| Seborrhoeic dermatitis | |
|---|---|
| Other names | Sebopsoriasis, seborrhoeic eczema, pityriasis capitis[1] |
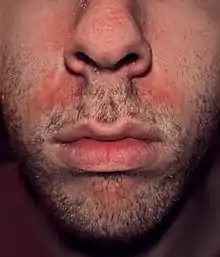 | |
| Seborrhoeic dermatitis of the face | |
| Specialty | Dermatology |
| Symptoms | Flaking, dry or greasy, red, itchy, and inflamed skin[2][3] |
| Duration | Several weeks to lifelong [4] |
| Causes | Multiple factors[4] |
| Risk factors | Stress, dry skin, winter, poor immune function, Parkinson disease[4] |
| Diagnostic method | Based on symptoms[4] |
| Differential diagnosis | Psoriasis, atopic dermatitis, tinea capitis, rosacea, systemic lupus erythematosus[4] |
| Treatment | Humidifier |
| Medication | Antifungal cream, anti-inflammatory agents, coal tar, phototherapy[3] |
| Frequency | ~5% (adults),[4] ~10% (babies)[5] |

Seborrhoeic dermatitis is a long-term skin disorder.[4] Symptoms include flaky, scaly, greasy, and occasionally itchy and inflamed skin.[2][3] Areas of the skin rich in oil-producing glands are often affected including the scalp, face, and chest.[4] It can result in social or self-esteem problems.[4] In babies, when the scalp is primarily involved, it is called cradle cap.[2] Seborrhoeic dermatitis of the scalp may be described in lay terms as dandruff due to the dry, flaky character of the skin.[6] However, as dandruff may refer to any dryness or scaling of the scalp, not all dandruff is seborrhoeic dermatitis.[6] Seborrhoeic dermatitis is sometimes inaccurately referred to as seborrhoea.[4]
The cause is unclear but believed to involve a number of genetic and environmental factors.[2][4] Risk factors for seborrhoeic dermatitis include poor immune function, Parkinson's disease, and alcoholic pancreatitis.[4][6] The condition may worsen with stress or during the winter.[4] Malassezia yeast is believed to play a role.[6] It is not a result of poor hygiene.[7] Diagnosis is typically clinical and based on the symptoms present.[4][8] The condition is not contagious.[9]
The typical treatment is topical antifungal cream and anti-inflammatory agents.[3] Specifically, ketoconazole or ciclopirox are effective.[10] Seborrhoeic dermatitis of the scalp is often treated with shampoo preparations of ketoconazole or zinc pyrithione.[11]
The condition is common in infants within the first three months of age or in adults aged 30 to 70 years.[2][4][5] It tends to affect more males.[12] Seborrhoeic dermatitis is more common in African Americans, among individuals who are immune compromised, such as with HIV, and individuals with Parkinson's disease.[11][12]
Signs and symptoms

Seborrhoeic dermatitis typically appears as dry, white, flaky skin. The flakes can be fine, loose, and diffuse or thick and adherent.[11][8] Additionally, flakes can appear yellow and oily or greasy.[8][12] In addition to flaky skin, seborrhoeic dermatitis can have areas of red, inflamed, and itchy skin that coincide with the area of skin flaking, but not all individuals have this symptom.[8] seborrhoeic dermatitis of the scalp can appear similarly to dandruff.[11] When the scalp is affected, there can be associated temporary hair loss.[11] Such hair loss varies in appearance from diffuse thinning to patchy areas of hair loss.[11] On close inspection, the locations where hair has thinned may have broken stubs of hair and pustules around the hair follicles.[11] Individuals with more pigmented skin tones may experience increased or decreased skin pigmentation in affected areas.[12]
Various locations can be affected by seborrhoeic dermatitis. Commonly affected areas include the face, ears, scalp, and across the body. It is less common in intertriginous areas, which are areas where the skin folds and comes into contact with itself, such as the groin or underarm.[11]
Seborrhoeic dermatitis' symptoms are typically mild and appear gradually but are often persistent, lasting weeks to years.[8][11][13] Individuals with seborrhoeic dermatitis are subject to recurrent bouts and it may be a lifelong condition.[8] Seborrhoeic dermatitis can also occur quickly and severely in patients with Human Immunodeficiency Virus (HIV). In fact, this is sometimes the first indication of HIV.[12]
Causes
The cause of seborrhoeic dermatitis has not been fully clarified.[1][14]
In addition to the presence of Malassezia, genetic, environmental, hormonal, and immune-system factors are necessary for and/or modulate the expression of seborrhoeic dermatitis.[15][16] The condition may be aggravated by illness, psychological stress, fatigue, sleep deprivation, change of season, and reduced general health.[17]
Fungi
The condition is thought to be due to a local inflammatory response to overgrowth by Malassezia fungi species in sebum-producing skin areas including the scalp, face, chest, back, underarms, and groin.[3][14] This is based on observations of high counts of Malassezia species in skin affected by seborrhoeic dermatitis and on the effectiveness of antifungals in treating the condition.[14] Species of Malassezia implicated in Seborrhoeic dermatitis include M. furfur (formerly Pityrosporum ovale), M. globosa, M. restricta, M. sympodialis, and M. slooffiae.[3] Malassezia appears to be the significant factor in seborrhoeic dermatitis but it is thought that other factors are necessary for the presence of Malassezia to result in the seborrhoeic dermatitis.[14] For example, summer growth of Malassezia in the skin alone does not result in seborrhoeic dermatitis.[14] Besides antifungals, the effectiveness of anti-inflammatory drugs, which reduce inflammation, and antiandrogens, which reduce sebum production, provide further insights into the pathophysiology of seborrhoeic dermatitis.[3][18][19]
Bacteria
Several bacteria, including Propionibacterium species and Staphylococcus aureus, have been shown to have some level of interaction with seborrhoeic dermatitis, though their exact impact is not known.[20][12]
Nutrition
Seborrhoeic dermatitis-like eruptions are also associated with pyridoxine (vitamin B6) and riboflavin (vitamin B2) deficiency.[21][8] In children and babies, issues with Δ6-desaturase enzymes[17] have been correlated with increased risk.
Immune dysfunction
Those with immunodeficiency (especially infection with HIV) and with neurological disorders that may impact immune system function such as Parkinson's disease (for which the condition is an autonomic sign) and stroke are particularly prone to it.[22]
Climate
Climate can affect seborrheic dermatitis, but there is a lack of consensus about which climates tend to exacerbate seborrheic dermatitis the most. Some studies show low humidity and low temperature are responsible for high frequency of seborrheic dermatitis.[23] Others suggest hot environments may also worsen seborrhoeic dermatitis.[12] Yet another described that high humidity and low UV exposure are culpable.[24] Dry skin and an impaired skin barrier contribute to the condition.[12][20] It is likely that climate and weather variations affect the water and lipid content of skin.[20]
Mechanism
Seborrhoeic dermatitis is a complex condition with many interacting factors that are not yet fully explained.[14] In general, the major factors that influence the development and severity include Malassezia yeast presents on and in the skin, skin production of oily sebum, and a subsequent inflammatory response against Malassezia and their byproducts.[12] Additional factors involved in the condition are a compromised skin barrier, the makeup and amount of sebum produced, the character of the immune response and inflammation, and the presence of other microbes species inhabiting the skin.[14][12] A suggested series of events leading to seborrhoeic dermatitis are initial damaged skin barrier and abnormal sebum production which leads to a change in the microbiome of the skin that in turn elicits an immune response.[14] An alternative explanation is an increase in sebum production feeding an increase in the Malassezia population that instigates inflammation; the inflammation then causes cellular changes that damage the skin barrier. This barrier disruption then encourages additional Malassezia growth and inflammation and again worsened skin barrier function.[12]
Diagnosis
Typically, seborrhoeic dermatitis is a clinical diagnosis based off a physician's expertise in identifying and differentiating skin conditions based on the history of the individual and the appearance of the skin.[8] However, seborrhoeic dermatitis may also be diagnosed with additional testing. The least invasive test is a visual inspection in the clinic using a Wood's Lamp.[11] A KOH test can also be used, where skin scraping of the affected skin may also be taken and prepared with potassium hydroxide (KOH) and visualized under a microscope to look for Malassezia or other microbiological cell. Additionally, a fungal culture of the affected skin may be taken to attempt to grow and identify the causative organism.[11]
Differential diagnosis
Seborrhoeic dermatitis can look similar to other skin conditions that share its characteristic dry, flaky, scaly, and inflamed appearance but have different causes and treatments. Physicians use the history of the individual with the skin condition as well as other tests to identify which disorder is present. Other conditions that may be confused with seborrhoeic dermatitis based on appearance are listed below.[8][11]
Management
Medications
A variety of different types of medications are able to reduce symptoms of seborrhoeic dermatitis.[3] These include certain antifungals, anti-inflammatory agents like corticosteroids and nonsteroidal anti-inflammatory drugs, antiandrogens, and antihistamines, among others.[3][1] Treatments must take into consideration potential side effects, especially with long-term use given the chronic nature of seborrhoeic dermatitis. Initial therapy is usually a topical preparation with an agreeable side effect profile.[12]
Antifungals
Regular use of an over-the-counter or prescription antifungal shampoo or cream is a common treatment. The topical antifungal medications ketoconazole and ciclopirox have the best evidence.[10] Ketoconazole should be used twice per week.[8] Shampoo or soap containing zinc pyrithione or selenium sulfide is also used.[8] These options should be used on a daily basis but may also be used in conjunction with a ketoconazole shampoo regimen on alternate days.[8] It is unclear if other antifungals are equally effective as this has not been sufficiently studied.[10] Antifungals that have been studied and found to be effective in the treatment of seborrhoeic dermatitis include ketoconazole, fluconazole, miconazole, bifonazole, sertaconazole, clotrimazole, flutrimazole, ciclopirox, terbinafine, butenafine, selenium disulfide, and lithium salts such as lithium gluconate and lithium succinate.[10][3] Topical climbazole appears to have little effectiveness in the treatment of seborrhoeic dermatitis.[10] Systemic therapy with oral antifungals including itraconazole, fluconazole, ketoconazole is effective, but adverse side effects have been documented for fluconazole and ketoconazole, with the latter not recommended for use, while itraconazole, with its good safety profile, is the most commonly prescribed.[3] Terbinafine is said to be effective, but with adverse side effects, while other sources state it is not effective and should not be used.[3][11]
Anti-inflammatory treatments
Topical corticosteroids have been shown to be effective in short-term treatment of seborrhoeic dermatitis. They cannot be used long term or for maintenance because of their skin-thinning side effect. Accordingly, these are used for only a few weeks at a time.[11] There is also evidence for the effectiveness of topical calcineurin inhibitors like tacrolimus and pimecrolimus as well as lithium salt therapy.[25] Calcineurin inhibitors were also effective in reducing growth of Malassezia, offering two routes by which they may treat seborrhoeic dermatitis.[24] Medications such as the calcineurin inhibitors should not be used in individuals with seborrhoeic dermatitis who are immune compromised because they cause further immune suppression.[11]
Oral immunosuppressive treatment, such as with prednisone, has been used in short courses for seborrhoeic dermatitis, as a last resort due to its potential side effects.[26]
Antiandrogens
Seborrhoea, which is sometimes associated with seborrhoeic dermatitis,[27][28][29] is recognized as an androgen-sensitive condition – that is, it is caused or aggravated by androgen sex hormones such as testosterone and dihydrotestosterone – and is a common symptom of hyperandrogenism (e.g., that seen in polycystic ovary syndrome).[30][31] In addition, seborrhoeic dermatitis, as well as acne, are commonly associated with puberty due to the steep increase of androgen levels at that time.[32] Males have increased activity of sebacious glands and are more likely to have seborrhoeic dermatitis.[20] Skin with increased sebacious glands is also more likely to be affected.[20]
In accordance with the involvement of androgens in seborrhoeic dermatitis, antiandrogens, such as cyproterone acetate,[33] spironolactone,[34] flutamide,[35][36] and nilutamide,[37][38] are highly effective in alleviating the condition.[30][39] As such, they are used in the treatment of seborrhoeic dermatitis,[30][39] particularly severe cases.[40] While beneficial in seborrhoeic dermatitis, effectiveness may vary with different antiandrogens; for instance, spironolactone (which is regarded as a relatively weak antiandrogen) has been found to produce a 50% improvement after three months of treatment, whereas flutamide has been found to result in an 80% improvement within three months.[30][36] Cyproterone acetate, similarly more potent and effective than spironolactone, results in considerable improvement or disappearance of acne and seborrhoea in 90% of patients within three months.[41]
Systemic antiandrogen therapy is generally used to treat seborrhoeic dermatitis only in women, not in men, as these medications can result in feminization (e.g., gynecomastia), sexual dysfunction, and infertility in males.[42][43] In addition, antiandrogens theoretically have the potential to feminize male fetuses in pregnant women and, for this reason, are usually combined with effective birth control in sexually active women who can or may become pregnant.[41]
Antihistamines
Antihistamines are used primarily to reduce itching, if present. However, research studies suggest that some antihistamines have anti-inflammatory properties.[44]
Keratolytics
Keratolytics help the skin via exfoliation built-up skin flakes and thereby remove scale. They are applied topically to the affected area. Keratolytics include urea, salicylic acid, coal tar, lactic acid, pyrithione zinc and propylene glycol.[24] Coal tar shampoo formulations can be effective.[8][24] Although no significant increased risk of cancer in human treatment with coal tar shampoos has been found, caution is advised since coal tar is carcinogenic in animals, and heavy human occupational exposures do increase cancer risks.[45]
Other treatments
- Isotretinoin, a sebosuppressive agent, may be used to reduce sebaceous gland activity as a last resort in refractory disease.[29] However, isotretinoin has potentially serious side effects, and few patients with seborrhoeic dermatitis are appropriate candidates for therapy.[26]
- Topical 0.75% and 1% Metronidazole[10][11]
- Topical 4% nicotinamide[3]
- Topical sulfacetamide[11]
- Tea tree oil [12]
- Cannabidiol shampoo [24]
- Frequent washing to avoid the build-up of scale, especially on the scalp, but while avoiding overly drying the skin[12][11][20]
- Avoiding damaging skin with harsh grooming or chemical irritants[20]
Phototherapy
Another option is natural and artificial UV radiation since it can inhibit the growth of Malassezia yeast.[46] Some recommend photodynamic therapy using UV-A and UV-B laser or red and blue LED light to inhibit the growth of Malassezia fungus and reduce seborrhoeic inflammation.[46][47][48]
Outcome
Seborrhoeic dermatitis is generally a chronic and recurring condition. Individuals may have the condition for several weeks to months, but it may also last years or their lifetime. There may be periods of relapse and worsening.[11][8]
Epidemiology
Seborrhoeic dermatitis affects 1 to 5% of the general population.[1][49][50] It is slightly more common in men, but affected women tend to have more severe symptoms.[50] The condition usually recurs throughout a person's lifetime.[51] Seborrhoeic dermatitis can occur in any age group[51] but often occurs during the first three months of life then again at puberty and peaks in incidence at around 40 years of age.[52][20] It can reportedly affect as many as 31% of older people.[50] Infants may also have this condition, though it is typically milder, and is referred to as cradle cap.[12] Seborrhoeic dermatitis is more common in African-Americans.[12]
Severity is worse in dry climates[51] as well as hot weather as dry skin can exacerbate the condition.[12] COVID-19 related mask usage may also cause or exacerbate facial seborrhoeic dermatitis.[12]
Individuals who are immune compromised have increased risk of seborrhoeic dermatitis.[12] Conditions that are associated with increased rates of seborrhoeic dermatitis include individuals with HIV, hepatitis C, alcoholic pancreatitis, Parkinson's disease, and alcohol abuse.[12] Seborrhoeic dermatitis is common in people with alcoholism, between 7 and 11 percent, which is twice the normal expected occurrence.[53]
References
- 1 2 3 4 Dessinioti C, Katsambas A (Jul–Aug 2013). "Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies". Clinics in Dermatology. 31 (4): 343–351. doi:10.1016/j.clindermatol.2013.01.001. PMID 23806151.
- 1 2 3 4 5 "Seborrheic Dermatitis - Dermatologic Disorders". Merck Manuals Professional Edition. Retrieved 22 November 2019.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Borda LJ, Perper M, Keri JE (March 2019). "Treatment of seborrheic dermatitis: a comprehensive review". The Journal of Dermatological Treatment. 30 (2): 158–169. doi:10.1080/09546634.2018.1473554. PMID 29737895. S2CID 13686180.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Ijaz N, Fitzgerald D (June 2017). "Seborrhoeic dermatitis". British Journal of Hospital Medicine. 78 (6): C88–C91. doi:10.12968/hmed.2017.78.6.C88. PMID 28614013.
- 1 2 Nobles T, Harberger S, Krishnamurthy K (August 2021). "Cradle Cap". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 30285358.
- 1 2 3 4 Naldi L, Diphoorn J (May 2015). "Seborrhoeic dermatitis of the scalp". BMJ Clinical Evidence. 2015. PMC 4445675. PMID 26016669.
- ↑ "Seborrheic dermatitis". American Academy of Dermatology. Archived from the original on 21 October 2017. Retrieved 20 October 2017.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Papadakis MA, McPhee SJ (2023). "Dermatitis, Seborrheic". Quick Medical Diagnosis & Treatment 2023 (2023 ed.). McGraw-Hill Education. ISBN 978-1264687343.
- ↑ "Seborrheic Dermatitis: What is It, Diagnosis & Treatment". Cleveland, Ohio: Cleveland Clinic.
- 1 2 3 4 5 6 Okokon EO, Verbeek JH, Ruotsalainen JH, Ojo OA, Bakhoya VN (May 2015). Okokon EO (ed.). "Topical antifungals for seborrhoeic dermatitis". The Cochrane Database of Systematic Reviews. 4 (5): CD008138. doi:10.1002/14651858.CD008138.pub3. PMC 4448221. PMID 25933684.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Dinulos JG (2021). Habif's Clinical Dermatology, Seventh Edition (7th ed.). Elsevier Inc. ISBN 978-0-323-61269-2.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 Jackson JM, Alexis A, Zirwas M, Taylor S (December 2022). "Unmet needs for patients with seborrheic dermatitis". Journal of the American Academy of Dermatology: S0190–9622(22)03307–2. doi:10.1016/j.jaad.2022.12.017. PMID 36538948. S2CID 254843412.
- ↑ "Dermatitis". Archived from the original on September 25, 2011. Retrieved June 11, 2010.
- 1 2 3 4 5 6 7 8 Wikramanayake TC, Borda LJ, Miteva M, Paus R (September 2019). "Seborrheic dermatitis-Looking beyond Malassezia". Experimental Dermatology. 28 (9): 991–1001. doi:10.1111/exd.14006. PMID 31310695.
- ↑ Johnson BA, Nunley JR (May 2000). "Treatment of seborrheic dermatitis". American Family Physician. 61 (9): 2703–10, 2713–4. PMID 10821151. Archived from the original on 2010-07-06.
- ↑ Janniger CK, Schwartz RA (July 1995). "Seborrheic dermatitis". American Family Physician. 52 (1): 149–55, 159–60. PMID 7604759.
- 1 2 Schwartz RA, Janusz CA, Janniger CK (July 2006). "Seborrheic dermatitis: an overview". American Family Physician. 74 (1): 125–130. PMID 16848386. Archived from the original on 2020-01-26. Retrieved 2010-04-15.
- ↑ Trivedi MK, Shinkai K, Murase JE (March 2017). "A Review of hormone-based therapies to treat adult acne vulgaris in women". International Journal of Women's Dermatology. 3 (1): 44–52. doi:10.1016/j.ijwd.2017.02.018. PMC 5419026. PMID 28492054.
- ↑ Paradisi R, Fabbri R, Porcu E, Battaglia C, Seracchioli R, Venturoli S (October 2011). "Retrospective, observational study on the effects and tolerability of flutamide in a large population of patients with acne and seborrhea over a 15-year period". Gynecological Endocrinology. 27 (10): 823–829. doi:10.3109/09513590.2010.526664. PMID 21117864. S2CID 20250916.
- 1 2 3 4 5 6 7 8 Mangion SE, Mackenzie L, Roberts MS, Holmes AM (April 2023). "Seborrheic dermatitis: topical therapeutics and formulation design". European Journal of Pharmaceutics and Biopharmaceutics. 185: 148–164. doi:10.1016/j.ejpb.2023.01.023. PMID 36842718. S2CID 257214910.
- ↑ Alamgir AN (2018). Therapeutic Use of Medicinal Plants and their Extracts: Volume 2: Phytochemistry and Bioactive Compounds. Springer. p. 435. ISBN 978-3319923871.
- ↑ "Seborrhoeic dermatitis and dandruff (seborrheic eczema). DermNet NZ". . DermNet NZ. 2012-03-20. Archived from the original on 2012-06-15. Retrieved 2012-06-10.
- ↑ Araya M, Kulthanan K, Jiamton S (September 2015). "Clinical Characteristics and Quality of Life of Seborrheic Dermatitis Patients in a Tropical Country". Indian Journal of Dermatology. 60 (5): 519. doi:10.4103/0019-5154.164410. PMC 4601435. PMID 26538714.
- 1 2 3 4 5 Leroy AK, Cortez de Almeida RF, Obadia DL, Frattini S, Melo DF (June 2023). "Scalp Seborrheic Dermatitis: What We Know So Far". Skin Appendage Disorders. 9 (3): 160–164. doi:10.1159/000529854. PMC 10264915. PMID 37325288.
- ↑ Kastarinen H, Oksanen T, Okokon EO, Kiviniemi VV, Airola K, Jyrkkä J, et al. (May 2014). "Topical anti-inflammatory agents for seborrhoeic dermatitis of the face or scalp". The Cochrane Database of Systematic Reviews. 2017 (5): CD009446. doi:10.1002/14651858.CD009446.pub2. PMC 6483543. PMID 24838779.
- 1 2 Gupta AK, Richardson M, Paquet M (January 2014). "Systematic review of oral treatments for seborrheic dermatitis". Journal of the European Academy of Dermatology and Venereology. 28 (1): 16–26. doi:10.1111/jdv.12197. PMID 23802806. S2CID 25441626.
- ↑ "Seborrhoeic dermatitis | DermNet NZ". dermnetnz.org. Retrieved 2021-09-20.
- ↑ Burton JL, Pye RJ (April 1983). "Seborrhoea is not a feature of seborrhoeic dermatitis". British Medical Journal. 286 (6372): 1169–1170. doi:10.1136/bmj.286.6372.1169. PMC 1547390. PMID 6220754.
- 1 2 de Souza Leão Kamamoto C, Sanudo A, Hassun KM, Bagatin E (January 2017). "Low-dose oral isotretinoin for moderate to severe seborrhea and seborrheic dermatitis: a randomized comparative trial". International Journal of Dermatology. 56 (1): 80–85. doi:10.1111/ijd.13408. PMID 27778328. S2CID 13049459.
- 1 2 3 4 Singh SM, Gauthier S, Labrie F (February 2000). "Androgen receptor antagonists (antiandrogens): structure-activity relationships". Current Medicinal Chemistry. 7 (2): 211–247. doi:10.2174/0929867003375371. PMID 10637363.
- ↑ Zouboulis CC, Degitz K (2004). "Androgen action on human skin -- from basic research to clinical significance". Experimental Dermatology. 13 (s4): 5–10. doi:10.1111/j.1600-0625.2004.00255.x. PMID 15507105. S2CID 34863608.
- ↑ Handelsman DJ (October 2020). "Androgen Physiology, Pharmacology, Use and Misuse". In Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, et al. (eds.). Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc. PMID 25905231.
- ↑ Becker KL (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 1004–. ISBN 978-0-7817-1750-2. Archived from the original on 2013-06-02.
- ↑ Plewig G, Kligman AM (6 December 2012). ACNE and ROSACEA. Springer Science & Business Media. pp. 66, 685, 687. ISBN 978-3-642-59715-2. Archived from the original on 19 March 2017.
- ↑ Farid NR, Diamanti-Kandarakis E (27 February 2009). Diagnosis and Management of Polycystic Ovary Syndrome. Springer Science & Business Media. pp. 240–. ISBN 978-0-387-09718-3. Archived from the original on 19 March 2017.
- 1 2 Diamanti-Kandarakis E (September 1999). "Current aspects of antiandrogen therapy in women". Current Pharmaceutical Design. 5 (9): 707–23 (717). doi:10.2174/1381612805666230111201150. PMID 10495361.
- ↑ Couzinet B, Thomas G, Thalabard JC, Brailly S, Schaison G (July 1989). "Effects of a pure antiandrogen on gonadotropin secretion in normal women and in polycystic ovarian disease". Fertility and Sterility. 52 (1): 42–50. doi:10.1016/s0015-0282(16)60786-0. PMID 2744186.
- ↑ Namer M (October 1988). "Clinical applications of antiandrogens". Journal of Steroid Biochemistry. 31 (4B): 719–729. doi:10.1016/0022-4731(88)90023-4. PMID 2462132.
- 1 2 Mutschler HD (1995). Drug Actions: Basic Principles and Therapeutic Aspects. CRC Press. pp. 304–. ISBN 978-0-8493-7774-7. Archived from the original on 2017-11-05.
- ↑ DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM (6 July 2008). Pharmacotherapy: A Pathophysiologic Approach. McGraw Hill Professional. p. 1598. ISBN 978-0-07-164325-2. Archived from the original on 19 March 2017.
- 1 2 Hughes A, Hasan SH, Oertel GW, Voss HE, Bahner F, Neumann F, et al. (27 November 2013). Androgens II and Antiandrogens / Androgene II und Antiandrogene. Springer Science & Business Media. pp. 351, 516. ISBN 978-3-642-80859-3. Archived from the original on 19 March 2017.
- ↑ Millikan LE (19 April 2016). Drug Therapy in Dermatology. CRC Press. pp. 295–. ISBN 978-0-203-90831-0. Archived from the original on 29 July 2017.
- ↑ Brenner S (13 December 2013). The Clinical Nanomedicine Handbook. CRC Press. pp. 97–. ISBN 978-1-4398-3478-7. Archived from the original on 5 November 2017.
- ↑ Grob JJ, Castelain M, Richard MA, Bonniol JP, Béraud V, Adhoute H, et al. (May 1998). "Antiinflammatory properties of cetirizine in a human contact dermatitis model. Clinical evaluation of patch tests is not hampered by antihistamines". Acta Dermato-Venereologica. 78 (3): 194–197. doi:10.1080/000155598441512. PMID 9602225.
- ↑ Roelofzen JH, Aben KK, Oldenhof UT, Coenraads PJ, Alkemade HA, van de Kerkhof PC, et al. (April 2010). "No increased risk of cancer after coal tar treatment in patients with psoriasis or eczema". The Journal of Investigative Dermatology. 130 (4): 953–961. doi:10.1038/jid.2009.389. PMID 20016499.
- 1 2 Wikler JR, Janssen N, Bruynzeel DP, Nieboer C (1990). "The effect of UV-light on pityrosporum yeasts: ultrastructural changes and inhibition of growth". Acta Dermato-Venereologica. 70 (1): 69–71. PMID 1967880.
- ↑ Calzavara-Pinton PG, Venturini M, Sala R (January 2005). "A comprehensive overview of photodynamic therapy in the treatment of superficial fungal infections of the skin". Journal of Photochemistry and Photobiology. B, Biology. 78 (1): 1–6. doi:10.1016/j.jphotobiol.2004.06.006. PMID 15629243.
- ↑ Maisch T, Szeimies RM, Jori G, Abels C (October 2004). "Antibacterial photodynamic therapy in dermatology". Photochemical & Photobiological Sciences. rsc.org. 3 (10): 907–917. doi:10.1039/B407622B. PMID 15480480. S2CID 32215045.
- ↑ Goldstein MA, Goldstein MC, Credit LP (17 March 2009). Your Best Medicine: From Conventional and Complementary Medicine--Expert-Endorsed Therapeutic Solutions to Relieve Symptoms and Speed Healing. Rodale. pp. 462–. ISBN 978-1-60529-656-2. Archived from the original on 5 November 2017.
- 1 2 3 Farage MA, Miller KW, Maibach HI (2 December 2009). Textbook of Aging Skin. Springer Science & Business Media. pp. 534–. ISBN 978-3-540-89655-5. Archived from the original on 5 November 2017.
- 1 2 3 Jacknin J (2001). Smart Medicine for Your Skin: A Comprehensive Guide to Understanding Conventional and Alternative Therapies to Heal Common Skin Problems. Penguin. pp. 271–. ISBN 978-1-58333-098-2. Archived from the original on 2017-11-05.
- ↑ Ooi ET, Tidman MJ (February 2014). "Improving the management of seborrhoeic dermatitis". The Practitioner. 258 (1768): 23–6, 3. PMID 24689165.
- ↑ Kostović K, Lipozencić J (2004). "Skin diseases in alcoholics". Acta Dermatovenerologica Croatica. 12 (3): 181–190. PMID 15369644.
External links
![]() Media related to Seborrhoeic dermatitis at Wikimedia Commons
Media related to Seborrhoeic dermatitis at Wikimedia Commons