 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Qelbree, Vivalan, Emovit, others |
| Other names | ICI-58834; SPN-812; SPN-809 |
| License data |
|
| Routes of administration | By mouth |
| Drug class | Antidepressant; Norepinephrine reuptake inhibitor |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 76–82%[1] |
| Metabolism | Hydroxylation (CYP2D6), glucuronidation (UGT1A9, UGT2B15)[1] |
| Metabolites | 5-Hydroxyviloxazine glucuronide[1] |
| Elimination half-life | IR: 2–5 hours[2] ER: 7.02 ± 4.74 hours[1] |
| Excretion | Urine (~90%), feces (<1%)[1][3] |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| DrugBank |
|
| ChemSpider | |
| UNII |
|
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.051.148 |
| Chemical and physical data | |
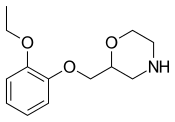
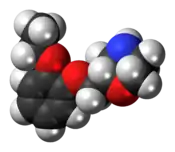
| Formula | C13H19NO3 |
| Molar mass | 237.299 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| | |
Viloxazine, sold under the brand name Qelbree and formerly as Vivalan[5] among others, is a selective norepinephrine reuptake inhibitor medication which is used in the treatment of attention deficit hyperactivity disorder (ADHD) in children and adults.[1][6] It was marketed for almost 30 years as an antidepressant for the treatment of depression before being discontinued and subsequently repurposed as a treatment for ADHD.[7][6][1] Viloxazine is taken orally.[1] It was used as an antidepressant in an immediate-release form and is used in ADHD in an extended-release form.[7][1]
Side effects of viloxazine include insomnia, headache, somnolence, fatigue, nausea, vomiting, decreased appetite, dry mouth, constipation, irritability, increased heart rate, and increased blood pressure.[1] Rarely, the medication may cause suicidal thoughts and behaviors.[1] It can also activate mania or hypomania in people with bipolar disorder.[1] Viloxazine acts as a selective norepinephrine reuptake inhibitor (NRI).[7][1][6] The immediate-release form has an elimination half-life of 2.5 hours[7][2] while the half-life of the extended-release form is 7 hours.[1]
Viloxazine was first described by 1972[8] and was marketed as an antidepressant in Europe in 1974.[7][9] It was not marketed in the United States at this time.[10] The medication was discontinued in 2002 for commercial reasons.[7][11][12] However, it was repurposed for the treatment of ADHD and was reintroduced, in the United States, in April 2021.[7][13][14] Viloxazine is a non-stimulant medication; it has no known misuse liability and is not a controlled substance.[1]
Medical uses
Attention deficit hyperactivity disorder
Viloxazine is indicated to treat attention deficit hyperactivity disorder (ADHD) in children age 6 to 12 years, adolescents age 13 to 17 years, and adults.[1]
Analyses of clinical trial data suggest that viloxazine produces moderate reductions in symptoms; it is about as effective as atomoxetine and methylphenidate but with fewer side effects.[15][16][17][18][19]
Depression
Viloxazine was previously marketed as an antidepressant for the treatment of major depressive disorder.[7][6] It was considered to be effective in mild to moderate as well as severe depression with or without co-morbid symptoms.[7] The typical dose range for depression was 100 to 400 mg per day in divided doses administered generally two to three times per day.[7]
Available forms
Viloxazine is available for ADHD in the form of 100, 150, and 200 mg extended-release capsules.[1] These capsules can be opened and sprinkled into food for easier administration.[1]
Side effects
The most common side effects include drowsiness, headache, loss of appetite. Psychiatric side effects occur in about 20% of cases; the most common of these is irritability (>5%).[20] Other common side effects include nausea, vomiting, epigastric pain, insomnia,[7] and increased libido.[21] Incidence of some side effects, including headache and drowsiness, appear to be dose-dependent.[22] In the treatment of depression, viloxazine is more tolerable than tricyclic antidepressants such as imipramine and amitryptiline.[7]
There were three cases of seizure worldwide, and most animal studies [and clinical trials that included epilepsy patients] indicated the presence of anticonvulsant properties, so viloxazine is not completely contraindicated in patients with epilepsy.[23]
Interactions
Viloxazine increased plasma levels of phenytoin by an average of 37%.[24] It also was known to significantly increase plasma levels of theophylline and decrease its clearance from the body,[25] sometimes resulting in accidental overdose of theophylline.[26]
Pharmacology
Pharmacodynamics
Viloxazine acts as a selective norepinephrine reuptake inhibitor and this is believed to be responsible for its therapeutic effectiveness in the treatment of conditions like ADHD and depression.[7][1][27][28] The affinities (KD) of viloxazine at the human monoamine transporters are 155 to 630 nM for the norepinephrine transporter (NET), 17,300 nM for the serotonin transporter (SERT), and >100,000 nM for the dopamine transporter (DAT).[27][28] Viloxazine has negligible affinity for a variety of assessed receptors, including the serotonin 5-HT1A and 5-HT2A receptors, the dopamine D2 receptor, the α1- and α2-adrenergic receptors, the histamine H1 receptor, and the muscarinic acetylcholine receptors (all >10,000 nM).[29][30]
More recent research has found that the pharmacodynamics of viloxazine may be more complex than previously assumed.[7][28] In 2020, viloxazine was reported to have significant affinity for the serotonin 5-HT2B and 5-HT2C receptors (Ki = 3,900 nM and 6,400 nM) and to act as an antagonist and agonist of these receptors, respectively.[28][6] It also showed weak antagonistic activity at the serotonin 5-HT7 receptor and the α1B- and β2-adrenergic receptors.[28][6] These actions, although relatively weak, might be involved in its effects and possibly its therapeutic effectiveness in the treatment of ADHD.[7][28]
Pharmacokinetics
Absorption
The bioavailability of extended-release viloxazine relative to an instant-release formulation was about 88%.[1] Peak and AUC levels of extended-release viloxazine are proportional over a dosage range of 100 to 400 mg once daily.[1] The time to peak levels is 5 hours with a range of 3 to 9 hours after a single 200 mg dose.[1] A high-fat meal modestly decreases levels of viloxazine and delays the time to peak by about 2 hours.[1] Steady-state levels of viloxazine are reached after 2 days of once-daily administration and no accumulation occurs.[1] Levels of viloxazine are approximately 40 to 50% higher in children age 6 to 11 years compared to children age 12 to 17 years.[1]
Distribution
The plasma protein binding of viloxazine is 76 to 82% over a concentration range of 0.5 to 10 μg/mL.[1]
Metabolism
The metabolism of viloxazine is primarily via the cytochrome P450 enzyme CYP2D6 and the UDP-glucuronosyltransferases UGT1A9 and UGT2B15.[1] The major metabolite of viloxazine is 5-hydroxyviloxazine glucuronide.[1] Viloxazine levels are slightly higher in CYP2D6 poor metabolizers relative to CYP2D6 extensive metabolizers.[1]
Elimination
The elimination of viloxazine is mainly renal.[1] Approximately 90% of the dose is excreted in urine within 24 hours and less than 1% of the dose is recovered in feces.[1]
The elimination half-life of instant-release viloxazine is 2 to 5 hours (2–3 hours in the most reliable studies)[2] and the half-life of extended-release viloxazine is 7.02 ± 4.74 hours.[1]
Chemistry
Viloxazine is a racemic compound with two stereoisomers, the (S)-(–)-isomer being five times as pharmacologically active as the (R)-(+)-isomer.[31]
History
Viloxazine was discovered by scientists at Imperial Chemical Industries when they recognized that some beta blockers inhibited serotonin reuptake inhibitor activity in the brain at high doses. To improve the ability of their compounds to cross the blood brain barrier, they changed the ethanolamine side chain of beta blockers to a morpholine ring, leading to the synthesis of viloxazine.[11]: 610 [32]: 9 It was first described in the scientific literature as early as 1972.[8]
The medication was first marketed in 1974.[7][9] Viloxazine was not approved for medical use by the FDA.[10] In 1984, the FDA granted the medication an orphan designation for treatment of cataplexy and narcolepsy with the tentative brand name Catatrol.[33] For unknown reasons however, it was never approved or introduced for these uses in the United States.[7] Viloxazine was withdrawn from markets worldwide in 2002 for commercial reasons unrelated to efficacy or safety.[7][11][12]
As of 2015, Supernus Pharmaceuticals was developing extended release formulations of viloxazine as a treatment for ADHD and major depressive disorder under the names SPN-809 and SPN-812.[34][35] Viloxazine was approved for the treatment of ADHD in the United States in April 2021.[13][14]
The benefit of viloxazine was evaluated in three clinical studies, including two in children (ages 6 to 11 years) and one in adolescents (ages 12 to 17 years) with ADHD.[36] In each study, pediatric participants were randomly assigned to receive one of two doses of viloxazine or placebo once daily for 6 to 8 weeks.[36] None of the participants, their parent(s)/caregiver(s), the study sponsor, or the study doctors knew which treatment the participant received during the study.[36] The severity of ADHD symptoms observed at the last week of treatment was significantly greater in participants who received placebo compared with participants who received viloxazine.[36] The severity of ADHD symptoms was assessed using the Attention-Deficit Hyperactivity Disorder Rating Scale 5th Edition (ADHD-RS-5).[36] A fourth study provided information about the safety of viloxazine in adolescents 12 to 17 years of age with ADHD.[36] The FDA approved viloxazine based on evidence from several clinical trial(s) of 1289 participants with attention deficit hyperactivity disorder (ADHD).[36] The trials were conducted at 59 sites in the United States.[36]
Research
Viloxazine has undergone two randomized controlled trials for nocturnal enuresis (bedwetting) in children, both of those times versus imipramine.[37][38] By 1990, it was seen as a less cardiotoxic alternative to imipramine, and to be especially effective in heavy sleepers.[39]
In narcolepsy, viloxazine has been shown to suppress auxiliary symptoms such as cataplexy and also abnormal sleep-onset REM[40] without significantly improving daytime somnolence.[41] In a cross-over trial (56 participants) viloxazine significantly reduced EDS and cataplexy.[12]
Viloxazine has also been studied for the treatment of alcoholism, with some success.[42]
Viloxazine did not demonstrate efficacy in a double-blind randomized controlled trial versus amisulpride in the treatment of dysthymia.[43]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 "Qelbree- viloxazine hydrochloride capsule, extended release". DailyMed. Archived from the original on 28 October 2022. Retrieved 3 May 2022.
- 1 2 3 Pinder RM, Brogden RN, Speight TM, Avery GS (June 1977). "Viloxazine: a review of its pharmacological properties and therapeutic efficacy in depressive illness". Drugs. 13 (6): 401–421. doi:10.2165/00003495-197713060-00001. PMID 324751. S2CID 44804763.
- ↑ Case DE, Reeves PR (February 1975). "The disposition and metabolism of I.C.I. 58,834 (viloxazine) in humans". Xenobiotica; the Fate of Foreign Compounds in Biological Systems. 5 (2): 113–129. doi:10.3109/00498257509056097. PMID 1154799.
- ↑ "SID 180462". PubChem Substance Summary. U.S. National Library of Medicine. Archived from the original on 14 June 2013. Retrieved 5 November 2005.
- ↑ Swiss Pharmaceutical Society (2000). Swiss Pharmaceutical Society (ed.). Index Nominum 2000: International Drug Directory. Taylor & Francis. pp. 1093–. ISBN 978-3-88763-075-1. Archived from the original on 2023-01-14. Retrieved 2022-05-03.
- 1 2 3 4 5 6 Cutler AJ, Mattingly GW, Jain R, O'Neal W (April 2022). "Current and future nonstimulants in the treatment of pediatric ADHD: monoamine reuptake inhibitors, receptor modulators, and multimodal agents". CNS Spectrums. 27 (2): 199–207. doi:10.1017/S1092852920001984. PMID 33121553.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Findling RL, Candler SA, Nasser AF, Schwabe S, Yu C, Garcia-Olivares J, et al. (June 2021). "Viloxazine in the Management of CNS Disorders: A Historical Overview and Current Status". CNS Drugs. 35 (6): 643–653. doi:10.1007/s40263-021-00825-w. PMC 8219567. PMID 34003459.
- 1 2 Mallion KB, Todd AH, Turner RW, Bainbridge JG, Greenwood DT, Madinaveitia J, et al. (July 1972). "2-(2-ethoxyphenoxymethyl)tetrahydro-1,4-oxazine hydrochloride, a potential psychotropic agent". Nature. 238 (5360): 157–158. Bibcode:1972Natur.238..157M. doi:10.1038/238157a0. PMID 4558457. S2CID 4268001.
- 1 2 Olivier B, Soudijn W, van Wijngaarden I (2000). "Serotonin, dopamine and norepinephrine transporters in the central nervous system and their inhibitors". Progress in Drug Research. Fortschritte der Arzneimittelforschung. Progres des Recherches Pharmaceutiques. Vol. 54. pp. 59–119. doi:10.1007/978-3-0348-8391-7_3. ISBN 978-3-0348-9546-0. PMID 10857386.
- 1 2 Dahmen MM, Lincoln J, Preskorn S (2010). "NARI Antidepressants". In Stolerman IP (ed.). Encyclopedia of Psychopharmacology. Berlin Heidelberg: Springer-Verlag. pp. 816–822. ISBN 9783540687061.
- 1 2 3 Williams DA (2012). "Chapter 18: Antidepressants.". In Lemke TL, Williams DA (eds.). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. ISBN 9781609133450.
- 1 2 3 Vignatelli L, D'Alessandro R, Candelise L (January 2008). "Antidepressant drugs for narcolepsy". The Cochrane Database of Systematic Reviews. 2008 (1): CD003724. doi:10.1002/14651858.CD003724.pub3. PMC 9030766. PMID 18254030.
- 1 2 "Qelbree: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Archived from the original on 2 April 2021. Retrieved 2 April 2021.
- 1 2 "Supernus Announces FDA Approval of Qelbree (SPN-812) for the Treatment of ADHD". Supernus Pharmaceuticals (Press release). 2 April 2021. Archived from the original on 6 April 2021. Retrieved 3 April 2021.
- ↑ Faraone SV, Gomeni R, Hull JT, Busse GD, Melyan Z, O'Neal W, et al. (February 2021). "Early response to SPN-812 (viloxazine extended-release) can predict efficacy outcome in pediatric subjects with ADHD: a machine learning post-hoc analysis of four randomized clinical trials". Psychiatry Research. 296: 113664. doi:10.1016/j.psychres.2020.113664. PMID 33418457. S2CID 230716405.
- ↑ Hanwella R, Senanayake M, de Silva V (November 2011). "Comparative efficacy and acceptability of methylphenidate and atomoxetine in treatment of attention deficit hyperactivity disorder in children and adolescents: a meta-analysis". BMC Psychiatry. 11: 176. doi:10.1186/1471-244X-11-176. PMC 3229459. PMID 22074258.
- ↑ Rezaei G, Hosseini SA, Akbari Sari A, Olyaeemanesh A, Lotfi MH, Yassini M, et al. (2016-02-10). "Comparative efficacy of methylphenidate and atomoxetine in the treatment of attention deficit hyperactivity disorder in children and adolescents: A systematic review and meta-analysis". Medical Journal of the Islamic Republic of Iran. 30: 325. PMC 4898838. PMID 27390695.
- ↑ Hazell PL, Kohn MR, Dickson R, Walton RJ, Granger RE, Wyk GW (November 2011). "Core ADHD symptom improvement with atomoxetine versus methylphenidate: a direct comparison meta-analysis". Journal of Attention Disorders. 15 (8): 674–683. doi:10.1177/1087054710379737. PMID 20837981. S2CID 43503227.
- ↑ Bushe C, Day K, Reed V, Karlsdotter K, Berggren L, Pitcher A, et al. (May 2016). "A network meta-analysis of atomoxetine and osmotic release oral system methylphenidate in the treatment of attention-deficit/hyperactivity disorder in adult patients". Journal of Psychopharmacology. 30 (5): 444–458. doi:10.1177/0269881116636105. PMID 27005307. S2CID 104938.
- ↑ Pozzi M, Bertella S, Gatti E, Peeters GG, Carnovale C, Zambrano S, Nobile M (December 2020). "Emerging drugs for the treatment of attention-deficit hyperactivity disorder (ADHD)". Expert Opinion on Emerging Drugs. 25 (4): 395–407. doi:10.1080/14728214.2020.1820481. hdl:2434/851076. PMID 32938246. S2CID 221768208.
- ↑ Chebili S, Abaoub A, Mezouane B, Le Goff JF (1998). "[Antidepressants and sexual stimulation: the correlation]" [Antidepressants and sexual stimulation: the correlation]. L'Encephale (in French). 24 (3): 180–184. PMID 9696909.
- ↑ Poznanski AJ, Akinyemi E (September 2022). "Recent Advances in Psychopharmacology". Advances in Psychiatry and Behavioral Health. 2 (1): 253–266. doi:10.1016/j.ypsc.2022.03.009. S2CID 252258910.
- ↑ Edwards JG, Glen-Bott M (September 1984). "Does viloxazine have epileptogenic properties?". Journal of Neurology, Neurosurgery, and Psychiatry. 47 (9): 960–964. doi:10.1136/jnnp.47.9.960. PMC 1027998. PMID 6434699.
- ↑ Pisani F, Fazio A, Artesi C, Russo M, Trio R, Oteri G, et al. (February 1992). "Elevation of plasma phenytoin by viloxazine in epileptic patients: a clinically significant drug interaction". Journal of Neurology, Neurosurgery, and Psychiatry. 55 (2): 126–127. doi:10.1136/jnnp.55.2.126. PMC 488975. PMID 1538217.
- ↑ Perault MC, Griesemann E, Bouquet S, Lavoisy J, Vandel B (September 1989). "A study of the interaction of viloxazine with theophylline". Therapeutic Drug Monitoring. 11 (5): 520–522. doi:10.1097/00007691-198909000-00005. PMID 2815226.
- ↑ Laaban JP, Dupeyron JP, Lafay M, Sofeir M, Rochemaure J, Fabiani P (1986). "Theophylline intoxication following viloxazine induced decrease in clearance". European Journal of Clinical Pharmacology. 30 (3): 351–353. doi:10.1007/BF00541543. PMID 3732375. S2CID 10114046.
- 1 2 Tatsumi M, Groshan K, Blakely RD, Richelson E (December 1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". European Journal of Pharmacology. 340 (2–3): 249–258. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- 1 2 3 4 5 6 Yu C, Garcia-Olivares J, Candler S, Schwabe S, Maletic V (2020). "New Insights into the Mechanism of Action of Viloxazine: Serotonin and Norepinephrine Modulating Properties". Journal of Experimental Pharmacology. 12: 285–300. doi:10.2147/JEP.S256586. PMC 7473988. PMID 32943948.
- ↑ Richelson E, Nelson A (July 1984). "Antagonism by antidepressants of neurotransmitter receptors of normal human brain in vitro". The Journal of Pharmacology and Experimental Therapeutics. 230 (1): 94–102. PMID 6086881.
- ↑ Wander TJ, Nelson A, Okazaki H, Richelson E (December 1986). "Antagonism by antidepressants of serotonin S1 and S2 receptors of normal human brain in vitro". European Journal of Pharmacology. 132 (2–3): 115–121. doi:10.1016/0014-2999(86)90596-0. PMID 3816971.
- ↑ Danchev ND, Rozhanets VV, Zhmurenko LA, Glozman OM, Zagorevskiĭ VA (May 1984). "[Behavioral and radioreceptor analysis of viloxazine stereoisomers]" [Behavioral and radioreceptor analysis of viloxazine stereoisomers]. Biulleten' Eksperimental'noi Biologii I Meditsiny (in Russian). 97 (5): 576–578. PMID 6326891.
- ↑ Wermuth CG (2006). "Chapter 1: Analogs as a Means of Discovering New Drugs.". In Fischer J, Ganellin CR (eds.). Analogue-based Drug Discovery. John Wiley & Sons. ISBN 978352760749-5.
- ↑ "Orphan Drug Designations and Approvals: Viloxazine". U.S. Food and Drug Administration. Archived from the original on 2022-06-25. Retrieved 1 August 2015.
- ↑ "Supernus profile". Bloomberg. Archived from the original on 2018-03-11. Retrieved 1 August 2015.
- ↑ "Psychiatry portfolio". Supernus. Archived from the original on 2016-04-17. Retrieved 1 August 2015.
- 1 2 3 4 5 6 7 8 "Drug Trials Snapshots: Qelbree". U.S. Food and Drug Administration. 13 March 2023. Archived from the original on 14 March 2023. Retrieved 13 March 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ Attenburrow AA, Stanley TV, Holland RP (January 1984). "Nocturnal enuresis: a study". The Practitioner. 228 (1387): 99–102. PMID 6364124.
- ↑ ^ Yurdakök M, Kinik E, Güvenç H, Bedük Y (1987). "Viloxazine versus imipramine in the treatment of enuresis". The Turkish Journal of Pediatrics. 29 (4): 227–230. PMID 3332732.
- ↑ Libert MH (1990). "[The use of viloxazine in the treatment of primary enuresis]" [The use of viloxazine in the treatment of primary enuresis]. Acta Urologica Belgica (in French). 58 (1): 117–122. PMID 2371930.
- ↑ Guilleminault C, Mancuso J, Salva MA, Hayes B, Mitler M, Poirier G, Montplaisir J (1986). "Viloxazine hydrochloride in narcolepsy: a preliminary report". Sleep. 9 (1 Pt 2): 275–279. doi:10.1093/sleep/9.1.275. PMID 3704453.
- ↑ Mitler MM, Hajdukovic R, Erman M, Koziol JA (January 1990). "Narcolepsy". Journal of Clinical Neurophysiology. 7 (1): 93–118. doi:10.1097/00004691-199001000-00008. PMC 2254143. PMID 1968069.
- ↑ Altamura AC, Mauri MC, Girardi T, Panetta B (1990). "Alcoholism and depression: a placebo controlled study with viloxazine". International Journal of Clinical Pharmacology Research. 10 (5): 293–298. PMID 2079386.
- ↑ Mattingly GW, Anderson RH (December 2016). "Optimizing outcomes in ADHD treatment: from clinical targets to novel delivery systems". CNS Spectrums. 21 (S1): 45–59. doi:10.1017/S1092852916000808. PMID 28044946. S2CID 24310209. Archived from the original on 2022-10-13. Retrieved 2019-09-24.
External links
- "Viloxazine". Drug Information Portal. U.S. National Library of Medicine.
- Clinical trial number NCT03247530 for "Evaluation of SPN-812 ER Low Dose in Children With ADHD" at ClinicalTrials.gov
- Clinical trial number NCT03247543 for "Evaluation of SPN-812 ER High Dose in Children With ADHD" at ClinicalTrials.gov