Prostaglandin E2 receptor 1 (EP1) is a 42kDa prostaglandin receptor encoded by the PTGER1 gene. EP1 is one of four identified EP receptors, EP1, EP2, EP3, and EP4 which bind with and mediate cellular responses principally to prostaglandin E2) (PGE2) and also but generally with lesser affinity and responsiveness to certain other prostanoids (see Prostaglandin receptors).[5] Animal model studies have implicated EP1 in various physiological and pathological responses. However, key differences in the distribution of EP1 between these test animals and humans as well as other complicating issues make it difficult to establish the function(s) of this receptor in human health and disease.[6]
Gene
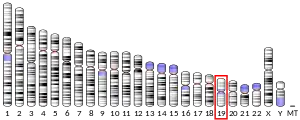
The PTGER1 gene is located on human chromosome 19 at position p13.12 (i.e. 19p13.12), contains 2 introns and 3 exons, and codes for a G protein-coupled receptor (GPCR) of the rhodopsin-like receptor family, Subfamily A14 (see rhodopsin-like receptors#Subfamily A14).[7]
Expression
Studies in mice, rats, and guinea pigs have found EP1 Messenger RNA and protein to be expressed in the papillary collecting ducts of the kidney, in the kidney, lung, stomach, thalamus, and in the dorsal root ganglia neurons as well as several central nervous system sites.[8] However, the expression of EP1 In humans, its expression appears to be more limited: EP1 receptors have been detected in human mast cells, pulmonary veins, keratinocytes, myometrium, and colon smooth muscle.[6][9]
Ligands
Activating ligands
The following standard prostaglandins have the following relative potencies in binding to and activating EP1: PGE2≥PGE1>PGF2alpha>PGD2. The receptor binding affinity Dissociation constant Kd (i.e. ligand concentration needed to bind with 50% of available EP1 receptors) is ~20 nM and that of PGE1 ~40 for the mouse receptor and ~25 nM for PGE2 with the human receptor.[9][10]
Because PGE2 activates multiple prostanoid receptors and has a short half-life in vivo due to its rapidly metabolism in cells by omega oxidation and beta oxidation], metabolically resistant EP1-selective activators are useful for the study of EP1's function and could be clinically useful for the treatment of certain diseases. Only one such agonist that is highly selective in stimulating EP1 has been synthesized and identified, ONO-D1-OO4. This compound has a Ki inhibitory binding value (see Biochemistry#Receptor/ligand binding affinity) of 150 nM compared to that of 25 nM for PGE2 and is therefore ~5 times weaker than PGE2.[9]
Inhibiting ligands
SC51322 (Ki=13.8 nM), GW-848687 (Ki=8.6 nM), ONO-8711, SC-19220, SC-51089, and several other synthetic compounds given in next cited reference are selective competitive antagonists for EP1 that have been used for studies in animal models of human diseases. Carbacylin, 17-phenyltrinor PGE1, and several other tested compounds are dual EP1/EP3 antagonists (most marketed prostanoid receptor antagonists exhibit poor receptor selectivity).[9]
Mechanism of cell activation
When initially bound to PGE2 or other stimulating ligand, EP1 mobilizes G proteins containing the Gq alpha subunit (Gαq/11)-G beta-gamma complex. These two subunits in turn stimulate the Phosphoinositide 3-kinase pathway that raises cellular cytosolic Ca2+ levels thereby regulating Ca2+-sensitive cell signal pathways which include, among several others, those that promote the activation of certain protein kinase C isoforms.[6] Since, this rise in cytosolic Ca2+ can also contract muscle cells, EP1 has been classified as a contractile type of prostanoid receptor. The activation of protein kinases C feeds back to phosphorylate and thereby desensitizes the activated EP1 receptor (see homologous desensitization but may also desensitize other types of prostanoid and non-prostanoid receptors (see heterologous desensitization). These desensitizations limit further EP1 receptor activation within the cell.[6][10][11] Concurrently with the mobilization of these pathways, ligand-activated EP1 stimulates ERK, p38 mitogen-activated protein kinases, and CREB pathways that lead to cellular functional responses.[12]
Function
Studies using animals genetically engineered to lack EP1 and supplemented by studies using treatment with EP1 receptor antagonists and agonists indicate that this receptor serves several functions. 1) It mediates hyperalgesia due to EP11 receptors located in the central nervous system but suppresses pain perception due to E1 located on dorsal root ganglia neurons in rats. Thus, PGE2 causes increased pain perception when administered into the central nervous system but inhibits pain perception when administered systemically; 2) It promotes colon cancer development in Azoxymethane-induced and APC gene knockout mice. 3) It promotes hypertension in diabetic mice and spontaneously hypertensive rats. 4) It suppresses stress-induced impulsive behavior and social dysfunction in mice by suppressing the activation of Dopamine receptor D1 and Dopamine receptor D2 signaling. 5) It enhances the differentiation of uncommitted T cell lymphocytes to the Th1 cell phenotype and may thereby favor the development of inflammatory rather than allergic responses to immune stimulation in rodents. Studies with human cells indicate that EP1 serves a similar function on T cells. 6) It may reduce expression of Sodium-glucose transport proteins in the apical membrane or cells of the intestinal mucosa in rodents.[6][12][13][14] 7) It may be differentially involved in etiology of acute brain injuries. Pharmacological inhibition or genetic deletion of EP1 receptor produce either beneficial or deleterious effects in rodent models of neurological disorders such as ischemic stroke,[15] epileptic seizure,[16] surgically induced brain injury[17] and traumatic brain injury.[18]
Clinical studies
EP1 receptor antagonists have been studied clinically primarily to treat hyperalgesia. Numerous EP antagonists have been developed including SC51332, GW-848687X, a benzofuran-containing drug that have had some efficacy in treating various hyperalgesic syndromes in animal models. None have as yet been reported to be useful in humans.[9]
See also
References
- 1 2 3 GRCh38: Ensembl release 89: ENSG00000160951 - Ensembl, May 2017
- 1 2 3 GRCm38: Ensembl release 89: ENSMUSG00000019464 - Ensembl, May 2017
- ↑ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ↑ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ↑ "Entrez Gene: PTGER1 prostaglandin E receptor 1 (subtype EP1), 42kDa".
- 1 2 3 4 5 Woodward DF, Jones RL, Narumiya S (September 2011). "International Union of Basic and Clinical Pharmacology. LXXXIII: classification of prostanoid receptors, updating 15 years of progress". Pharmacological Reviews. 63 (3): 471–538. doi:10.1124/pr.110.003517. PMID 21752876.
- ↑ "PTGER1 prostaglandin E receptor 1 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov.
- ↑ Ricciotti E, FitzGerald GA (May 2011). "Prostaglandins and inflammation". Arteriosclerosis, Thrombosis, and Vascular Biology. 31 (5): 986–1000. doi:10.1161/ATVBAHA.110.207449. PMC 3081099. PMID 21508345.
- 1 2 3 4 5 Markovič T, Jakopin Ž, Dolenc MS, Mlinarič-Raščan I (January 2017). "Structural features of subtype-selective EP receptor modulators". Drug Discovery Today. 22 (1): 57–71. doi:10.1016/j.drudis.2016.08.003. PMID 27506873.
- 1 2 Narumiya S, Sugimoto Y, Ushikubi F (October 1999). "Prostanoid receptors: structures, properties, and functions". Physiological Reviews. 79 (4): 1193–226. doi:10.1152/physrev.1999.79.4.1193. PMID 10508233. S2CID 7766467.
- ↑ Korbecki J, Baranowska-Bosiacka I, Gutowska I, Chlubek D (2014). "Cyclooxygenase pathways". Acta Biochimica Polonica. 61 (4): 639–49. doi:10.18388/abp.2014_1825. PMID 25343148.
- 1 2 Moreno JJ (December 2016). "Eicosanoid receptors: Targets for the treatment of disrupted intestinal epithelial homeostasis". European Journal of Pharmacology. 796: 7–19. doi:10.1016/j.ejphar.2016.12.004. PMID 27940058. S2CID 1513449.
- ↑ Matsuoka T, Narumiya S (August 2008). "The roles of prostanoids in infection and sickness behaviors". Journal of Infection and Chemotherapy. 14 (4): 270–8. doi:10.1007/s10156-008-0622-3. PMID 18709530. S2CID 207058745.
- ↑ Matsuoka T, Narumiya S (September 2007). "Prostaglandin receptor signaling in disease". TheScientificWorldJournal. 7: 1329–47. doi:10.1100/tsw.2007.182. PMC 5901339. PMID 17767353.
- ↑ Kawano T, Anrather J, Zhou P, Park L, Wang G, Frys KA, Kunz A, Cho S, Orio M, Iadecola C (February 2006). "Prostaglandin E2 EP1 receptors: downstream effectors of COX-2 neurotoxicity". Nature Medicine. 12 (2): 225–9. doi:10.1038/nm1362. PMID 16432513. S2CID 33649705.
- ↑ Fischborn SV, Soerensen J, Potschka H (September 2010). "Targeting the prostaglandin E2 EP1 receptor and cyclooxygenase-2 in the amygdala kindling model in mice". Epilepsy Research. 91 (1): 57–65. doi:10.1016/j.eplepsyres.2010.06.012. PMID 20655707. S2CID 36191106.
- ↑ Khatibi NH, Jadhav V, Matus B, Fathali N, Martin R, Applegate R, Tang J, Zhang JH (2011). "Prostaglandin E2 EP1 Receptor Inhibition Fails to Provide Neuroprotection in Surgically Induced Brain-Injured Mice". Intracerebral Hemorrhage Research. Acta Neurochirurgica Supplementum. Vol. 111. pp. 277–81. doi:10.1007/978-3-7091-0693-8_46. ISBN 978-3-7091-0692-1. PMC 3569069. PMID 21725768.
{{cite book}}:|journal=ignored (help) - ↑ Glushakov AV, Fazal JA, Narumiya S, Doré S (2014). "Role of the prostaglandin E2 EP1 receptor in traumatic brain injury". PLOS ONE. 9 (11): e113689. Bibcode:2014PLoSO...9k3689G. doi:10.1371/journal.pone.0113689. PMC 4245217. PMID 25426930.
Further reading
- Coleman RA, Smith WL, Narumiya S (June 1994). "International Union of Pharmacology classification of prostanoid receptors: properties, distribution, and structure of the receptors and their subtypes". Pharmacological Reviews. 46 (2): 205–29. PMID 7938166.
- Lee TY, Watanabe Y (May 1975). "A nonlinear regression model as applied to the comparison of axis-angles of electrocardiographic systems". Japanese Heart Journal. 16 (3): 243–56. doi:10.1536/ihj.16.243. PMID 1160156.
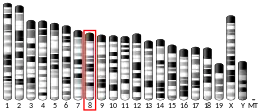
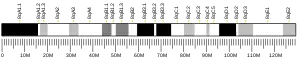
- Duncan AM, Anderson LL, Funk CD, Abramovitz M, Adam M (February 1995). "Chromosomal localization of the human prostanoid receptor gene family". Genomics. 25 (3): 740–2. doi:10.1016/0888-7543(95)80022-E. PMID 7759114.
- Funk CD, Furci L, FitzGerald GA, Grygorczyk R, Rochette C, Bayne MA, Abramovitz M, Adam M, Metters KM (December 1993). "Cloning and expression of a cDNA for the human prostaglandin E receptor EP1 subtype". The Journal of Biological Chemistry. 268 (35): 26767–72. doi:10.1016/S0021-9258(19)74379-8. PMID 8253813.
- Kurihara Y, Endo H, Kondo H (January 2001). "Induction of IL-6 via the EP3 subtype of prostaglandin E receptor in rat adjuvant-arthritic synovial cells". Inflammation Research. 50 (1): 1–5. doi:10.1007/s000110050716. PMID 11235015. S2CID 21908528.
- Kyveris A, Maruscak E, Senchyna M (March 2002). "Optimization of RNA isolation from human ocular tissues and analysis of prostanoid receptor mRNA expression using RT-PCR". Molecular Vision. 8: 51–8. PMID 11951086.
- Matsuoka Y, Furuyashiki T, Bito H, Ushikubi F, Tanaka Y, Kobayashi T, Muro S, Satoh N, Kayahara T, Higashi M, Mizoguchi A, Shichi H, Fukuda Y, Nakao K, Narumiya S (April 2003). "Impaired adrenocorticotropic hormone response to bacterial endotoxin in mice deficient in prostaglandin E receptor EP1 and EP3 subtypes". Proceedings of the National Academy of Sciences of the United States of America. 100 (7): 4132–7. Bibcode:2003PNAS..100.4132M. doi:10.1073/pnas.0633341100. PMC 153060. PMID 12642666.
- Richards JA, Brueggemeier RW (June 2003). "Prostaglandin E2 regulates aromatase activity and expression in human adipose stromal cells via two distinct receptor subtypes". The Journal of Clinical Endocrinology and Metabolism. 88 (6): 2810–6. doi:10.1210/jc.2002-021475. PMID 12788892.
- Kitamura T, Itoh M, Noda T, Tani K, Kobayashi M, Maruyama T, Kobayashi K, Ohuchida S, Sugimura T, Wakabayashi K (July 2003). "Combined effects of prostaglandin E receptor subtype EP1 and subtype EP4 antagonists on intestinal tumorigenesis in adenomatous polyposis coli gene knockout mice". Cancer Science. 94 (7): 618–21. doi:10.1111/j.1349-7006.2003.tb01492.x. PMID 12841871. S2CID 9202306.
- Moreland RB, Kim N, Nehra A, Goldstein I, Traish A (October 2003). "Functional prostaglandin E (EP) receptors in human penile corpus cavernosum". International Journal of Impotence Research. 15 (5): 362–8. doi:10.1038/sj.ijir.3901042. PMID 14562138. S2CID 5845483.
- Su JL, Shih JY, Yen ML, Jeng YM, Chang CC, Hsieh CY, Wei LH, Yang PC, Kuo ML (January 2004). "Cyclooxygenase-2 induces EP1- and HER-2/Neu-dependent vascular endothelial growth factor-C up-regulation: a novel mechanism of lymphangiogenesis in lung adenocarcinoma". Cancer Research. 64 (2): 554–64. doi:10.1158/0008-5472.CAN-03-1301. PMID 14744769. S2CID 8510719.
- Wu T, Wu H, Wang J, Wang J (March 2011). "Expression and cellular localization of cyclooxygenases and prostaglandin E synthases in the hemorrhagic brain". Journal of Neuroinflammation. 8: 22. doi:10.1186/1742-2094-8-22. PMC 3062590. PMID 21385433.
- Han C, Wu T (June 2005). "Cyclooxygenase-2-derived prostaglandin E2 promotes human cholangiocarcinoma cell growth and invasion through EP1 receptor-mediated activation of the epidermal growth factor receptor and Akt". The Journal of Biological Chemistry. 280 (25): 24053–63. doi:10.1074/jbc.M500562200. PMID 15855163.
- Nicola C, Timoshenko AV, Dixon SJ, Lala PK, Chakraborty C (August 2005). "EP1 receptor-mediated migration of the first trimester human extravillous trophoblast: the role of intracellular calcium and calpain". The Journal of Clinical Endocrinology and Metabolism. 90 (8): 4736–46. doi:10.1210/jc.2005-0413. PMID 15886234.
- Durrenberger PF, Facer P, Casula MA, Yiangou Y, Gray RA, Chessell IP, Day NC, Collins SD, Bingham S, Wilson AW, Elliot D, Birch R, Anand P (January 2006). "Prostanoid receptor EP1 and Cox-2 in injured human nerves and a rat model of nerve injury: a time-course study". BMC Neurology. 6: 1. doi:10.1186/1471-2377-6-1. PMC 1361784. PMID 16393343.
- Zhao X, Wu T, Chang CF, Wu H, Han X, Li Q, Gao Y, Li Q, Hou Z, Maruyama T, Zhang J, Wang J (May 2015). "Toxic role of prostaglandin E2 receptor EP1 after intracerebral hemorrhage in mice". Brain, Behavior, and Immunity. 46: 293–310. doi:10.1016/j.bbi.2015.02.011. PMC 4422065. PMID 25697396.
- McGraw DW, Mihlbachler KA, Schwarb MR, Rahman FF, Small KM, Almoosa KF, Liggett SB (May 2006). "Airway smooth muscle prostaglandin-EP1 receptors directly modulate beta2-adrenergic receptors within a unique heterodimeric complex". The Journal of Clinical Investigation. 116 (5): 1400–9. doi:10.1172/JCI25840. PMC 1451203. PMID 16670773.
- Horita H, Kuroda E, Hachisuga T, Kashimura M, Yamashita U (July 2007). "Induction of prostaglandin E2 production by leukemia inhibitory factor promotes migration of first trimester extravillous trophoblast cell line, HTR-8/SVneo". Human Reproduction. 22 (7): 1801–9. doi:10.1093/humrep/dem125. PMID 17525067.
External links
- "Prostanoid Receptors: EP1". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.