| Glutaric acidemia type 2 | |
|---|---|
| Other names | Multiple acyl-CoA dehydrogenase deficiency (MADD);[1] Glutaric academia/aceduria type II (GA-II) |
 | |
| Glutaric acid | |
| Specialty | Medical genetics |
Glutaric acidemia type 2 is an autosomal recessive metabolic disorder that is characterised by defects in the ability of the body to use proteins and fats for energy. Incompletely processed proteins and fats can build up, leading to a dangerous chemical imbalance called acidosis. It is a metabolic myopathy, categorized under fatty acid metabolism disorder as that is the bioenergetic system that it affects the most. It also affects choline metabolism.[2]
The phenotypic presentation has 3 forms: a neonatal-onset form with congenital anomalies (type I), a neonatal-onset form without congenital anomalies (type II), and a late-onset form (type III).[3]
Individuals with glutaric acidemia type 2 frequently experience exercise-induced muscle fatigue, hypotonia, myalgia, and proximal muscle weakness.[4] The symptoms not only overlap with another type of metabolic myopathy, that of mitochondrial myopathy, but MADD also impairs the FAD-dependent respiratory chain in the mitochondria of muscle cells, as well as some muscle biopsies showing COX-negative fibres and deficiency of coenzyme Q10.[5][2]
Genetics
Mutations in the ETFA, ETFB, and ETFDH genes cause glutaric acidemia type II. Mutations in these genes result in a deficiency in one of two enzymes that normally work together in the mitochondria, which are the energy-producing centers of cells. The ETFA and ETFB genes encode two subunits of the enzyme electron transfer flavoprotein, while the ETFDH gene encodes the enzyme electron-transferring-flavoprotein dehydrogenase. When one of these enzymes is defective or missing, the mitochondria cannot function normally, partially broken-down proteins and fats accumulate in the cells and damage them; this damage leads to the signs and symptoms of glutaric acidemia type II.[1]
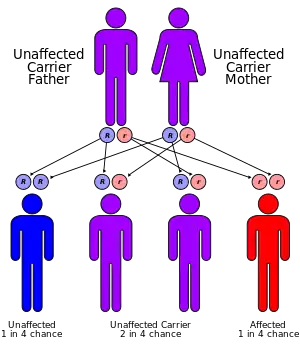
This condition is inherited in an autosomal recessive pattern, which means the defective gene is located on an autosome, and two copies of the gene – one from each parent – are needed to inherit the disorder. The parents of an individual with an autosomal recessive disorder are carriers of one copy of the defective gene, but do not show signs and symptoms of the disorder themselves.
Diagnosis
Glutaric acidemia type 2 often appears in infancy as a sudden metabolic crisis, in which acidosis and low blood sugar (hypoglycemia) cause weakness, behavior changes, and vomiting. There may also be enlargement of the liver, heart failure, and a characteristic odor resembling that of sweaty feet. Some infants with glutaric acidemia type 2 have birth defects, including multiple fluid-filled growths in the kidneys (polycystic kidneys). Glutaric acidemia type 2 is a very rare disorder. Its precise incidence is unknown. It has been reported in several different ethnic groups.
Treatment
It is important for patients with MADD to strictly avoid fasting to prevent hypoglycemia and crises of metabolic acidosis;[6][7] for this reason, infants and small children should eat frequent meals.[7] Patients with MADD can experience life-threatening metabolic crises precipitated by common childhood illnesses or other stresses on the body,[7] so avoidance of such stresses is critical.[6] Patients may be advised to follow a diet low in fat and protein and high in carbohydrates, particularly in severe cases.[6][7] Depending on the subtype, riboflavin[7] (100-400 mg/day),[6] coenzyme Q10 (CoQ10),[6] L-carnitine,[7] or glycine[7] supplements may be used to help restore energy production. Some small, uncontrolled studies[8][9][10] have reported that racemic salts of beta-hydroxybutyrate (one of the ketone bodies) were helpful in patients with moderately severe disease; further research is needed.[6]
See also
- Glutaric acidemia type 1
- Riboflavin-responsive exercise intolerance - similar in biochemical features, also responsive to riboflavin
- Metabolic myopathy
References
- 1 2 "Glutaric acidemia type II". Genetics Home Reference. U.S. Department of Health & Human Services. Retrieved 20 August 2018.
- 1 2 Henriques, Bárbara J.; Katrine Jentoft Olsen, Rikke; Gomes, Cláudio M.; Bross, Peter (2021-04-15). "Electron transfer flavoprotein and its role in mitochondrial energy metabolism in health and disease". Gene. 776: 145407. doi:10.1016/j.gene.2021.145407. ISSN 1879-0038. PMC 7949704. PMID 33450351.
- ↑ "#231680 - MULTIPLE ACYL-CoA DEHYDROGENASE DEFICIENCY; MADD". www.omim.org. Retrieved 2023-12-06.
- ↑ "Glutaric acidemia type II". Genetic and Rare Diseases Information Center. Retrieved 23 February 2023.
- ↑ Béhin, A.; Acquaviva-Bourdain, C.; Souvannanorath, S.; Streichenberger, N.; Attarian, S.; Bassez, G.; Brivet, M.; Fouilhoux, A.; Labarre-Villa, A.; Laquerrière, A.; Pérard, L.; Kaminsky, P.; Pouget, J.; Rigal, O.; Vanhulle, C. (March 2016). "Multiple acyl-CoA dehydrogenase deficiency (MADD) as a cause of late-onset treatable metabolic disease". Revue Neurologique. 172 (3): 231–241. doi:10.1016/j.neurol.2015.11.008. ISSN 0035-3787. PMID 27038534.
- 1 2 3 4 5 6 "Multiple acyl-CoA dehydrogenase deficiency". Orphanet. INSERM and the European Commission. Retrieved 30 August 2018.
- 1 2 3 4 5 6 7 "Glutaric acidemia type II". Genetic and Rare Diseases Information Center (GARD). National Institutes of Health National Center for Advancing Translational Sciences. Retrieved 30 August 2018.
- ↑ Gautschi M, Weisstanner C, Slotboom J, Nava E, Zürcher T, Nuoffer JM (January 2015). "Highly efficient ketone body treatment in multiple acyl-CoA dehydrogenase deficiency-related leukodystrophy". Pediatr Res. 77 (1): 91–8. doi:10.1038/pr.2014.154. PMID 25289702.
- ↑ Van Rijt WJ, Heiner-Fokkema MR, du Marchie Sarvaas GJ, Waterham HR, Blokpoel RG, van Spronsen FJ, Derks TG (October 2014). "Favorable outcome after physiologic dose of sodium-D,L-3-hydroxybutyrate in severe MADD". Pediatrics. 134 (4): e1224-8. doi:10.1542/peds.2013-4254. PMID 25246622. S2CID 16829114. Retrieved 30 August 2018.
- ↑ Van Hove JL, Grünewald S, Jaeken J, Demaerel P, Declercq PE, Bourdoux P, Niezen-Koning K, Deanfeld JE, Leonard JV (26 April 2003). "D,L-3-hydroxybutyrate treatment of multiple acyl-CoA dehydrogenase deficiency (MADD)". The Lancet. 361 (9367): 1433–5. doi:10.1016/S0140-6736(03)13105-4. PMID 12727399. S2CID 25397192.
This article incorporates public domain text from The U.S. National Library of Medicine