
Systemic use of ketotifen may also interact with other drugs that cause sedation, such as alcohol, antihistamines, opioids, benzodiazepines, or antidepressants. These interactions may increase the risk of drowsiness, dizziness, confusion, or impaired mental and physical abilities. Therefore, caution is advised when using ketotifen with these drugs, and the dose of ketotifen or the other drugs may need to be adjusted. Patients should also avoid driving or operating machinery while taking ketotifen or other sedating drugs.[9]
Systemic use of ketotifen may decrease the effectiveness of benzylpenicilloyl polylysine as a diagnostic agent.[24] Ketotifen may affect the results of some laboratory tests, such as skin tests for allergies or blood glucose levels. Ketotifen may interfere with the skin test reactions by suppressing the histamine response, leading to false-negative results. Therefore, ketotifen should be discontinued at least 72 hours before performing skin tests. Ketotifen may also increase the blood glucose levels by inhibiting the insulin secretion, leading to hyperglycemia. Therefore, ketotifen should be used with caution in patients with diabetes mellitus, and blood glucose levels should be monitored regularly.[9]
Ophthalmic use of ketotifen may interact with contact lenses, as the eye drops may contain preservatives that can be absorbed by soft contact lenses and cause eye irritation. Therefore, contact lenses should be removed before applying the eye drops, and should not be reinserted until 15 minutes after the application.[26]
Pharmacology
Ketotifen is a selective antihistamine – that is, an inverse agonist of the histamine H1 receptor (Ki = 0.166 nM)[27] – and mast cell stabilizer.[28][29] In addition, ketotifen has weak anticholinergic (Ki = 204 nM for mACh) and antiserotonergic (Ki = 38.9 nM for 5-HT2A) activity.[27][30] However, at the dosages in which it is typically used clinically, both the anticholinergic and antiserotonergic activity of ketotifen are said not to be appreciable.[31]
Ketotifen is a lipophilic compound that can cross the blood-brain barrier and exert central nervous system effects, such as sedation, weight gain, and anticonvulsant activity. Ketotifen also has peripheral effects, such as inhibition of platelet aggregation, modulation of cytokine production, and enhancement of mucociliary clearance.[9]
Ketotifen acts as a mast cell stabilizer by preventing the degranulation and release of histamine and other inflammatory mediators, such as leukotrienes, prostaglandins, and cytokines, from mast cells. Ketotifen also inhibits the activation and migration of eosinophils, basophils, and neutrophils, which are involved in the inflammatory response and tissue damage in allergic and respiratory diseases.[9]
Ketotifen has a dual mode of action as an antihistamine and a mast cell stabilizer, which makes it effective in the prophylaxis and treatment of various allergic and respiratory conditions, such as asthma, allergic rhinitis, conjunctivitis, dermatitis, urticaria, and anaphylaxis. Ketotifen can also reduce the bronchial hyperreactivity and airway inflammation that are characteristic of chronic asthma.[9]
Ketotifen has plasma half-life of about 12 hours. Ketotifen is extensively metabolized in the liver by oxidation and conjugation, and the metabolites are excreted in the urine and feces. The bioavailability of oral ketotifen is about 50% due to hepatic first-pass metabolism. Peak plasma concentration is reached in about 2 to 4 hours. The pharmacokinetics of ketotifen are not significantly affected by age, gender, or renal impairment, but may be altered by hepatic impairment or concomitant use of other drugs.[9][32]
Ketotifen is mainly metabolized by the cytochrome P450 (CYP) enzymes, especially CYP3A4 and CYP2D6, in the liver. These enzymes are responsible for the oxidation and demethylation of ketotifen, producing the major metabolites norketotifen and 10-hydroxyketotifen. Norketotifen is pharmacologically active and has a similar potency as ketotifen, while 10-hydroxyketotifen is inactive. The metabolites are then conjugated with glucuronic acid or sulfate and excreted in the urine and feces. The metabolism of ketotifen may be affected by genetic polymorphisms of CYP2D6, which can result in different phenotypes of poor, intermediate, extensive, or ultra-rapid metabolizers. The metabolism of ketotifen may also be influenced by the concomitant use of other drugs that inhibit or induce CYP3A4 or CYP2D6, such as ketoconazole, erythromycin, rifampicin, or fluoxetine. These interactions may alter the pharmacokinetics and pharmacodynamics of ketotifen and its metabolites, and may require dose adjustment or monitoring.[9]
Classification

Ketotifen is a noncompetitive H1-antihistamine and mast cell stabilizer. There is no academic consensus on whether ketotifen should be classified as a medication belonging to the first[33][34][4] or the second generations of antihistamine drugs;[35][36] the classification can vary depending on the criteria used and the context of the study.[37]
Some studies classify ketotifen as a first-generation antihistamine,[33][34][4] but others classify it as a second-generation antihistamine.[35][36] The classification can vary depending on the criteria used and the context of the study, as the classification of antihistamines is primarily based on their chemical structure, pharmacological properties, and side effect profiles. Ketotifen is a tricyclic, benzocycloheptene-based compound with chemical structures similar to first-generation antihistamines such as azatadine, cyproheptadine, chlorpheniramine and diphenhydramine, and other compounds with antihistamine properties such as pizotifen. The sedative effects of ketotifen is also a reason in differences in classification. First-generation antihistamines are well known for their sedating side effects due to their ability to penetrate the blood–brain barrier.[38] While ketotifen has some sedative properties, it is generally considered to have a milder sedative effect compared to traditional first-generation antihistamines,[37][21] so this reduced sedation is one of the reasons why ketotifen is sometimes classified as a second-generation antihistamine.[39]
Research directions
Increased appetite and weight gain
The underlying mechanisms of why ketotifen (similarly to other antihistamine drugs such as astemizole, azelastine)[37] may increase appetite and lead to weight gain in some people, are not fully understood.[37]
Different studies have shown conflicting results about the amount of weight gain caused by ketotifen. In one study (postmarketing surveillance),[37] it was found that around 1 to 2 out of every 100 people who took the drug experienced weight gain, with adults gaining about 1 kilogram (2.2 lb) and children over the age of one gaining 2.8–3.3 kilograms (6.2–7.3 lb). However, in another study,[20] adults gained a higher amount of weight: 5.0–5.4 kilograms (11.0–11.9 lb).[20]
Ketotifen exhibits a chemical resemblance to pizotifen, a substance known for its appetite-stimulating properties.[37] One proposed mechanism involves the inhibitory effect of ketotifen on the production of TNF-α, which is a cytokine that plays a role in regulating energy metabolism. TNF-α can act directly on adipocytes (fat cells) to regulate the release of leptin. Leptin is a hormone produced by adipose tissue and acts as a satiety signal by binding to receptors in the hypothalamus, where it inhibits appetite. By reducing TNF-α production, ketotifen may lead to decreased leptin levels, reducing appetite control inhibition. Furthermore, ketotifen's influence on serotonin regulation could be involved in central serotonin disinhibition. Serotonin is known to have suppressant effects on appetite. It is suggested that ketotifen might cause a decrease in serotonin levels due to this regulatory influence. As a result, the decrease in serotonin function may lead to increased food intake tendency and heightened appetite. Still, these potential mechanisms have been hypothesized based on limited evidence.[40] Studies on mice suggest that caffeine[40] or Citrus aurantifolia oil[41] may prevent prevent weight-gain induced by ketotifen, but, this has not been confirmed on human subjects.[41]
Norketotifen
Research directions for ketotifen include the investigation of norketotifen (NK), a metabolite of ketotifen. In vitro studies using human liver microsomes and hepatocytes suggest that NK may be the major demethylated hepatic metabolite of ketotifen. Unlike ketotifen, NK does not seem to induce severe sedative effects, potentially allowing for higher doses to be administered without sedation as a limiting factor. Furthermore, NK may probably have potent and dose-dependent inhibition of the release of the pro-inflammatory cytokine TNF-α, suggesting potential anti-inflammatory activity. Thus, ketotifen can probably be considered a sedating prodrug that is converted to NK, a nonsedating metabolite with anti-inflammatory properties, when used as an anti-inflammatory medication.[42]
Conditions
Ketotifen's efficacy in asthma remains inconclusive despite extensive testing,[37][43][44] however, the research is ongoing. Long-term administration of oral ketotifen in the prophylaxis of asthma has shown positive outcomes, allowing for a reduction in corticosteroid and bronchodilator use while improving clinical symptoms and maintaining respiratory function. Still, a lengthy period (8 to 12 weeks) is needed until the drug develops its anti-asthmatic effects.[21][45] Tolerance does not develop, and there is no rebound effect upon treatment interruption. The antihistaminic properties alone do not account for its effectiveness; mast cell stabilization or other mechanisms may be involved. The exact mechanisms are poorly understood. Comparative trials suggest similar efficacy to disodium cromoglycate.[45] Ketotifen demonstrates limited efficacy in addressing exercise-induced asthma and does not effectively reduce bronchial hyperactivity.[46][47] Other drugs, such as montelukast, can be more effective than ketotifen in treating asthma.[48] In children, oral ketotifen when used alone or in combination with other interventions, leads to better control of asthma symptoms and wheezing compared to placebo. Children treated with ketotifen are more likely to reduce or stop their use of bronchodilators within 12-16 weeks of treatment, but the most common side effects when treating asthma in children are sedation and weight gain. As such, ketotifen offers benefits for long-term control of asthma and wheezing in children due to its effectiveness in improving symptom control and reducing reliance on rescue medications.[12]
There is research on the potential application of ketotifen in relieving irritable bowel syndrome, still the results are inconclusive.[49][50]
It was hypothesized that ketotifen may be effective against SARS-CoV-2, a virus behind the COVID-19 pandemic, but there were no studies to confirm the hypothesis; the research did not proceed behind in-vitro experiments.[51]
Society and culture

Ketotifen was patented in 1970 and came into medical use in 1976.[52] In 2020, it was the 289th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[53][54] Ketotifen is sold under the brand name Zaditor among many others worldwide.[55]
There was a litigation related to ketotifen. In 2021, the plaintiff, Edward C. Hanks, brought an action in the United States District Court, C.D. Illinois, against the defendants, Ned Hubbard and others, alleging that they violated his rights under the Eighth Amendment of the U.S. Constitution by acting with deliberate indifference to his serious medical needs. The plaintiff claimed that he suffered from a chronic eye condition that required medical attention and that the defendant, Dr. Hubbard, prescribed him ketotifen. The plaintiff further claimed that the ketotifen eye drops caused him adverse reactions, such as severe pain, burning, and blurred vision, and that the defendant, Dr. Hubbard, failed to offer him an alternative medication or refer him to an ophthalmologist. The plaintiff also claimed that he sustained permanent eye damage as a result of the ketotifen. The district court granted the defendant's motion to dismiss, finding that the plaintiff failed to state a claim upon which relief could be granted. The plaintiff appealed to the U.S. Court of Appeals for the Seventh Circuit, which affirmed the district court's judgment on 7 February 2022.[56]
References
- 1 2 3 "Zaditor- ketotifen fumarate solution". DailyMed. 13 February 2020. Retrieved 4 September 2020.
- 1 2 3 Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau AM, et al. (October 2009). "EAACI/GA(2)LEN/EDF/WAO guideline: management of urticaria". Allergy. 64 (10): 1427–1443. doi:10.1111/j.1398-9995.2009.02178.x. PMID 19772513. S2CID 14587946.
- ↑ Li Z, Celestin J (23 February 2015). Ketotifen: A Role in the Treatment of Idiopathic Anaphylaxis. American Academy of Allergy, Asthma & Immunology Annual Meeting. Houston.
- 1 2 3 Sokol KC, Amar NK, Starkey J, Grant JA (December 2013). "Ketotifen in the management of chronic urticaria: resurrection of an old drug". Annals of Allergy, Asthma & Immunology. 111 (6): 433–436. doi:10.1016/j.anai.2013.10.003. PMC 4309375. PMID 24267353.
- ↑ Shawky RM, Seifeldin NS (2015). "The relation between antihistamine medication during early pregnancy & birth defects". Egyptian Journal of Medical Human Genetics. 16 (4): 287–90. doi:10.1016/j.ejmhg.2015.04.003.
- 1 2 3 Zuberbier T (January 2012). "A Summary of the New International EAACI/GA(2)LEN/EDF/WAO Guidelines in Urticaria". The World Allergy Organization Journal. 5 (Suppl 1): S1–S5. doi:10.1186/1939-4551-5-S1-S1. PMC 3488932. PMID 23282889.
- ↑ Ono J, Toshida H (July 2022). "Use of Ketotifen Fumarate-Eluting Daily Disposable Soft Contact Lens in Management of Ocular Allergy: Literature Review and Report of Two Cases". Cureus. 14 (7): e27093. doi:10.7759/cureus.27093. PMC 9391663. PMID 36000122.
- 1 2 3 4 "DailyMed - ketotifen fumarate drug-eluting contact lens". dailymed.nlm.nih.gov.
- 1 2 3 4 5 6 7 8 "Ketotifen".
- ↑ El-Alali EA, Abukhiran IM, Alhmoud TZ (July 2021). "Successful use of montelukast in eosinophilic gastroenteritis: a case report and a literature review". BMC Gastroenterology. 21 (1): 279. doi:10.1186/s12876-021-01854-x. PMC 8265096. PMID 34238222.
- ↑ Frieri M (June 2018). "Mast Cell Activation Syndrome". Clin Rev Allergy Immunol. 54 (3): 353–365. doi:10.1007/s12016-015-8487-6. PMID 25944644. S2CID 5723622.
- 1 2 Schwarzer G, Bassler D, Mitra A, Ducharme FM, Forster J (2004). "Ketotifen alone or as additional medication for long-term control of asthma and wheeze in children". Cochrane Database Syst Rev. 2004 (1): CD001384. doi:10.1002/14651858.CD001384.pub2. PMC 8406918. PMID 14973969.
- ↑ Grahnén A, Lönnebo A, Beck O, Eckernäs SA, Dahlström B, Lindström B (May 1992). "Pharmacokinetics of ketotifen after oral administration to healthy male subjects". Biopharmaceutics & Drug Disposition. 13 (4): 255–262. doi:10.1002/bdd.2510130404. PMID 1600111. S2CID 72293850.
- ↑ Fink A, Bibi H, Eliraz A, Schlesinger M, Bentwich Z (August 1986). "Ketotifen, disodium cromoglycate, and verapamil inhibit leukotriene activity: determination by tube leukocyte adherence inhibition assay". Annals of Allergy. 57 (2): 103–106. PMID 3090908.
- ↑ Castillo JG, Gamboa PM, García BE, Oehling A (1990). "Effect of ketotifen on phosphodiesterase activity from asthmatic individuals". Allergologia et Immunopathologia. 18 (4): 197–201. PMID 1702263.
- 1 2 "Ketotifen Monograph for Professionals".
- 1 2 "Ketotifen ophthalmic Uses, Side Effects & Warnings".
- ↑ "Ketotifen - Mechanism, Indication, Contraindications, Dosing, Adverse Effect, Interaction, Hepatic Dose; Drug Index; Pediatric Oncall". Pediatric Oncall.
- 1 2 Ketotifen. National Institute of Child Health and Human Development. 2006. PMID 30000587. NCBI NBK501527.
- 1 2 3 "Zaditen - MIMS online". www.mims.co.uk.
- 1 2 3 Grant SM, Goa KL, Fitton A, Sorkin EM (September 1990). "Ketotifen. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in asthma and allergic disorders". Drugs. 40 (3): 412–448. doi:10.2165/00003495-199040030-00006. PMID 2226222. S2CID 242916740.
- 1 2 3 4 Le Blaye I, Donatini B, Hall M, Krupp P (1992). "Acute ketotifen overdosage. A review of present clinical experience". Drug Safety. 7 (5): 387–392. doi:10.2165/00002018-199207050-00007. PMID 1418695. S2CID 25839342.
- 1 2 3 4 5 Jeffreys DB, Volans GN (May 1981). "Ketotifen overdose: surveillance of the toxicity of a new drug". British Medical Journal. 282 (6278): 1755–1756. doi:10.1136/bmj.282.6278.1755. PMC 1505736. PMID 6113023.
- 1 2 Greenwood C (July 1982). "The pharmacology of ketotifen". Chest. 82 (1 Suppl): 45S–48S. doi:10.1378/chest.82.1_supplement.45s. PMID 6123414.
- ↑ Rogóz Z, Skuza G, Sowińska H (1981). "Central action of ketotifen". Polish Journal of Pharmacology and Pharmacy. 33 (5): 503–515. PMID 7335554.
- ↑ "Ketotifen Ophthalmic: Generic, Uses, Side Effects, Dosages, Interactions, Warnings".
- 1 2 Kakiuchi M, Ohashi T, Musoh K, Kawamura K, Morikawa K, Kato H (April 1997). "Studies on the novel antiallergic agent HSR-609: its penetration into the central nervous system in mice and guinea pigs and its selectivity for the histamine H1-receptor". Japanese Journal of Pharmacology. 73 (4): 291–298. doi:10.1254/jjp.73.291. PMID 9165365.
- ↑ Nelson WL (2008). "Antihistamines and Related Antiallergic and Antiulcer Agents". In Lemke TL, Williams DA (eds.). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1019–. ISBN 978-0-7817-6879-5.
- ↑ Ang DC, Hilligoss J, Stump T (September 2015). "Mast Cell Stabilizer (Ketotifen) in Fibromyalgia: Phase 1 Randomized Controlled Clinical Trial". The Clinical Journal of Pain. 31 (9): 836–842. doi:10.1097/AJP.0000000000000169. PMC 4417653. PMID 25370135.
- ↑ Alagarsamy V (16 June 2012). "Antihistamines". Textbook of Medicinal Chemistry Vol II - E-Book. Elsevier Health Sciences. pp. 38–. ISBN 978-81-312-3259-0.
- ↑ Drews J (6 December 2012). "Substances with an Antialergic Effect". Immunopharmacology: Principles and Perspectives. Springer Science & Business Media. pp. 282–. ISBN 978-3-642-75561-3.
- ↑ Fahmy RH, Badr-Eldin SM (August 2014). "Novel delivery approach for ketotifen fumarate: dissofilms formulation using 3² experimental design: in vitro/in vivo evaluation". Pharm Dev Technol. 19 (5): 521–30. doi:10.3109/10837450.2013.800108. PMID 23713715. S2CID 45012360.
- 1 2 Bittner L, Teixidó E, Keddi I, Escher BI, Klüver N (May 2019). "pH-Dependent Uptake and Sublethal Effects of Antihistamines in Zebrafish (Danio rerio) Embryos". Environmental Toxicology and Chemistry. 38 (5): 1012–1022. doi:10.1002/etc.4395. PMID 30779379. S2CID 73482611.
- 1 2 Pinke KH, Zorzella-Pezavento SF, de Campos Fraga-Silva TF, Mimura LA, de Oliveira LR, Ishikawa LL, et al. (January 2020). "Calming Down Mast Cells with Ketotifen: A Potential Strategy for Multiple Sclerosis Therapy?". Neurotherapeutics. 17 (1): 218–234. doi:10.1007/s13311-019-00775-8. PMC 7007452. PMID 31463682.
- 1 2 Janeczko P, Norris MR, Bielory L (October 2021). "Assessment of receptor affinities of ophthalmic and systemic agents in dry eye disease". Current Opinion in Allergy and Clinical Immunology. 21 (5): 480–485. doi:10.1097/ACI.0000000000000773. PMID 34387278. S2CID 236998913.
- 1 2 Triantafillou V, Maina IW, Patel NN, Tong CC, Papagiannopoulos P, Kohanski MA, et al. (February 2020). "In vitro safety of ketotifen as a topical nasal rinse". International Forum of Allergy & Rhinology. 10 (2): 265–270. doi:10.1002/alr.22461. PMID 32086998. S2CID 211246051.
- 1 2 3 4 5 6 7 Slater JW, Zechnich AD, Haxby DG (January 1999). "Second-generation antihistamines: a comparative review". Drugs. 57 (1): 31–47. doi:10.2165/00003495-199957010-00004. PMID 9951950. S2CID 24659435.
- ↑ Sagara A, Nagahama A, Aki H, Yoshimura H, Hiraide M, Shimizu T, et al. (October 2023). "Potential risk of driving performance under combined conditions of taking second-generation antihistamines and attending calls using a hands-free function". Traffic Injury Prevention. 25 (1): 36–40. doi:10.1080/15389588.2023.2265002. PMID 37815801. S2CID 263801715.
- ↑ Aelony Y (September 1998). "First-generation vs second-generation antihistamines". Archives of Internal Medicine. 158 (17): 1949–1950. doi:10.1001/archinte.158.17.1949. PMID 9759694.
- 1 2 Habibi Asl B, Vaez H, Imankhah T, Hamidi S (2014). "Impact of caffeine on weight changes due to ketotifen administration". Advanced Pharmaceutical Bulletin. 4 (1): 83–89. doi:10.5681/apb.2014.013. PMC 3885374. PMID 24409414.
- 1 2 Asnaashari S, Delazar A, Habibi B, Vasfi R, Nahar L, Hamedeyazdan S, Sarker SD (December 2010). "Essential oil from Citrus aurantifolia prevents ketotifen-induced weight-gain in mice". Phytotherapy Research. 24 (12): 1893–1897. doi:10.1002/ptr.3227. PMID 20623616. S2CID 8888404.
- ↑ Aberg AK, Arulnesan N, Bolger GT, Ciofalo VB, Pucaj K, Walle K, Walle T (April 2022). "Ketotifen is a Prodrug. Norketotifen is the active metabolite". Drug Development Research. 83 (2): 362–367. doi:10.1002/ddr.21865. PMID 34410005. S2CID 237216445.
- ↑ Canny GJ, Reisman J, Levison H (January 1997). "Does ketotifen have a steroid-sparing effect in childhood asthma?". The European Respiratory Journal. 10 (1): 65–70. doi:10.1183/09031936.97.10010065. PMID 9032494.
- ↑ Hoshino M, Nakamura Y, Shin Z, Fukushima Y (August 1997). "Effects of ketotifen on symptoms and on bronchial mucosa in patients with atopic asthma". Allergy. 52 (8): 814–820. doi:10.1111/j.1398-9995.1997.tb02152.x. PMID 9284980. S2CID 30563319.
- 1 2 Craps L (1983). "Prophylaxis of asthma with ketotifen in children and adolescents: a review". Pharmatherapeutica. 3 (5): 314–326. PMID 6405397.
- ↑ Petheram IS, Moxham J, Bierman CW, McAllen M, Spiro SG (April 1981). "Ketotifen in atopic asthma and exercise-induced asthma". Thorax. 36 (4): 308–312. doi:10.1136/thx.36.4.308. PMC 471498. PMID 6116296.
- ↑ Pérez-Padilla JR (1999). "[Ketotifen (Zaditen and K-Asthmal): a drug with sales disproportionate to its demonstrated effectiveness]". Gaceta Medica de Mexico (in Spanish). 135 (2): 165–170. PMID 10327750.
- ↑ Al-Hamdani FY (October 2010). "Comparative clinical evaluation of ketotifen and montelukast sodium in asthmatic Iraqi patients". Saudi Pharmaceutical Journal. 18 (4): 245–249. doi:10.1016/j.jsps.2010.07.001. PMC 3730982. PMID 23960734.
- ↑ Zhang L, Song J, Hou X (April 2016). "Mast Cells and Irritable Bowel Syndrome: From the Bench to the Bedside". Journal of Neurogastroenterology and Motility. 22 (2): 181–192. doi:10.5056/jnm15137. PMC 4819856. PMID 26755686.
- ↑ Klooker TK, Braak B, Koopman KE, Welting O, Wouters MM, van der Heide S, et al. (September 2010). "The mast cell stabiliser ketotifen decreases visceral hypersensitivity and improves intestinal symptoms in patients with irritable bowel syndrome" (PDF). Gut. 59 (9): 1213–1221. doi:10.1136/gut.2010.213108. PMID 20650926. S2CID 18889707.
- ↑ Kiani P, Scholey A, Dahl TA, McMann L, Iversen JM, Verster JC (March 2021). "In Vitro Assessment of the Antiviral Activity of Ketotifen, Indomethacin and Naproxen, Alone and in Combination, against SARS-CoV-2". Viruses. 13 (4): 558. doi:10.3390/v13040558. PMC 8065848. PMID 33810356.
- ↑ Alapi EM, Fischer J (2006). "Table of Selected Analogue Classes". In Fischer J, Ganellin CR (eds.). Analogue-based Drug Discovery. John Wiley & Sons. p. 548. ISBN 978-3-527-60749-5.
- ↑ "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- ↑ "Ketotifen - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- ↑ "Ketotifen International". Drugs.com. Retrieved 4 September 2020.
- ↑ Hanks v. Hubbard (C.D. Ill 8 March 2021).