| Abortion | |
|---|---|
| Other names | Induced miscarriage, termination of pregnancy |
| Specialty | Obstetrics and gynecology |
| ICD-10-PCS | 10A0 |
| ICD-9-CM | 779.6 |
| MeSH | D000028 |
| MedlinePlus | 007382 |
| eMedicine | 252560 |
Abortion is the termination of a pregnancy by removal or expulsion of an embryo or fetus.[nb 1] An abortion that occurs without intervention is known as a miscarriage or "spontaneous abortion"; these occur in approximately 30% to 40% of all pregnancies.[2][3] When deliberate steps are taken to end a pregnancy, it is called an induced abortion, or less frequently "induced miscarriage". The unmodified word abortion generally refers to an induced abortion.[4][5] The most common reason women give for having an abortion is for birth-timing and limiting family size.[6][7][8] Other reasons reported include maternal health, an inability to afford a child, domestic violence, lack of support, feeling they are too young, wishing to complete education or advance a career, and not being able or willing to raise a child conceived as a result of rape or incest.[6][8][9]
When done legally in industrialized societies, induced abortion is one of the safest procedures in medicine.[10]: 1 [11] In the United States, the risk of maternal mortality is 14 times lower after induced abortion than after childbirth.[12] Unsafe abortions—those performed by people lacking the necessary skills, or in inadequately resourced settings—are responsible for between 5-13% of maternal deaths, especially in the developing world.[13] However, medication abortions that are self-managed are highly effective and safe throughout the first trimester.[14][15][16] Public health data shows that making safe abortion legal and accessible reduces maternal deaths.[17][18]
Modern methods use medication or surgery for abortions.[19] The drug mifepristone in combination with prostaglandin appears to be as safe and effective as surgery during the first and second trimesters of pregnancy.[19][20] The most common surgical technique involves dilating the cervix and using a suction device.[21] Birth control, such as the pill or intrauterine devices, can be used immediately following abortion.[20] When performed legally and safely on a woman who desires it, induced abortions do not increase the risk of long-term mental or physical problems.[22] In contrast, unsafe abortions performed by unskilled individuals, with hazardous equipment, or in unsanitary facilities cause between 22,000 and 44,000 deaths and 6.9 million hospital admissions each year.[23] The World Health Organization states that "access to legal, safe and comprehensive abortion care, including post-abortion care, is essential for the attainment of the highest possible level of sexual and reproductive health".[24] Historically, abortions have been attempted using herbal medicines, sharp tools, forceful massage, or other traditional methods.[25]
Around 73 million abortions are performed each year in the world,[26] with about 45% done unsafely.[27] Abortion rates changed little between 2003 and 2008,[28] before which they decreased for at least two decades as access to family planning and birth control increased.[29] As of 2018, 37% of the world's women had access to legal abortions without limits as to reason.[30] Countries that permit abortions have different limits on how late in pregnancy abortion is allowed.[31] Abortion rates are similar between countries that restrict abortion and countries that broadly allow it, though this is partly because countries which restrict abortion tend to have higher unintended pregnancy rates.[32]
Globally, there has been a widespread trend towards greater legal access to abortion since 1973,[33] but there remains debate with regard to moral, religious, ethical, and legal issues.[34][35] Those who oppose abortion often argue that an embryo or fetus is a person with a right to life, and thus equate it with murder.[36][37] Those who support its legality often argue that it is a woman's reproductive right.[38] Others favor legal and accessible abortion as a public health measure.[39] Abortion laws and views of the procedure are different around the world. In some countries abortion is legal and women have the right to make the choice about abortion.[40] In some areas, abortion is legal only in specific cases such as rape, fetal defects, poverty, risk to a woman's health, or incest.[41]
Types
Induced
Approximately 205 million pregnancies occur each year worldwide. Over a third are unintended and about a fifth end in induced abortion.[28][42] Most abortions result from unintended pregnancies.[43][44] In the United Kingdom, 1 to 2% of abortions are done because of genetic problems in the fetus.[22] A pregnancy can be intentionally aborted in several ways. The manner selected often depends upon the gestational age of the embryo or fetus, which increases in size as the pregnancy progresses.[45][46]
Legality, regional availability, and a woman's or her doctor's personal preference may inform her choice of a specific procedure. Reasons for procuring induced abortions are typically characterized as either therapeutic or elective. An abortion is medically referred to as a therapeutic abortion when it is performed to save the life of the pregnant woman; to prevent harm to the woman's physical or mental health; to terminate a pregnancy where indications are that the child will have a significantly increased chance of mortality or morbidity; or to selectively reduce the number of fetuses to lessen health risks associated with multiple pregnancy.[47][48] An abortion is referred to as elective or voluntary when it is performed at the request of the woman for non-medical reasons.[48] Confusion sometimes arises over the term elective because "elective surgery" generally refers to all scheduled surgery, whether medically necessary or not.[49]
Spontaneous
Miscarriage, also known as spontaneous abortion, is the unintentional expulsion of an embryo or fetus before the 24th week of gestation.[50] A pregnancy that ends before 37 weeks of gestation resulting in a live-born infant is a "premature birth" or a "preterm birth".[51] When a fetus dies in utero after viability, or during delivery, it is usually termed "stillborn".[52] Premature births and stillbirths are generally not considered to be miscarriages, although usage of these terms can sometimes overlap.[53]
Studies of pregnant women in the US and China have shown that between 40% and 60% of embryos do not progress to birth.[54][55][56] The vast majority of miscarriages occur before the woman is aware that she is pregnant,[48] and many pregnancies spontaneously abort before medical practitioners can detect an embryo.[57] Between 15% and 30% of known pregnancies end in clinically apparent miscarriage, depending upon the age and health of the pregnant woman.[58] 80% of these spontaneous abortions happen in the first trimester.[59]
The most common cause of spontaneous abortion during the first trimester is chromosomal abnormalities of the embryo or fetus,[48][60] accounting for at least 50% of sampled early pregnancy losses.[61] Other causes include vascular disease (such as lupus), diabetes, other hormonal problems, infection, and abnormalities of the uterus.[60] Advancing maternal age and a woman's history of previous spontaneous abortions are the two leading factors associated with a greater risk of spontaneous abortion.[61] A spontaneous abortion can also be caused by accidental trauma; intentional trauma or stress to cause miscarriage is considered induced abortion or feticide.[62]
Methods
Medical
Medical abortions are those induced by abortifacient pharmaceuticals. Medical abortion became an alternative method of abortion with the availability of prostaglandin analogs in the 1970s and the antiprogestogen mifepristone (also known as RU-486) in the 1980s.[20][19][63][64]
The most common early first trimester medical abortion regimens use mifepristone in combination with misoprostol (or sometimes another prostaglandin analog, gemeprost) up to 10 weeks (70 days) gestational age,[65][66] methotrexate in combination with a prostaglandin analog up to 7 weeks gestation, or a prostaglandin analog alone.[19] Mifepristone–misoprostol combination regimens work faster and are more effective at later gestational ages than methotrexate–misoprostol combination regimens, and combination regimens are more effective than misoprostol alone, particularly in the second trimester.[63][67] Medical abortion regimens involving mifepristone followed by misoprostol in the cheek between 24 and 48 hours later are effective when performed before 70 days' gestation.[66][65]
In very early abortions, up to 7 weeks gestation, medical abortion using a mifepristone–misoprostol combination regimen is considered to be more effective than surgical abortion (vacuum aspiration), especially when clinical practice does not include detailed inspection of aspirated tissue.[68] Early medical abortion regimens using mifepristone, followed 24–48 hours later by buccal or vaginal misoprostol are 98% effective up to 9 weeks gestational age; from 9 to 10 weeks efficacy decreases modestly to 94%.[65][69] If medical abortion fails, surgical abortion must be used to complete the procedure.[70]
Early medical abortions account for the majority of abortions before 9 weeks gestation in Britain,[71][72] France,[73] Switzerland,[74] United States,[75] and the Nordic countries.[76]
Medical abortion regimens using mifepristone in combination with a prostaglandin analog are the most common methods used for second trimester abortions in Canada, most of Europe, China and India,[64] in contrast to the United States where 96% of second trimester abortions are performed surgically by dilation and evacuation.[77]
A 2020 Cochrane Systematic Review concluded that providing women with medications to take home to complete the second stage of the procedure for an early medical abortion results in an effective abortion.[78] Further research is required to determine if self-administered medical abortion is as safe as provider-administered medical abortion, where a health care professional is present to help manage the medical abortion.[78] Safely permitting women to self-administer abortion medication has the potential to improve access to abortion.[78] Other research gaps that were identified include how to best support women who choose to take the medication home for a self-administered abortion.[78]
Surgical
.svg.png.webp)
1: Amniotic sac
2: Embryo
3: Uterine lining
4: Speculum
5: Vacurette
6: Attached to a suction pump
Up to 15 weeks' gestation, suction-aspiration or vacuum aspiration are the most common surgical methods of induced abortion.[79] Manual vacuum aspiration (MVA) consists of removing the fetus or embryo, placenta, and membranes by suction using a manual syringe, while electric vacuum aspiration (EVA) uses an electric pump. These techniques can both be used very early in pregnancy. MVA can be used up to 14 weeks but is more often used earlier in the U.S. EVA can be used later.[77]
MVA, also known as "mini-suction" and "menstrual extraction", or EVA can be used in very early pregnancy when cervical dilation may not be required. Dilation and curettage (D&C) refers to opening the cervix (dilation) and removing tissue (curettage) via suction or sharp instruments. D&C is a standard gynecological procedure performed for a variety of reasons, including examination of the uterine lining for possible malignancy, investigation of abnormal bleeding, and abortion. The World Health Organization recommends sharp curettage only when suction aspiration is unavailable.[80]
Dilation and evacuation (D&E), used after 12 to 16 weeks, consists of opening the cervix and emptying the uterus using surgical instruments and suction. D&E is performed vaginally and does not require an incision. Intact dilation and extraction (D&X) refers to a variant of D&E sometimes used after 18 to 20 weeks when removal of an intact fetus improves surgical safety or for other reasons.[81]
Abortion may also be performed surgically by hysterotomy or gravid hysterectomy. Hysterotomy abortion is a procedure similar to a caesarean section and is performed under general anesthesia. It requires a smaller incision than a caesarean section and can be used during later stages of pregnancy. Gravid hysterectomy refers to removal of the whole uterus while still containing the pregnancy. Hysterotomy and hysterectomy are associated with much higher rates of maternal morbidity and mortality than D&E or induction abortion.[82]
First trimester procedures can generally be performed using local anesthesia, while second trimester methods may require deep sedation or general anesthesia.[83][84][85]
Labor induction abortion
In places lacking the necessary medical skill for dilation and extraction, or when preferred by practitioners, an abortion can be induced by first inducing labor and then inducing fetal demise if necessary.[86] This is sometimes called "induced miscarriage". This procedure may be performed from 13 weeks gestation to the third trimester. Although it is very uncommon in the United States, more than 80% of induced abortions throughout the second trimester are labor-induced abortions in Sweden and other nearby countries.[87]
Only limited data are available comparing labor-induced abortion with the dilation and extraction method.[87] Unlike D&E, labor-induced abortions after 18 weeks may be complicated by the occurrence of brief fetal survival, which may be legally characterized as live birth. For this reason, labor-induced abortion is legally risky in the United States.[87][88]
Other methods
Historically, a number of herbs reputed to possess abortifacient properties have been used in folk medicine. Among these are: tansy, pennyroyal, black cohosh, and the now-extinct silphium.[89]: 44–47, 62–63, 154–155, 230–231
In 1978, one woman in Colorado died and another developed organ damage when they attempted to terminate their pregnancies by taking pennyroyal oil.[90] Because the indiscriminant use of herbs as abortifacients can cause serious—even lethal—side effects, such as multiple organ failure,[91] such use is not recommended by physicians.
Abortion is sometimes attempted by causing trauma to the abdomen. The degree of force, if severe, can cause serious internal injuries without necessarily succeeding in inducing miscarriage.[92] In Southeast Asia, there is an ancient tradition of attempting abortion through forceful abdominal massage.[93] One of the bas reliefs decorating the temple of Angkor Wat in Cambodia depicts a demon performing such an abortion upon a woman who has been sent to the underworld.[93]
Reported methods of unsafe, self-induced abortion include misuse of misoprostol and insertion of non-surgical implements such as knitting needles and clothes hangers into the uterus. These and other methods to terminate pregnancy may be called "induced miscarriage". Such methods are rarely used in countries where surgical abortion is legal and available.[94]
Safety

The health risks of abortion depend principally upon whether the procedure is performed safely or unsafely. The World Health Organization (WHO) defines unsafe abortions as those performed by unskilled individuals, with hazardous equipment, or in unsanitary facilities.[95] Legal abortions performed in the developed world are among the safest procedures in medicine.[10][96] In the United States as of 2012, abortion was estimated to be about 14 times safer for women than childbirth.[12] CDC estimated in 2019 that US pregnancy-related mortality was 17.2 maternal deaths per 100,000 live births,[97] while the US abortion mortality rate was 0.43 maternal deaths per 100,000 procedures.[11][98][99] In the UK, guidelines of the Royal College of Obstetricians and Gynaecologists state that "Women should be advised that abortion is generally safer than continuing a pregnancy to term."[100] Worldwide, on average, abortion is safer than carrying a pregnancy to term. A 2007 study reported that "26% of all pregnancies worldwide are terminated by induced abortion," whereas "deaths from improperly performed [abortion] procedures constitute 13% of maternal mortality globally."[101] In Indonesia in 2000 it was estimated that 2 million pregnancies ended in abortion, 4.5 million pregnancies were carried to term, and 14-16 percent of maternal deaths resulted from abortion.[102]
In the US from 2000 to 2009, abortion had a mortality rate lower than plastic surgery, lower or similar to running a marathon, and about equivalent to traveling 760 miles (1,220 km) in a passenger car.[11] Five years after seeking abortion services, women who gave birth after being denied an abortion reported worse health than women who had either first or second trimester abortions.[103] The risk of abortion-related mortality increases with gestational age, but remains lower than that of childbirth.[104] Outpatient abortion is as safe from 64 to 70 days' gestation as it before 63 days.[105]
There is little difference in terms of safety and efficacy between medical abortion using a combined regimen of mifepristone and misoprostol and surgical abortion (vacuum aspiration) in early first trimester abortions up to 10 weeks gestation.[68] Medical abortion using the prostaglandin analog misoprostol alone is less effective and more painful than medical abortion using a combined regimen of mifepristone and misoprostol or surgical abortion.[106][107]
Vacuum aspiration in the first trimester is the safest method of surgical abortion, and can be performed in a primary care office, abortion clinic, or hospital. Complications, which are rare, can include uterine perforation, pelvic infection, and retained products of conception requiring a second procedure to evacuate.[108] Infections account for one-third of abortion-related deaths in the United States.[109] The rate of complications of vacuum aspiration abortion in the first trimester is similar regardless of whether the procedure is performed in a hospital, surgical center, or office.[110] Preventive antibiotics (such as doxycycline or metronidazole) are typically given before abortion procedures,[111] as they are believed to substantially reduce the risk of postoperative uterine infection;[83][112] however, antibiotics are not routinely given with abortion pills.[113] The rate of failed procedures does not appear to vary significantly depending on whether the abortion is performed by a doctor or a mid-level practitioner.[114]
Complications after second trimester abortion are similar to those after first trimester abortion, and depend somewhat on the method chosen.[115] The risk of death from abortion approaches roughly half the risk of death from childbirth the farther along a woman is in pregnancy; from one in a million before 9 weeks gestation to nearly one in ten thousand at 21 weeks or more (as measured from the last menstrual period).[116][117] It appears that having had a prior surgical uterine evacuation (whether because of induced abortion or treatment of miscarriage) correlates with a small increase in the risk of preterm birth in future pregnancies. The studies supporting this did not control for factors not related to abortion or miscarriage, and hence the causes of this correlation have not been determined, although multiple possibilities have been suggested.[118][119]
Some purported risks of abortion are promoted primarily by anti-abortion groups,[120][121] but lack scientific support.[120] For example, the question of a link between induced abortion and breast cancer has been investigated extensively. Major medical and scientific bodies (including the WHO, National Cancer Institute, American Cancer Society, Royal College of OBGYN and American Congress of OBGYN) have concluded that abortion does not cause breast cancer.[122]
In the past even illegality has not automatically meant that the abortions were unsafe. Referring to the U.S., historian Linda Gordon states: "In fact, illegal abortions in this country have an impressive safety record."[123]: 25 According to Rickie Solinger,
A related myth, promulgated by a broad spectrum of people concerned about abortion and public policy, is that before legalization abortionists were dirty and dangerous back-alley butchers.... [T]he historical evidence does not support such claims.[124]: 4
Authors Jerome Bates and Edward Zawadzki describe the case of an illegal abortionist in the eastern U.S. in the early 20th century who was proud of having successfully completed 13,844 abortions without any fatality.[125]: 59 In 1870s New York City the famous abortionist/midwife Madame Restell (Anna Trow Lohman) appears to have lost very few women among her more than 100,000 patients[126]—a lower mortality rate than the childbirth mortality rate at the time. In 1936, the prominent professor of obstetrics and gynecology Frederick J. Taussig wrote that a cause of increasing mortality during the years of illegality in the U.S. was that
With each decade of the past fifty years the actual and proportionate frequency of this accident [perforation of the uterus] has increased, due, first, to the increase in the number of instrumentally induced abortions; second, to the proportionate increase in abortions handled by doctors as against those handled by midwives; and, third, to the prevailing tendency to use instruments instead of the finger in emptying the uterus.[127]: 223
Mental health
Current evidence finds no relationship between most induced abortions and mental health problems[22][128] other than those expected for any unwanted pregnancy.[129] A report by the American Psychological Association concluded that a woman's first abortion is not a threat to mental health when carried out in the first trimester, with such women no more likely to have mental-health problems than those carrying an unwanted pregnancy to term; the mental-health outcome of a woman's second or greater abortion is less certain.[129][130] Some older reviews concluded that abortion was associated with an increased risk of psychological problems;[131] however, later reviews of the medical literature found that they did not use an appropriate control group.[128] When a control group is utilized, receiving abortion is not associated with adverse psychological outcomes.[128] However, women seeking abortion who are denied access to abortion have an increase in anxiety after the denial.[128]
Although some studies show negative mental-health outcomes in women who choose abortions after the first trimester because of fetal abnormalities,[132] more rigorous research would be needed to show this conclusively.[133] Some proposed negative psychological effects of abortion have been referred to by anti-abortion advocates as a separate condition called "post-abortion syndrome", but this is not recognized by medical or psychological professionals in the United States.[134]
A 2020 long term-study among US women found that about 99% of women felt that they made the right decision five years after they had an abortion. Relief was the primary emotion with few women feeling sadness or guilt. Social stigma was a main factor predicting negative emotions and regret years later.[135]
Unsafe abortion

Women seeking an abortion may use unsafe methods, especially when it is legally restricted. They may attempt self-induced abortion or seek the help of a person without proper medical training or facilities. This can lead to severe complications, such as incomplete abortion, sepsis, hemorrhage, and damage to internal organs.[136]
Unsafe abortions are a major cause of injury and death among women worldwide. Although data are imprecise, it is estimated that approximately 20 million unsafe abortions are performed annually, with 97% taking place in developing countries.[10] Unsafe abortions are believed to result in millions of injuries.[10][137] Estimates of deaths vary according to methodology, and have ranged from 37,000 to 70,000 in the past decade;[10][138][139] deaths from unsafe abortion account for around 13% of all maternal deaths.[140] The World Health Organization believes that mortality has fallen since the 1990s.[141] To reduce the number of unsafe abortions, public health organizations have generally advocated emphasizing the legalization of abortion, training of medical personnel, and ensuring access to reproductive-health services.[142]
A major factor in whether abortions are performed safely or not is the legal standing of abortion. Countries with restrictive abortion laws have higher rates of unsafe abortion and similar overall abortion rates compared to those where abortion is legal and available.[138][28] For example, the 1996 legalization of abortion in South Africa had an immediate positive impact on the frequency of abortion-related complications,[143] with abortion-related deaths dropping by more than 90%.[144] Similar reductions in maternal mortality have been observed after other countries have liberalized their abortion laws, such as Romania and Nepal.[145] A 2011 study concluded that in the United States, some state-level anti-abortion laws are correlated with lower rates of abortion in that state.[146] The analysis, however, did not take into account travel to other states without such laws to obtain an abortion.[147] In addition, a lack of access to effective contraception contributes to unsafe abortion. It has been estimated that the incidence of unsafe abortion could be reduced by up to 75% (from 20 million to 5 million annually) if modern family planning and maternal health services were readily available globally.[148] Rates of such abortions may be difficult to measure because they can be reported variously as miscarriage, "induced miscarriage", "menstrual regulation", "mini-abortion", and "regulation of a delayed/suspended menstruation".[149][150]
Forty percent of the world's women are able to access therapeutic and elective abortions within gestational limits,[31] while an additional 35 percent have access to legal abortion if they meet certain physical, mental, or socioeconomic criteria.[41] While maternal mortality seldom results from safe abortions, unsafe abortions result in 70,000 deaths and 5 million disabilities per year.[138] Complications of unsafe abortion account for approximately an eighth of maternal mortalities worldwide,[151] though this varies by region.[152] Secondary infertility caused by an unsafe abortion affects an estimated 24 million women.[153] The rate of unsafe abortions has increased from 44% to 49% between 1995 and 2008.[28] Health education, access to family planning, and improvements in health care during and after abortion have been proposed to address consequences of unsafe abortion.[154]
Incidence
There are two commonly used methods of measuring the incidence of abortion:
- Abortion rate – number of abortions annually per 1,000 women between 15 and 44 years of age;[155] some sources use a range of 15–49.
- Abortion percentage – number of abortions out of 100 known pregnancies; pregnancies include live births, abortions, and miscarriages.
In many places, where abortion is illegal or carries a heavy social stigma, medical reporting of abortion is not reliable.[156] For this reason, estimates of the incidence of abortion must be made without determining certainty related to standard error.[28] The number of abortions performed worldwide seems to have remained stable in the early 2000s, with 41.6 million having been performed in 2003 and 43.8 million having been performed in 2008.[28] The abortion rate worldwide was 28 per 1000 women per year, though it was 24 per 1000 women per year for developed countries and 29 per 1000 women per year for developing countries.[28] The same 2012 study indicated that in 2008, the estimated abortion percentage of known pregnancies was at 21% worldwide, with 26% in developed countries and 20% in developing countries.[28]
On average, the incidence of abortion is similar in countries with restrictive abortion laws and those with more liberal access to abortion.[157] Restrictive abortion laws are associated with increases in the percentage of abortions performed unsafely.[31][158][157] The unsafe abortion rate in developing countries is partly attributable to lack of access to modern contraceptives; according to the Guttmacher Institute, providing access to contraceptives would result in about 14.5 million fewer unsafe abortions and 38,000 fewer deaths from unsafe abortion annually worldwide.[159]
The rate of legal, induced abortion varies extensively worldwide. According to the report of employees of Guttmacher Institute it ranged from 7 per 1000 women per year (Germany and Switzerland) to 30 per 1000 women per year (Estonia) in countries with complete statistics in 2008. The proportion of pregnancies that ended in induced abortion ranged from about 10% (Israel, the Netherlands and Switzerland) to 30% (Estonia) in the same group, though it might be as high as 36% in Hungary and Romania, whose statistics were deemed incomplete.[160][161]
An American study in 2002 concluded that about half of women having abortions were using a form of contraception at the time of becoming pregnant. Inconsistent use was reported by half of those using condoms and three-quarters of those using the birth control pill; 42% of those using condoms reported failure through slipping or breakage.[162] The Guttmacher Institute estimated that "most abortions in the United States are obtained by minority women" because minority women "have much higher rates of unintended pregnancy".[163] In a 2022 analysis by the Kaiser Family Foundation, while people of color comprise 44% of the population in Mississippi, 59% of the population in Texas, 42% of the population in Louisiana (by the state Health Department), and 35% of the population in Alabama, they comprise 80%, 74%, 72%, and 70% of those receiving abortions.[164]
The abortion rate may also be expressed as the average number of abortions a woman has during her reproductive years; this is referred to as total abortion rate (TAR).[165]
Gestational age and method


Abortion rates vary depending on the stage of pregnancy and the method practiced. In 2003, the Centers for Disease Control and Prevention (CDC) reported that 26% of reported legal induced abortions in the United States were known to have been obtained at less than 6 weeks' gestation, 18% at 7 weeks, 15% at 8 weeks, 18% at 9 through 10 weeks, 10% at 11 through 12 weeks, 6% at 13 through 15 weeks, 4% at 16 through 20 weeks and 1% at more than 21 weeks. 91% of these were classified as having been done by "curettage" (suction-aspiration, dilation and curettage, dilation and evacuation), 8% by "medical" means (mifepristone), >1% by "intrauterine instillation" (saline or prostaglandin), and 1% by "other" (including hysterotomy and hysterectomy).[166] According to the CDC, due to data collection difficulties the data must be viewed as tentative and some fetal deaths reported beyond 20 weeks may be natural deaths erroneously classified as abortions if the removal of the dead fetus is accomplished by the same procedure as an induced abortion.[8]
The Guttmacher Institute estimated there were 2,200 intact dilation and extraction procedures in the US during 2000; this accounts for <0.2% of the total number of abortions performed that year.[167] Similarly, in England and Wales in 2006, 89% of terminations occurred at or under 12 weeks, 9% between 13 and 19 weeks, and 2% at or over 20 weeks. 64% of those reported were by vacuum aspiration, 6% by D&E, and 30% were medical.[168] There are more second trimester abortions in developing countries such as China, India and Vietnam than in developed countries.[169]
There are both medical and non-medical reasons to have an abortion later in pregnancy (after 20 weeks). A study was conducted from 2008 to 2010 at the University of California San Francisco where more than 440 women were asked about why they experienced delays in obtaining abortion care, if there were any. This study found that almost half of individuals who obtained an abortion after 20 weeks did not suspect that they were pregnant until later in their pregnancy.[170] Other barriers to abortion care found in the study included lack of information about where to access an abortion, difficulties with transportation, lack of insurance coverage, and inability to pay for the abortion procedure.[170]
Medical reasons for seeking an abortion later in pregnancy include fetal anomalies and health risk to the pregnant person.[171] There are diagnostic tests that can diagnose Down Syndrome or cystic fibrosis as early as 10 weeks into gestation, but structural fetal anomalies are often detected much later in pregnancy.[170] A proportion of structural fetal anomalies are lethal, which means that the fetus will almost certainly die before or shortly after birth.[170] Life-threatening conditions may also develop later in pregnancy, such as early severe preeclampsia, newly diagnosed cancer in need of urgent treatment, and intrauterine infection (chorioamnionitis), which often occurs along with premature rupture of the amniotic sac (PPROM).[170] If serious medical conditions such as these arise before the fetus is viable, the person carrying the pregnancy may pursue an abortion to preserve their own health.[170]
Motivation
Personal

The reasons why women have abortions are diverse and vary across the world.[8][6][7] Some of the reasons may include an inability to afford a child, domestic violence, lack of support, feeling they are too young, and the wish to complete education or advance a career.[9] Additional reasons include not being able or willing to raise a child conceived as a result of rape or incest.[6][172]
Societal
Some abortions are undergone as the result of societal pressures.[173] These might include the preference for children of a specific sex or race, disapproval of single or early motherhood, stigmatization of people with disabilities, insufficient economic support for families, lack of access to or rejection of contraceptive methods, or efforts toward population control (such as China's one-child policy). These factors can sometimes result in compulsory abortion or sex-selective abortion.[174] In cultures where there is a preference for male children, some women have sex selective abortions, which have partially replaced the earlier practice of female infanticide.[174]
Maternal and fetal health
An additional factor is maternal health which was listed as the main reason by about a third of women in 3 of 27 countries and about 7% of women in a further 7 of these 27 countries.[8][6]
In the U.S., the Supreme Court decisions in Roe v. Wade and Doe v. Bolton: "ruled that the state's interest in the life of the fetus became compelling only at the point of viability, defined as the point at which the fetus can survive independently of its mother. Even after the point of viability, the state cannot favor the life of the fetus over the life or health of the pregnant woman. Under the right of privacy, physicians must be free to use their "medical judgment for the preservation of the life or health of the mother." On the same day that the Court decided Roe, it also decided Doe v. Bolton, in which the Court defined health very broadly: "The medical judgment may be exercised in the light of all factors—physical, emotional, psychological, familial, and the woman's age—relevant to the well-being of the patient. All these factors may relate to health. This allows the attending physician the room he needs to make his best medical judgment."[175]: 1200–1201
Public opinion shifted in America following television personality Sherri Finkbine's discovery during her fifth month of pregnancy that she had been exposed to thalidomide. Unable to obtain a legal abortion in the United States, she traveled to Sweden. From 1962 to 1965, an outbreak of German measles left 15,000 babies with severe birth defects. In 1967, the American Medical Association publicly supported liberalization of abortion laws. A National Opinion Research Center poll in 1965 showed 73% supported abortion when the mother's life was at risk, 57% when birth defects were present and 59% for pregnancies resulting from rape or incest.[176]
Cancer
The rate of cancer during pregnancy is 0.02–1%, and in many cases, cancer of the mother leads to consideration of abortion to protect the life of the mother, or in response to the potential damage that may occur to the fetus during treatment. This is particularly true for cervical cancer, the most common type of which occurs in 1 of every 2,000–13,000 pregnancies, for which initiation of treatment "cannot co-exist with preservation of fetal life (unless neoadjuvant chemotherapy is chosen)". Very early stage cervical cancers (I and IIa) may be treated by radical hysterectomy and pelvic lymph node dissection, radiation therapy, or both, while later stages are treated by radiotherapy. Chemotherapy may be used simultaneously. Treatment of breast cancer during pregnancy also involves fetal considerations, because lumpectomy is discouraged in favor of modified radical mastectomy unless late-term pregnancy allows follow-up radiation therapy to be administered after the birth.[177]
Exposure to a single chemotherapy drug is estimated to cause a 7.5–17% risk of teratogenic effects on the fetus, with higher risks for multiple drug treatments. Treatment with more than 40 Gy of radiation usually causes spontaneous abortion. Exposure to much lower doses during the first trimester, especially 8 to 15 weeks of development, can cause intellectual disability or microcephaly, and exposure at this or subsequent stages can cause reduced intrauterine growth and birth weight. Exposures above 0.005–0.025 Gy cause a dose-dependent reduction in IQ.[177] It is possible to greatly reduce exposure to radiation with abdominal shielding, depending on how far the area to be irradiated is from the fetus.[178][179]
The process of birth itself may also put the mother at risk. According to Li et al., "[v]aginal delivery may result in dissemination of neoplastic cells into lymphovascular channels, haemorrhage, cervical laceration and implantation of malignant cells in the episiotomy site, while abdominal delivery may delay the initiation of non-surgical treatment."[180]
History and religion

Since ancient times, abortions have been done using a number of methods, including herbal medicines acting as abortifacients, sharp tools through the use of force, or through other traditional medicine methods.[25] Induced abortion has a long history and can be traced back to civilizations as varied as ancient China (abortifacient knowledge is often attributed to the mythological ruler Shennong),[182] ancient India since its Vedic age,[183] ancient Egypt with its Ebers Papyrus (c. 1550 BCE), and the Roman Empire in the time of Juvenal (c. 200 CE).[25] One of the earliest known artistic representations of abortion is in a bas relief at Angkor Wat (c. 1150). Found in a series of friezes that represent judgment after death in Hindu and Buddhist culture, it depicts the technique of abdominal abortion.[93]
In Judaism (Genesis 2:7), the fetus is not considered to have a human soul until it is safely outside of the woman, is viable, and has taken its first breath.[184][185][186] The fetus is considered valuable property of the woman and not a human life while in the womb (Exodus 21:22–23). While Judaism encourages people to be fruitful and multiply by having children, abortion is allowed and is deemed necessary when a pregnant woman's life is in danger.[187][188] Several religions, including Judaism, which disagree that human life begins at conception, support the legality of abortion on religious freedom grounds.[189] In Islam, abortion is traditionally permitted until a point in time when Muslims believe the soul enters the fetus,[25] considered by various theologians to be at conception, 40 days after conception, 120 days after conception, or quickening.[190] Abortion is largely heavily restricted or forbidden in areas of high Islamic faith such as the Middle East and North Africa.[191]
Some medical scholars and abortion opponents have suggested that the Hippocratic Oath forbade physicians in Ancient Greece from performing abortions;[25] other scholars disagree with this interpretation,[25] and state that the medical texts of Hippocratic Corpus contain descriptions of abortive techniques right alongside the Oath.[192] The physician Scribonius Largus wrote in 43 CE that the Hippocratic Oath prohibits abortion, as did Soranus of Ephesus, although apparently not all doctors adhered to it strictly at the time. According to Soranus' 1st or 2nd century CE work Gynaecology, one party of medical practitioners banished all abortives as required by the Hippocratic Oath; the other party to which he belonged was willing to prescribe abortions only for the sake of the mother's health.[193][194] In Politics (350 BCE), Aristotle condemned infanticide as a means of population control. He preferred abortion in such cases,[195][196] with the restriction that it "must be practised on it before it has developed sensation and life; for the line between lawful and unlawful abortion will be marked by the fact of having sensation and being alive."[197]
In the Catholic Church, opinion was divided on how serious abortion was in comparison with such acts as contraception, oral sex, and sex in marriage for pleasure rather than procreation.[198]: 155–167 The Catholic Church did not begin vigorously opposing abortion until the 19th century.[25][189] As early as ~100 CE, the Didache taught that abortion was sinful.[199] Several historians argue that prior to the 19th century most Catholic authors did not regard termination of pregnancy before quickening or ensoulment as an abortion.[200][201][202] Among these authors were the Doctors of the Church, such as St. Augustine, St. Thomas Aquinas, and St. Alphonsus Liguori. In 1588, Pope Sixtus V (r. 1585–1590) was the only Pope before Pope Pius IX (in his 1869 bull, Apostolicae Sedis) to institute a Church policy labeling all abortion as homicide and condemning abortion regardless of the stage of pregnancy.[203][198]: 362–364 [89]: 157–158 Sixtus V's pronouncement was reversed in 1591 by Pope Gregory XIV.[204] In the recodification of 1917 Code of Canon Law, Apostolicae Sedis was strengthened, in part to remove a possible reading that excluded excommunication of the mother.[205] Statements made in the Catechism of the Catholic Church, the codified summary of the Church's teachings, considers abortion from the moment of conception as homicide and called for the end of legal abortion.[206]
Denominations that support abortion rights with some limits include the United Methodist Church, Episcopal Church, Evangelical Lutheran Church in America and Presbyterian Church USA.[207] A 2014 Guttmacher survey of abortion patients in the United States found that many reported a religious affiliation: 24% were Catholic while 30% were Protestant.[208] A 1995 survey reported that Catholic women are as likely as the general population to terminate a pregnancy, Protestants are less likely to do so, and evangelical Christians are the least likely to do so.[8][6] A 2019 Pew Research Center study found that most Christian denominations were against overturning Roe v. Wade, which in the United States legalized abortion, at around 70%, except White Evangelicals at 35%.[209]

Abortion has been a fairly common practice,[211][212] and was not always illegal or controversial until the 19th century.[213][214] Under common law, including early English common law dating back to Edward Coke in 1648,[215] abortion was generally permitted before quickening (14–26 weeks after conception, or between the fourth and sixth month),[216][217][218] and at women's discretion;[189] it was whether abortion was performed after quickening that determined if it was a crime.[215] In Europe and North America, abortion techniques advanced starting in the 17th century; the conservatism of most in the medical profession with regards to sexual matters prevented the wide expansion of abortion techniques.[25][219][220] Other medical practitioners in addition to some physicians advertised their services, and they were not widely regulated until the 19th century when the practice, sometimes called restellism,[221] was banned in both the United States and the United Kingdom.[25][nb 2]
Some 19th-century physicians, one of the most famous and consequential being American Horatio Storer,[222] argued for anti-abortion laws on racist and misogynist as well as moral grounds.[223][224][225] Church groups were also highly influential in anti-abortion movements,[25][213][223] and religious groups more so since the 20th century.[222] Some of the early anti-abortion laws punished only the doctor or abortionist,[189] and while women could be criminally tried for a self-induced abortion,[215] they were rarely prosecuted in general.[213] In the United States, some argued that abortion was more dangerous than childbirth until about 1930 when incremental improvements in abortion procedures relative to childbirth made abortion safer.[nb 3] Others maintain that in the 19th century early abortions under the hygienic conditions in which midwives usually worked were relatively safe.[226][227][228] Several scholars argue that, despite improved medical procedures, the period from the 1930s until the 1970s saw more zealous enforcement of anti-abortion laws, alongside an increasing control of abortion providers by organized crime.[nb 4]
In 1920, Soviet Russia became the first country to legalize abortion after Lenin insisted that no woman be forced to give birth.[229][230] Iceland (1935) and Sweden (1938) would follow suit to legalize certain or all forms of abortion.[231] In Nazi Germany (1935), a law permitted abortions for those deemed "hereditarily ill", while women considered of German stock were specifically prohibited from having abortions.[232] Beginning in the second half of the 20th century, abortion was legalized in a greater number of countries.[25] In Japan, abortion was first legalized by the 1948 "Eugenics Protection Law" meant to prevent the births of "inferior" humans. As of 2022, due to Japan's continuing strongly patriarchal culture and traditional views on women's societal roles, women who want an abortion must normally get written permission from their partner.[233][234]
Society and culture
Abortion debate
Induced abortion has long been the source of considerable debate. Ethical, moral, philosophical, biological, religious and legal issues surrounding abortion are related to value systems. Opinions of abortion may be about fetal rights, governmental authority, and women's rights.
In both public and private debate, arguments presented in favor of or against abortion access focus on either the moral permissibility of an induced abortion, or the justification of laws permitting or restricting abortion.[235] The World Medical Association Declaration on Therapeutic Abortion notes, "circumstances bringing the interests of a mother into conflict with the interests of her unborn child create a dilemma and raise the question as to whether or not the pregnancy should be deliberately terminated."[236] Abortion debates, especially pertaining to abortion laws, are often spearheaded by groups advocating one of these two positions. Groups who favor greater legal restrictions on abortion, including complete prohibition, most often describe themselves as "pro-life" while groups who are against such legal restrictions describe themselves as "pro-choice".[237]
Modern abortion law
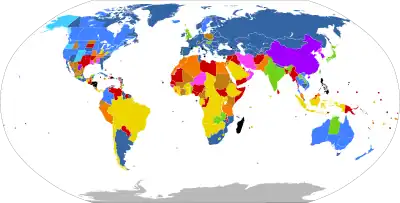
| Legal on request: | |
| No gestational limit | |
| Gestational limit after the first 17 weeks | |
| Gestational limit in the first 17 weeks | |
| Unclear gestational limit | |
| Legally restricted to cases of: | |
| Risk to woman's life, to her health*, rape*, fetal impairment*, or socioeconomic factors | |
| Risk to woman's life, to her health*, rape, or fetal impairment | |
| Risk to woman's life, to her health*, or fetal impairment | |
| Risk to woman's life*, to her health*, or rape | |
| Risk to woman's life or to her health | |
| Risk to woman's life | |
| Illegal with no exceptions | |
| No information | |
| * Does not apply to some countries or territories in that category | |
Current laws pertaining to abortion are diverse. Religious, moral, and cultural factors continue to influence abortion laws throughout the world. The right to life, the right to liberty, the right to security of person, and the right to reproductive health are major issues of human rights that sometimes constitute the basis for the existence or absence of abortion laws.
In jurisdictions where abortion is legal, certain requirements must often be met before a woman may obtain a legal abortion (an abortion performed without the woman's consent is considered feticide and is generally illegal). These requirements usually depend on the age of the fetus, often using a trimester-based system to regulate the window of legality, or as in the U.S., on a doctor's evaluation of the fetus' viability. Some jurisdictions require a waiting period before the procedure, prescribe the distribution of information on fetal development, or require that parents be contacted if their minor daughter requests an abortion.[238] Other jurisdictions may require that a woman obtain the consent of the fetus' father before aborting the fetus, that abortion providers inform women of health risks of the procedure—sometimes including "risks" not supported by the medical literature—and that multiple medical authorities certify that the abortion is either medically or socially necessary. Many restrictions are waived in emergency situations. China, which has ended their[239] one-child policy, and now has a two child policy,[240][241] has at times incorporated mandatory abortions as part of their population control strategy.[242]
Other jurisdictions ban abortion almost entirely. Many, but not all, of these allow legal abortions in a variety of circumstances. These circumstances vary based on jurisdiction, but may include whether the pregnancy is a result of rape or incest, the fetus' development is impaired, the woman's physical or mental well-being is endangered, or socioeconomic considerations make childbirth a hardship.[41] In countries where abortion is banned entirely, such as Nicaragua, medical authorities have recorded rises in maternal death directly and indirectly due to pregnancy as well as deaths due to doctors' fears of prosecution if they treat other gynecological emergencies.[243][244] Some countries, such as Bangladesh, that nominally ban abortion, may also support clinics that perform abortions under the guise of menstrual hygiene.[245] This is also a terminology in traditional medicine.[246] In places where abortion is illegal or carries heavy social stigma, pregnant women may engage in medical tourism and travel to countries where they can terminate their pregnancies.[247] Women without the means to travel can resort to providers of illegal abortions or attempt to perform an abortion by themselves.[248]
The organization Women on Waves has been providing education about medical abortions since 1999. The NGO created a mobile medical clinic inside a shipping container, which then travels on rented ships to countries with restrictive abortion laws. Because the ships are registered in the Netherlands, Dutch law prevails when the ship is in international waters. While in port, the organization provides free workshops and education; while in international waters, medical personnel are legally able to prescribe medical abortion drugs and counseling.[249][250][251]
Sex-selective abortion
Sonography and amniocentesis allow parents to determine sex before childbirth. The development of this technology has led to sex-selective abortion, or the termination of a fetus based on its sex. The selective termination of a female fetus is most common.
Sex-selective abortion is partially responsible for the noticeable disparities between the birth rates of male and female children in some countries. The preference for male children is reported in many areas of Asia, and abortion used to limit female births has been reported in Taiwan, South Korea, India, and China.[252] This deviation from the standard birth rates of males and females occurs despite the fact that the country in question may have officially banned sex-selective abortion or even sex-screening.[253][254][255][256] In China, a historical preference for a male child has been exacerbated by the one-child policy, which was enacted in 1979.[257]
Many countries have taken legislative steps to reduce the incidence of sex-selective abortion. At the International Conference on Population and Development in 1994 over 180 states agreed to eliminate "all forms of discrimination against the girl child and the root causes of son preference",[258] conditions also condemned by a PACE resolution in 2011.[259] The World Health Organization and UNICEF, along with other United Nations agencies, have found that measures to restrict access to abortion in an effort to reduce sex-selective abortions have unintended negative consequences, largely stemming from the fact that women may seek or be coerced into seeking unsafe, extralegal abortions.[258] On the other hand, measures to reduce gender inequality can reduce the prevalence of such abortions without attendant negative consequences.[258][260]
Anti-abortion violence
In a number of cases, abortion providers and these facilities have been subjected to various forms of violence, including murder, attempted murder, kidnapping, stalking, assault, arson, and bombing. Anti-abortion violence is classified by both governmental and scholarly sources as terrorism.[261][262] In the U.S. and Canada, over 8,000 incidents of violence, trespassing, and death threats have been recorded by providers since 1977, including over 200 bombings/arsons and hundreds of assaults.[263] The majority of abortion opponents have not been involved in violent acts.
In the United States, four physicians who performed abortions have been murdered: David Gunn (1993), John Britton (1994), Barnett Slepian (1998), and George Tiller (2009). Also murdered, in the U.S. and Australia, have been other personnel at abortion clinics, including receptionists and security guards such as James Barrett, Shannon Lowney, Lee Ann Nichols, and Robert Sanderson. Woundings (e.g., Garson Romalis) and attempted murders have also taken place in the United States and Canada. Hundreds of bombings, arsons, acid attacks, invasions, and incidents of vandalism against abortion providers have occurred.[264][265] Notable perpetrators of anti-abortion violence include Eric Robert Rudolph, Scott Roeder, Shelley Shannon, and Paul Jennings Hill, the first person to be executed in the United States for murdering an abortion provider.[266]
Legal protection of access to abortion has been brought into some countries where abortion is legal. These laws typically seek to protect abortion clinics from obstruction, vandalism, picketing, and other actions, or to protect women and employees of such facilities from threats and harassment.
Far more common than physical violence is psychological pressure. In 2003, Chris Danze organized anti-abortion organizations throughout Texas to prevent the construction of a Planned Parenthood facility in Austin. The organizations released the personal information online of those involved with construction, sent them up to 1200 phone calls a day and contacted their churches.[267] Some protestors record women entering clinics on camera.[267]
Non-human examples
Spontaneous abortion occurs in various animals. For example, in sheep it may be caused by stress or physical exertion, such as crowding through doors or being chased by dogs.[268] In cows, abortion may be caused by contagious disease, such as brucellosis or Campylobacter, but can often be controlled by vaccination.[269] Eating pine needles can also induce abortions in cows.[270][271] Several plants, including broomweed, skunk cabbage, poison hemlock, and tree tobacco, are known to cause fetal deformities and abortion in cattle[272]: 45–46 and in sheep and goats.[272]: 77–80 In horses, a fetus may be aborted or resorbed if it has lethal white syndrome (congenital intestinal aganglionosis). Foal embryos that are homozygous for the dominant white gene (WW) are theorized to also be aborted or resorbed before birth.[273] In many species of sharks and rays, stress-induced abortions occur frequently on capture.[274]
Viral infection can cause abortion in dogs.[275] Cats can experience spontaneous abortion for many reasons, including hormonal imbalance. A combined abortion and spaying is performed on pregnant cats, especially in trap–neuter–return programs, to prevent unwanted kittens from being born.[276][277][278] Female rodents may terminate a pregnancy when exposed to the smell of a male not responsible for the pregnancy, known as the Bruce effect.[279]
Abortion may also be induced in animals, in the context of animal husbandry. For example, abortion may be induced in mares that have been mated improperly, or that have been purchased by owners who did not realize the mares were pregnant, or that are pregnant with twin foals.[280] Feticide can occur in horses and zebras due to male harassment of pregnant mares or forced copulation,[281][282][283] although the frequency in the wild has been questioned.[284] Male gray langur monkeys may attack females following male takeover, causing miscarriage.[285]
See also
Notes
- ↑ For a list of definitions as stated by obstetrics and gynecology (OB/GYN) textbooks, dictionaries, and other sources, see Definitions of abortion. Definitions of abortion vary from source to source, and language used to define abortion often reflects societal and political opinions, not only scientific knowledge.[1]
- ↑ In the United States, the first laws related to abortion beginning in the 1820s were made to protect women from real or perceived risks, and those more restrictive penalized only the provider. By 1859, abortion was not a crime in 21 out of 33 states, and was prohibited only post-quickening, while penalties for pre-quickening abortions were lower. This changed starting in the 1860s under the influence of anti-immigrant and anti-Catholic sentiment.[189]
- ↑ By 1930, medical procedures in the United States had improved for both childbirth and abortion but not equally, and induced abortion in the first trimester had become safer than childbirth. In 1973, Roe v. Wade acknowledged that abortion in the first trimester was safer than childbirth. For sources, see:
- "The 1970s". Time Communication 1940–1989: Retrospective. Time. 1989.
Blackmun was also swayed by the fact that most abortion prohibitions were enacted in the 19th century when the procedure was more dangerous than now.
- Will GF (1990). Suddenly: The American Idea Abroad and at Home, 1986–1990. Free Press. p. 312. ISBN 0-02-934435-2.
- Lewis J, Shimabukuro JO (28 January 2001). "Abortion Law Development: A Brief Overview". Congressional Research Service. Archived from the original on 14 May 2011. Retrieved 1 May 2011.
- Schultz DA (2002). Encyclopedia of American Law. Infobase Publishing. p. 1. ISBN 0-8160-4329-9. Archived from the original on 9 December 2015.
- Lahey JN (24 September 2009). "Birthing a Nation: Fertility Control Access and the 19th Century Demographic Transition" (PDF; preliminary version). Colloquium. Pomona College. Archived (PDF) from the original on 7 January 2012.
- "The 1970s". Time Communication 1940–1989: Retrospective. Time. 1989.
- ↑ For sources, see:
- James Donner, Women in Trouble: The Truth about Abortion in America, Monarch Books, 1959.
- Ann Oakley, The Captured Womb, Basil Blackwell, 1984, p. 91.
- Rickie Solinger, The Abortionist: A Woman Against the Law, The Free Press, 1994, pp. xi, 5, 16–17, 157–175.
- Leslie J. Reagan, When Abortion Was a Crime: Women, Medicine, and Law in the United States, 1867–1973, University of California Press, 1997.
- Max Evans, Madam Millie: Bordellos from Silver City to Ketchikan, University of New Mexico Press, 2002, pp. 209–218, 230, 267–286, 305.
References
- ↑ Kulczycki A. "Abortion". Oxford Bibliographies. Archived from the original on 13 April 2014. Retrieved 9 April 2014.
- ↑ The Johns Hopkins Manual of Gynecology and Obstetrics (4 ed.). Lippincott Williams & Wilkins. 2012. pp. 438–439. ISBN 9781451148015. Archived from the original on 10 September 2017.
- ↑ "How many people are affected by or at risk for pregnancy loss or miscarriage?". www.nichd.nih.gov. 15 July 2013. Archived from the original on 2 April 2015. Retrieved 14 March 2015.
- ↑ "Home : Oxford English Dictionary". www.oed.com. Archived from the original on 19 August 2020. Retrieved 5 April 2019.
- ↑ "Abortion (noun)". Oxford Living Dictionaries. Archived from the original on 28 May 2018. Retrieved 8 June 2018.
[mass noun] The deliberate termination of a human pregnancy, most often performed during the first 28 weeks of pregnancy
- 1 2 3 4 5 6 Bankole A, Singh S, Haas T (1998). "Reasons Why Women Have Induced Abortions: Evidence from 27 Countries". International Family Planning Perspectives. 24 (3): 117–127, 152. doi:10.2307/3038208. JSTOR 3038208. Archived from the original on 17 January 2006.
Worldwide, the most commonly reported reason women cite for having an abortion is to postpone or stop childbearing. The second most common reason—socioeconomic concerns—includes disruption of education or employment; lack of support from the father; desire to provide schooling for existing children; and poverty, unemployment or inability to afford additional children. In addition, relationship problems with a husband or partner and a woman's perception that she is too young constitute other important categories of reasons. Women's characteristics are associated with their reasons for having an abortion: With few exceptions, older women and married women are the most likely to identify limiting childbearing as their main reason for abortion. - Conclusions - Reasons women give for why they seek abortion are often far more complex than simply not intending to become pregnant; the decision to have an abortion is usually motivated by more than one factor.
- 1 2 Chae S, Desai S, Crowell M, Sedgh G (1 October 2017). "Reasons why women have induced abortions: a synthesis of findings from 14 countries". Contraception. 96 (4): 233–241. doi:10.1016/j.contraception.2017.06.014. PMC 5957082. PMID 28694165.
In most countries, the most frequently cited reasons for having an abortion were socioeconomic concerns or limiting childbearing. With some exceptions, little variation existed in the reasons given by women's sociodemographic characteristics. Data from three countries where multiple reasons could be reported in the survey showed that women often have more than one reason for having an abortion.
- 1 2 3 4 5 6 "The limitations of U.S. statistics on abortion". Issues in Brief. New York: The Guttmacher Institute. 1997. Archived from the original on 4 April 2012.
- 1 2 Stotland NL (July 2019). "Update on Reproductive Rights and Women's Mental Health". The Medical Clinics of North America. 103 (4): 751–766. doi:10.1016/j.mcna.2019.02.006. PMID 31078205. S2CID 153307516.
- 1 2 3 4 5 Grimes DA, Benson J, Singh S, Romero M, Ganatra B, Okonofua FE, Shah IH (25 November 2006). "Unsafe abortion: the preventable pandemic". Lancet. 368 (9550): 1908–1919. doi:10.1016/S0140-6736(06)69481-6. PMID 17126724. S2CID 6188636.
- 1 2 3 Raymond EG, Grossman D, Weaver MA, Toti S, Winikoff B (November 2014). "Mortality of induced abortion, other outpatient surgical procedures and common activities in the United States". Contraception. 90 (5): 476–479. doi:10.1016/j.contraception.2014.07.012. PMID 25152259.
Results: The abortion-related mortality rate in 2000-2009 in the United States was 0.7 per 100,000 abortions. Studies in approximately the same years found mortality rates of 0.8-1.7 deaths per 100,000 plastic surgery procedures, 0-1.7 deaths per 100,000 dental procedures, 0.6-1.2 deaths per 100,000 marathons run and at least 4 deaths among 100,000 cyclists in a large annual bicycling event. The traffic fatality rate per 758 vehicle miles traveled by passenger cars in the United States in 2007-2011 was about equal to the abortion-related mortality rate. Conclusions: The safety of induced abortion as practiced in the United States for the past decade met or exceeded expectations for outpatient surgical procedures and compared favorably to that of two common nonmedical voluntary activities.
- 1 2 Raymond EG, Grimes DA (February 2012). "The comparative safety of legal induced abortion and childbirth in the United States". Obstetrics and Gynecology. 119 (2 Pt 1): 215–219. doi:10.1097/AOG.0b013e31823fe923. PMID 22270271. S2CID 25534071.
Conclusion: Legal induced abortion is markedly safer than childbirth. The risk of death associated with childbirth is approximately 14 times higher than that with abortion. Similarly, the overall morbidity associated with childbirth exceeds that with abortion.
- ↑ "Preventing unsafe abortion". World Health Organization. Archived from the original on 23 August 2019. Retrieved 6 August 2019.
- ↑ "Self-management Recommendation 50: Self-management of medical abortion in whole or in part at gestational ages < 12 weeks (3.6.2) - Abortion care guideline". WHO Department of Sexual and Reproductive Health and Research. 19 November 2021. Retrieved 21 September 2023.
- ↑ Moseson H, Jayaweera R, Raifman S, Keefe-Oates B, Filippa S, Motana R, et al. (October 2020). "Self-managed medication abortion outcomes: results from a prospective pilot study". Reproductive Health. 17 (1): 164. doi:10.1186/s12978-020-01016-4. PMC 7588945. PMID 33109230.
- ↑ Moseson H, Jayaweera R, Egwuatu I, Grosso B, Kristianingrum IA, Nmezi S, et al. (January 2022). "Effectiveness of self-managed medication abortion with accompaniment support in Argentina and Nigeria (SAFE): a prospective, observational cohort study and non-inferiority analysis with historical controls". The Lancet. Global Health. 10 (1): e105–e113. doi:10.1016/S2214-109X(21)00461-7. PMC 9359894. PMID 34801131.
- ↑ Faúndes A, Shah IH (October 2015). "Evidence supporting broader access to safe legal abortion". International Journal of Gynaecology and Obstetrics. World Report on Women's Health 2015: The unfinished agenda of women's reproductive health. 131 (Suppl 1): S56–S59. doi:10.1016/j.ijgo.2015.03.018. PMID 26433508.
A strong body of accumulated evidence shows that the simple means to drastically reduce unsafe abortion-related maternal deaths and morbidity is to make abortion legal and institutional termination of pregnancy broadly accessible. [...] [C]riminalization of abortion only increases mortality and morbidity without decreasing the incidence of induced abortion, and that decriminalization rapidly reduces abortion-related mortality and does not increase abortion rates.
- ↑ Latt SM, Milner A, Kavanagh A (January 2019). "Abortion laws reform may reduce maternal mortality: an ecological study in 162 countries". BMC Women's Health. 19 (1): 1. doi:10.1186/s12905-018-0705-y. PMC 6321671. PMID 30611257.
- 1 2 3 4 Zhang J, Zhou K, Shan D, Luo X (May 2022). "Medical methods for first trimester abortion". The Cochrane Database of Systematic Reviews. 2022 (5): CD002855. doi:10.1002/14651858.CD002855.pub5. PMC 9128719. PMID 35608608.
- 1 2 3 Kapp N, Whyte P, Tang J, Jackson E, Brahmi D (September 2013). "A review of evidence for safe abortion care". Contraception. 88 (3): 350–363. doi:10.1016/j.contraception.2012.10.027. PMID 23261233.
- ↑ "Abortion – Women's Health Issues". Merck Manuals Consumer Version. Archived from the original on 13 July 2018. Retrieved 12 July 2018.
- 1 2 3 Lohr PA, Fjerstad M, Desilva U, Lyus R (2014). "Abortion". BMJ. 348: f7553. doi:10.1136/bmj.f7553. S2CID 220108457.
- ↑ "Induced Abortion Worldwide | Guttmacher Institute". Guttmacher.org. 1 March 2018. Archived from the original on 1 March 2018. Retrieved 23 June 2023.
- ↑ "Abortion". www.who.int. Archived from the original on 6 May 2021. Retrieved 14 April 2021.
- 1 2 3 4 5 6 7 8 9 10 11 Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD, Joffe C (2009). "1. Abortion and medicine: A sociopolitical history" (PDF). Management of Unintended and Abnormal Pregnancy (1st ed.). Oxford: John Wiley & Sons. ISBN 978-1-4443-1293-5. OL 15895486W. Archived (PDF) from the original on 19 January 2012.
- ↑ "Abortion". www.who.int. Archived from the original on 21 September 2022. Retrieved 21 September 2022.
- ↑ "Worldwide, an estimated 25 million unsafe abortions occur each year". World Health Organization. 28 September 2017. Archived from the original on 29 September 2017. Retrieved 29 September 2017.
- 1 2 3 4 5 6 7 8 Sedgh G, Singh S, Shah IH, Ahman E, Henshaw SK, Bankole A (February 2012). "Induced abortion: incidence and trends worldwide from 1995 to 2008" (PDF). Lancet. 379 (9816): 625–632. doi:10.1016/S0140-6736(11)61786-8. PMID 22264435. S2CID 27378192. Archived (PDF) from the original on 6 February 2012.
Because few of the abortion estimates were based on studies of random samples of women, and because we did not use a model-based approach to estimate abortion incidence, it was not possible to compute confidence intervals based on standard errors around the estimates. Drawing on the information available on the accuracy and precision of abortion estimates that were used to develop the subregional, regional, and worldwide rates, we computed intervals of certainty around these rates (webappendix). We computed wider intervals for unsafe abortion rates than for safe abortion rates. The basis for these intervals included published and unpublished assessments of abortion reporting in countries with liberal laws, recently published studies of national unsafe abortion, and high and low estimates of the numbers of unsafe abortion developed by WHO.
- ↑ Sedgh G, Henshaw SK, Singh S, Bankole A, Drescher J (September 2007). "Legal abortion worldwide: incidence and recent trends". International Family Planning Perspectives. 33 (3): 106–116. doi:10.1363/3310607. PMID 17938093. Archived from the original on 19 August 2009.
- ↑ "Induced Abortion Worldwide". Guttmacher Institute. 1 March 2018. Archived from the original on 23 February 2020. Retrieved 21 February 2020.
Of the world's 1.64 billion women of reproductive age, 6% live where abortion is banned outright, and 37% live where it is allowed without restriction as to reason. Most women live in countries with laws that fall between these two extremes.
- 1 2 3 Culwell KR, Vekemans M, de Silva U, Hurwitz M, Crane BB (July 2010). "Critical gaps in universal access to reproductive health: contraception and prevention of unsafe abortion". International Journal of Gynaecology and Obstetrics. 110 (Suppl): S13–S16. doi:10.1016/j.ijgo.2010.04.003. PMID 20451196. S2CID 40586023.
- ↑ "Unintended Pregnancy and Abortion Worldwide". Guttmacher Institute. 28 May 2020. Archived from the original on 23 February 2020. Retrieved 9 March 2021.
Abortion is sought and needed even in settings where it is restricted—that is, in countries where it is prohibited altogether or is allowed only to save the women's life or to preserve her physical or mental health. Unintended pregnancy rates are highest in countries that restrict abortion access and lowest in countries where abortion is broadly legal. As a result, abortion rates are similar in countries where abortion is restricted and those where the procedure is broadly legal (i.e., where it is available on request or on socioeconomic grounds).
- ↑ Staff FP (24 June 2022). "Roe Abolition Makes U.S. a Global Outlier". Foreign Policy. Retrieved 20 October 2023.
- ↑ Paola A, Walker R, LaCivita L (2010). Nixon F (ed.). Medical ethics and humanities. Sudbury, MA: Jones and Bartlett Publishers. p. 249. ISBN 978-0-7637-6063-2. OL 13764930W. Archived from the original on 6 September 2017.
- ↑ Johnstone MJ (2009). "Bioethics a nursing perspective". Confederation of Australian Critical Care Nurses Journal (5th ed.). Sydney, NSW: Churchill Livingstone/Elsevier. 3 (4): 24–30. ISBN 978-0-7295-7873-8. PMID 2129925. Archived from the original on 6 September 2017.
Although abortion has been legal in many countries for several decades now, its moral permissibilities continues to be the subject of heated public debate.
- ↑ Driscoll M (18 October 2013). "What do 55 million people have in common?". Fox News. Archived from the original on 31 August 2014. Retrieved 2 July 2014.
- ↑ Hansen D (18 March 2014). "Abortion: Murder, or Medical Procedure?". The Huffington Post. Archived from the original on 14 July 2014. Retrieved 2 July 2014.
- ↑ Sifris RN (2013). Reproductive freedom, torture and international human rights: challenging the masculinisation of torture. Hoboken, NJ: Taylor & Francis. p. 3. ISBN 978-1-135-11522-7. OCLC 869373168. Archived from the original on 15 October 2015.
- ↑ Åhman E (2007). Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003 (5th ed.). World Health Organization. ISBN 978-92-4-159612-1. Archived from the original on 7 April 2018. Retrieved 24 March 2018.
- ↑ Fabiola Sanchez, Megan Janetsky, Mexico decriminalizes abortion, extending Latin American trend of widening access to procedure, Associated Press (AP), September 6, 2023
- 1 2 3 Boland R, Katzive L (September 2008). "Developments in laws on induced abortion: 1998-2007". International Family Planning Perspectives. 34 (3): 110–120. doi:10.1363/3411008. PMID 18957353. Archived from the original on 7 October 2011.
- ↑ Cheng L (1 November 2008). "Surgical versus medical methods for second-trimester induced abortion". The WHO Reproductive Health Library. World Health Organization. Archived from the original on 1 August 2010. Retrieved 17 June 2011.
- ↑ Bankole A, Singh S, Haas T (1998). "Reasons Why Women Have Induced Abortions: Evidence from 27 Countries". International Family Planning Perspectives. 24 (3): 117–27, 152. doi:10.2307/3038208. JSTOR 3038208. Archived from the original on 17 January 2006.
- ↑ Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM (September 2005). "Reasons U.S. women have abortions: quantitative and qualitative perspectives" (PDF). Perspectives on Sexual and Reproductive Health. 37 (3): 110–118. doi:10.1111/j.1931-2393.2005.tb00045.x. PMID 16150658. Archived (PDF) from the original on 17 January 2006.
- ↑ Stubblefield PG (2002). "10. Family Planning". In Berek JS (ed.). Novak's Gynecology (13 ed.). Lippincott Williams & Wilkins. ISBN 978-0-7817-3262-8.
- ↑ Bartlett LA, Berg CJ, Shulman HB, Zane SB, Green CA, Whitehead S, Atrash HK (2004). "Risk factors for legal induced abortion-related mortality in the United States". Obstetrics & Gynecology. 103 (4): 729–737. doi:10.1097/01.AOG.0000116260.81570.60. PMID 15051566. S2CID 42597014.
- ↑ Roche NE (28 September 2004). "Therapeutic Abortion". eMedicine. Archived from the original on 14 December 2004. Retrieved 19 June 2011.
- 1 2 3 4 Schorge JO, Schaffer JI, Halvorson LM, Hoffman BL, Bradshaw KD, Cunningham FG, eds. (2008). "6. First-Trimester Abortion". Williams Gynecology (1 ed.). McGraw-Hill Medical. ISBN 978-0-07-147257-9.
- ↑ Janiak E, Goldberg AB (1 February 2016). "Eliminating the phrase 'elective abortion': why language matters". Contraception. 93 (2): 89–92. doi:10.1016/j.contraception.2015.10.008. ISSN 0010-7824. PMID 26480889. Archived from the original on 24 January 2023. Retrieved 27 November 2022.
- ↑ Churchill Livingstone medical dictionary. Edinburgh New York: Churchill Livingstone Elsevier. 2008. ISBN 978-0-443-10412-1.
The preferred term for unintentional loss of the product of conception prior to 24 weeks' gestation is miscarriage.
- ↑ AnnasGJ, Elias S (2007). "51. Legal and Ethical Issues in Obstetric Practice". In Gabbe SG, Niebyl JR, Simpson JL (eds.). Obstetrics: Normal and Problem Pregnancies (5th ed.). Churchill Livingstone. p. 669. ISBN 978-0-443-06930-7.
A preterm birth is defined as one that occurs before the completion of 37 menstrual weeks of gestation, regardless of birth weight.
- ↑ Stillbirth. Concise Medical Dictionary. Oxford University Press. 2010. ISBN 978-0199557141. Archived from the original on 15 October 2015.
birth of a fetus that shows no evidence of life (heartbeat, respiration, or independent movement) at any time later than 24 weeks after conception
- ↑ "7 FAM 1470 Documenting Stillbirth (Fetal Death)". United States Department of State. 18 February 2011. Archived from the original on 5 February 2016. Retrieved 12 January 2016.
- ↑ Annas GJ, Elias S (2007). "24. Pregnancy loss". In Gabbe SG, Niebyl JR, Simpson JL (eds.). Obstetrics: Normal and Problem Pregnancies (5th ed.). Churchill Livingstone. ISBN 978-0-443-06930-7.
- ↑ Jarvis GE (7 June 2017). "Early embryo mortality in natural human reproduction: What the data say [version 2; peer review: 2 approved, 1 approved with reservations]". f1000research.com. Archived from the original on 19 January 2022. Retrieved 13 May 2022.
- ↑ Jarvis GE (26 August 2016). "Estimating limits for natural human embryo mortality [version 1; peer review: 2 approved]". f1000research.com. Archived from the original on 24 January 2023. Retrieved 14 May 2022.
- ↑ Katz VL (2007). "16. Spontaneous and Recurrent Abortion – Etiology, Diagnosis, Treatment". In Katz VL, Lentz GM, Lobo RA, Gershenson DM (eds.). Katz: Comprehensive Gynecology (5 th ed.). Mosby. ISBN 978-0-323-02951-3.
- ↑ Stovall TG (2002). "17. Early Pregnancy Loss and Ectopic Pregnancy". In Berek JS (ed.). Novak's Gynecology (13 ed.). Lippincott Williams & Wilkins. ISBN 978-0-7817-3262-8.
- ↑ Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, Casey BM, Sheffield JS, eds. (2014). Williams Obstetrics (24th ed.). McGraw Hill Education. ISBN 978-0-07-179893-8.
- 1 2 Stöppler MS. Shiel Jr WC (ed.). "Miscarriage (Spontaneous Abortion)". MedicineNet.com. WebMD. Archived from the original on 29 August 2004. Retrieved 7 April 2009.
- 1 2 Jauniaux E, Kaminopetros P, El-Rafaey H (1999). "Early pregnancy loss". In Whittle MJ, Rodeck CH (eds.). Fetal medicine: basic science and clinical practice. Edinburgh: Churchill Livingstone. p. 837. ISBN 978-0-443-05357-3. OCLC 42792567.
- ↑ "Fetal Homicide Laws". National Conference of State Legislatures. Archived from the original on 11 September 2012. Retrieved 7 April 2009.
- 1 2 Creinin MD, Gemzell-Danielsson K (2009). "Medical abortion in early pregnancy". In Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD (eds.). Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell. pp. 111–134. ISBN 978-1-4051-7696-5.
- 1 2 Kapp N, von Hertzen H (2009). "Medical methods to induce abortion in the second trimester". In Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD (eds.). Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell. pp. 178–192. ISBN 978-1-4051-7696-5.
- 1 2 3 Chen MJ, Creinin MD (July 2015). "Mifepristone With Buccal Misoprostol for Medical Abortion: A Systematic Review". Obstetrics and Gynecology. 126 (1): 12–21. doi:10.1097/AOG.0000000000000897. PMID 26241251. S2CID 20800109. Archived from the original on 26 July 2020. Retrieved 30 July 2019.
- 1 2 Center for Drug Evaluation and Research (8 February 2019). "Mifeprex (mifepristone) Information". FDA. Archived from the original on 23 April 2019. Retrieved 2 July 2019.
- ↑ Wildschut H, Both MI, Medema S, Thomee E, Wildhagen MF, Kapp N (January 2011). "Medical methods for mid-trimester termination of pregnancy". The Cochrane Database of Systematic Reviews. 2011 (1): CD005216. doi:10.1002/14651858.CD005216.pub2. PMC 8557267. PMID 21249669.
- 1 2 WHO Department of Reproductive Health and Research (2006). Frequently asked clinical questions about medical abortion (PDF). Geneva: World Health Organization. ISBN 92-4-159484-5. Archived from the original (PDF) on 26 December 2011. Retrieved 22 November 2011.
- ↑ Fjerstad M, Sivin I, Lichtenberg ES, Trussell J, Cleland K, Cullins V (September 2009). "Effectiveness of medical abortion with mifepristone and buccal misoprostol through 59 gestational days". Contraception. 80 (3): 282–286. doi:10.1016/j.contraception.2009.03.010. PMC 3766037. PMID 19698822. The regimen (200 mg of mifepristone, followed 24–48 hours later by 800 mcg of vaginal misoprostol) previously used by Planned Parenthood clinics in the United States from 2001 to March 2006 was 98.5% effective through 63 days gestation—with an ongoing pregnancy rate of about 0.5%, and an additional 1% of women having uterine evacuation for various reasons, including problematic bleeding, persistent gestational sac, clinician judgment or a woman's request. The regimen (200 mg of mifepristone, followed 24–48 hours later by 800 mcg of buccal misoprostol) currently used by Planned Parenthood clinics in the United States since April 2006 is 98% effective through 59 days gestation.
- ↑ Holmquist S, Gilliam M (2008). "Induced abortion". In Gibbs RS, Karlan BY, Haney AF, Nygaard I (eds.). Danforth's obstetrics and gynecology (10th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 586–603. ISBN 978-0-7817-6937-2.
- ↑ "Abortion statistics, England and Wales: 2010" (PDF). London: Department of Health, United Kingdom. 24 May 2011. Archived (PDF) from the original on 1 October 2015. Retrieved 22 November 2011.
- ↑ "Abortion statistics, year ending 31 December 2010" (PDF). Edinburgh: ISD, NHS Scotland. 31 May 2011. Archived (PDF) from the original on 26 July 2011. Retrieved 22 November 2011.
- ↑ Vilain A, Mouquet MC (22 June 2011). "Voluntary terminations of pregnancies in 2008 and 2009" (PDF). Paris: DREES, Ministry of Health, France. Archived from the original (PDF) on 26 September 2011. Retrieved 22 November 2011.
- ↑ "Abortions in Switzerland 2010". Neuchâtel: Office of Federal Statistics, Switzerland. 5 July 2011. Archived from the original on 3 October 2011. Retrieved 22 November 2011.
- ↑ Jones RK, Witwer E, Jerman J (2019). Abortion Incidence and Service Availability in the United States, 2017 (Report). Guttmacher Institute. doi:10.1363/2019.30760. PMC 5487028.
- ↑ Gissler M, Heino A (21 February 2011). "Induced abortions in the Nordic countries 2009" (PDF). Helsinki: National Institute for Health and Welfare, Finland. Archived from the original (PDF) on 18 January 2012. Retrieved 22 November 2011.
- 1 2 Meckstroth K, Paul M (2009). "First-trimester aspiration abortion". In Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD (eds.). Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell. pp. 135–156. ISBN 978-1-4051-7696-5.
- 1 2 3 4 Gambir K, Kim C, Necastro KA, Ganatra B, Ngo TD (March 2020). "Self-administered versus provider-administered medical abortion". The Cochrane Database of Systematic Reviews. 2020 (3): CD013181. doi:10.1002/14651858.CD013181.pub2. PMC 7062143. PMID 32150279.
- ↑ Healthwise (2004). "Manual and vacuum aspiration for abortion". WebMD. Archived from the original on 11 February 2007. Retrieved 5 December 2008.
- ↑ World Health Organization (2017). "Dilatation and curettage". Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. Geneva: World Health Organization. ISBN 978-92-4-154587-7. OCLC 181845530. Archived from the original on 19 May 2009. Retrieved 30 July 2019.
- ↑ Hammond C, Chasen S (2009). Dilation and evacuation. In Paul M, Lichtenberg ES Borgatta L Grimes DA Stubblefield P Creinin (eds)Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell. pp. 178–192. ISBN 978-1-4051-7696-5.
- ↑ "ACOG Practice Bulletin No. 135: Second-trimester abortion". Obstetrics and Gynecology. 121 (6): 1394–1406. June 2013. doi:10.1097/01.AOG.0000431056.79334.cc. PMID 23812485. S2CID 205384119.
- 1 2 Templeton A, Grimes DA (December 2011). "Clinical practice. A request for abortion". The New England Journal of Medicine. 365 (23): 2198–2204. doi:10.1056/NEJMcp1103639. PMID 22150038.
- ↑ Allen RH, Singh R (June 2018). "Society of Family Planning clinical guidelines pain control in surgical abortion part 1 - local anesthesia and minimal sedation". Contraception. 97 (6): 471–477. doi:10.1016/j.contraception.2018.01.014. PMID 29407363. S2CID 3777869. Archived from the original on 3 March 2022. Retrieved 20 January 2022.
- ↑ Cansino C, Denny C, Carlisle AS, Stubblefield P (December 2021). "Society of Family Planning clinical recommendations: Pain control in surgical abortion part 2 - Moderate sedation, deep sedation, and general anesthesia". Contraception. 104 (6): 583–592. doi:10.1016/j.contraception.2021.08.007. PMID 34425082. S2CID 237279946. Archived from the original on 3 March 2022. Retrieved 20 January 2022.
- ↑ Borgatta L (December 2014). "Labor Induction Termination of Pregnancy". Global Library of Women's Medicine. GLOWM.10444. doi:10.3843/GLOWM.10444. Archived from the original on 24 September 2015. Retrieved 25 September 2015.
- 1 2 3 Borgatta L, Kapp N (July 2011). "Clinical guidelines. Labor induction abortion in the second trimester". Contraception. 84 (1): 4–18. doi:10.1016/j.contraception.2011.02.005. PMID 21664506. Archived from the original on 6 June 2020. Retrieved 25 September 2015.
10. What is the effect of feticide on labor induction abortion outcome? Deliberately causing demise of the fetus before labor induction abortion is performed primarily to avoid transient fetal survival after expulsion; this approach may be for the comfort of both the woman and the staff, to avoid futile resuscitation efforts. Some providers allege that feticide also facilitates delivery, although little data support this claim. Transient fetal survival is very unlikely after intraamniotic installation of saline or urea, which are directly feticidal. Transient survival with misoprostol for labor induction abortion at greater than 18 weeks ranges from 0% to 50% and has been observed in up to 13% of abortions performed with high-dose oxytocin. Factors associated with a higher likelihood of transient fetal survival with labor induction abortion include increasing gestational age, decreasing abortion interval and the use of nonfeticidal inductive agents such as the PGE1 analogues.
- ↑ 2015 Clinical Policy Guidelines (PDF). National Abortion Federation. 2015. Archived (PDF) from the original on 12 August 2015. Retrieved 30 October 2015.
Policy Statement: Medical induction abortion is a safe and effective method for termination of pregnancies beyond the first trimester when performed by trained clinicians in medical offices, freestanding clinics, ambulatory surgery centers, and hospitals. Feticidal agents may be particularly important when issues of viability arise.
- 1 2 Riddle JM (1997). Eve's herbs: a history of contraception and abortion in the West. Cambridge, MA: Harvard University Press. ISBN 978-0-674-27024-4. OCLC 36126503.
- ↑ Sullivan JB, Rumack BH, Thomas H, Peterson RG, Bryson P (December 1979). "Pennyroyal oil poisoning and hepatotoxicity". JAMA. 242 (26): 2873–2874. doi:10.1001/jama.1979.03300260043027. PMID 513258. S2CID 26198529.
- ↑ Ciganda C, Laborde A (2003). "Herbal infusions used for induced abortion". Journal of Toxicology. Clinical Toxicology. 41 (3): 235–239. doi:10.1081/CLT-120021104. PMID 12807304. S2CID 44851492.
- ↑ Smith JP (1998). "Risky choices: the dangers of teens using self-induced abortion attempts". Journal of Pediatric Health Care. 12 (3): 147–151. doi:10.1016/S0891-5245(98)90245-0. PMID 9652283.
- 1 2 3 4 Potts M, Graff M, Taing J (October 2007). "Thousand-year-old depictions of massage abortion". The Journal of Family Planning and Reproductive Health Care. 33 (4): 233–234. doi:10.1783/147118907782101904. PMID 17925100.
- ↑ Thapa SR, Rimal D, Preston J (September 2006). "Self induction of abortion with instrumentation". Australian Family Physician. 35 (9): 697–698. PMID 16969439. Archived from the original on 8 January 2009.
- ↑ "The Prevention and Management of Unsafe Abortion" (PDF). World Health Organization. April 1992. Archived (PDF) from the original on 30 May 2010. Retrieved 18 October 2017.
- ↑ Grimes DA, Creinin MD (April 2004). "Induced abortion: an overview for internists". Annals of Internal Medicine. 140 (8): 620–626. doi:10.7326/0003-4819-140-8-200404200-00009. PMID 15096333.
- ↑ Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, et al. (May 2019). "Vital Signs: Pregnancy-Related Deaths, United States, 2011-2015, and Strategies for Prevention, 13 States, 2013-2017". MMWR. Morbidity and Mortality Weekly Report. 68 (18): 423–429. doi:10.15585/mmwr.mm6818e1. PMC 6542194. PMID 31071074.
- ↑ National Academies of Sciences Engineering, Health Medicine Division, Board on Health Care Services, Board on Population Health Public Health Practice, Committee on Reproductive Health Services: Assessing the Safety Quality of Abortion Care in the U.S (2018). Read "The Safety and Quality of Abortion Care in the United States" at NAP.edu. doi:10.17226/24950. ISBN 978-0-309-46818-3. PMID 29897702. Archived from the original on 24 July 2020. Retrieved 26 May 2019.
- ↑ Kortsmit K (2022). "Abortion Surveillance — United States, 2020". MMWR. Surveillance Summaries. 71 (10): 1–27. doi:10.15585/mmwr.ss7110a1. ISSN 1546-0738. PMC 9707346. PMID 36417304.
The national case-fatality rate for legal induced abortion for 2013–2019 was 0.43 deaths related to legal induced abortions per 100,000 reported legal abortions. This case-fatality rate was lower than the rates for the previous 5-year periods.
- ↑ Donnelly L (26 February 2011). "Abortion is Safer than Having a Baby, Doctors Say". The Telegraph.
- ↑ Dixon-Mueller R, Germain A (January 2007). "Fertility regulation and reproductive health in the Millennium Development Goals: the search for a perfect indicator". American Journal of Public Health. 97 (1): 45–51. doi:10.2105/AJPH.2005.068056. PMC 1716248. PMID 16571693.
- ↑ "Abortion in Indonesia" (PDF). Guttmacher Institute. 2008. Archived (PDF) from the original on 7 June 2020. Retrieved 13 October 2019.
- ↑ Ralph LJ, Schwarz EB, Grossman D, Foster DG (August 2019). "Self-reported Physical Health of Women Who Did and Did Not Terminate Pregnancy After Seeking Abortion Services: A Cohort Study". Annals of Internal Medicine. 171 (4): 238–247. doi:10.7326/M18-1666. PMID 31181576. S2CID 184482546.
- ↑ Raymond EG, Grimes DA (February 2012). "The comparative safety of legal induced abortion and childbirth in the United States". Obstetrics and Gynecology. 119 (2 Pt 1): 215–219. doi:10.1097/AOG.0b013e31823fe923. PMID 22270271. S2CID 25534071.
- ↑ Abbas D, Chong E, Raymond EG (September 2015). "Outpatient medical abortion is safe and effective through 70 days gestation". Contraception. 92 (3): 197–199. doi:10.1016/j.contraception.2015.06.018. PMID 26118638.
- ↑ Grossman D (3 September 2004). "Medical methods for first trimester abortion: RHL commentary". Reproductive Health Library. Geneva: World Health Organization. Archived from the original on 28 October 2011. Retrieved 22 November 2011.
- ↑ Chien P, Thomson M (15 December 2006). "Medical versus surgical methods for first trimester termination of pregnancy: RHL commentary". Reproductive Health Library. Geneva: World Health Organization. Archived from the original on 17 May 2010. Retrieved 1 June 2010.
- ↑ Westfall JM, Sophocles A, Burggraf H, Ellis S (1998). "Manual vacuum aspiration for first-trimester abortion". Archives of Family Medicine. 7 (6): 559–562. doi:10.1001/archfami.7.6.559. PMID 9821831. Archived from the original on 5 April 2005.
- ↑ Dempsey A (December 2012). "Serious infection associated with induced abortion in the United States". Clinical Obstetrics and Gynecology. 55 (4): 888–892. doi:10.1097/GRF.0b013e31826fd8f8. PMID 23090457.
- ↑ White K, Carroll E, Grossman D (November 2015). "Complications from first-trimester aspiration abortion: a systematic review of the literature". Contraception. 92 (5): 422–438. doi:10.1016/j.contraception.2015.07.013. PMID 26238336.
- ↑ "ACOG practice bulletin No. 104: antibiotic prophylaxis for gynecologic procedures". Obstetrics and Gynecology. 113 (5): 1180–1189. May 2009. doi:10.1097/AOG.0b013e3181a6d011. PMID 19384149.
- ↑ Sawaya GF, Grady D, Kerlikowske K, Grimes DA (May 1996). "Antibiotics at the time of induced abortion: the case for universal prophylaxis based on a meta-analysis". Obstetrics and Gynecology. 87 (5 Pt 2): 884–890. PMID 8677129.
- ↑ Achilles SL, Reeves MF (April 2011). "Prevention of infection after induced abortion: release date October 2010: SFP guideline 20102". Contraception. 83 (4): 295–309. doi:10.1016/j.contraception.2010.11.006. PMID 21397086.
- ↑ Barnard S, Kim C, Park MH, Ngo TD (July 2015). "Doctors or mid-level providers for abortion" (PDF). The Cochrane Database of Systematic Reviews. 2015 (7): CD011242. doi:10.1002/14651858.CD011242.pub2. PMC 9188302. PMID 26214844. Retrieved 24 November 2019.
- ↑ Lerma K, Shaw KA (December 2017). "Update on second trimester medical abortion". Current Opinion in Obstetrics & Gynecology. 29 (6): 413–418. doi:10.1097/GCO.0000000000000409. PMID 28922193. S2CID 12459747.
Second trimester surgical abortion is well tolerated and increasingly expeditious
- ↑ Steinauer J, Jackson A, Grossman D, et al. (Committee on Practice Bulletins-Gynecology) (June 2013). "Second-trimester abortion. Practice Bulletin No. 135". American College of Obstetrics & Gynecology - Practice Bulletins. Archived from the original on 24 December 2019. Retrieved 4 December 2019.
The mortality rate associated with abortion is low (0.6 per 100,000 legal, induced abortions), and the risk of death associated with childbirth is approximately 14 times higher than that with abortion. Abortion-related mortality increases with each week of gestation, with a rate of 0.1 per 100,000 procedures at 8 weeks of gestation or less, and 8.9 per 100,000 procedures at 21 weeks of gestation or greater.
- ↑ Bartlett LA, Berg CJ, Shulman HB, Zane SB, Green CA, Whitehead S, Atrash HK (April 2004). "Risk factors for legal induced abortion-related mortality in the United States". Obstetrics and Gynecology. 103 (4): 729–737. doi:10.1097/01.AOG.0000116260.81570.60. PMID 15051566. S2CID 42597014.
The risk factor that continues to be most strongly associated with mortality from legal abortion is gestational age at the time of the abortion
- ↑ Saccone G, Perriera L, Berghella V (May 2016). "Prior uterine evacuation of pregnancy as independent risk factor for preterm birth: a systematic review and metaanalysis" (PDF). American Journal of Obstetrics and Gynecology. 214 (5): 572–591. doi:10.1016/j.ajog.2015.12.044. PMID 26743506. Archived (PDF) from the original on 27 August 2021. Retrieved 27 June 2020.
Prior surgical uterine evacuation for either I-TOP[induced termination of pregnancy] or SAB[spontaneous abortion, - also known as miscarriage] is an independent risk factor for PTB[pre-term birth]. These data warrant caution in the use of surgical uterine evacuation and should encourage safer surgical techniques as well as medical methods.
- ↑ Averbach SH, Seidman D, Steinauer J, Darney P (January 2017). "Re: Prior uterine evacuation of pregnancy as independent risk factor for preterm birth: a systematic review and metaanalysis". American Journal of Obstetrics and Gynecology. 216 (1): 87. doi:10.1016/j.ajog.2016.08.038. PMID 27596618. Archived from the original on 27 August 2021. Retrieved 28 June 2020.
- 1 2 Jasen P (October 2005). "Breast cancer and the politics of abortion in the United States". Medical History. 49 (4): 423–444. doi:10.1017/S0025727300009145. PMC 1251638. PMID 16562329.
- ↑ Schneider AP, Zainer CM, Kubat CK, Mullen NK, Windisch AK (August 2014). "The breast cancer epidemic: 10 facts". The Linacre Quarterly. Catholic Medical Association. 81 (3): 244–277. doi:10.1179/2050854914Y.0000000027. PMC 4135458. PMID 25249706.
an association between [induced abortion] and breast cancer has been found by numerous Western and non-Western researchers from around the world. This is especially true in more recent reports that allow for a sufficient breast cancer latency period since an adoption of a Western life style in sexual and reproductive behavior.
- ↑ Position statements of major medical bodies on abortion and breast cancer include:
- World Health Organization: "Induced abortion does not increase breast cancer risk (Fact sheet N°240)". World Health Organization. Archived from the original on 13 February 2011. Retrieved 6 January 2011.
- National Cancer Institute: "Abortion, Miscarriage, and Breast Cancer Risk". National Cancer Institute. 20 February 2003. Archived from the original on 21 December 2010. Retrieved 11 January 2011.
- American Cancer Society: "Is Abortion Linked to Breast Cancer?". American Cancer Society. 23 September 2010. Archived from the original on 5 June 2011. Retrieved 20 June 2011.
At this time, the scientific evidence does not support the notion that abortion of any kind raises the risk of breast cancer.
- Royal College of Obstetricians and Gynaecologists: "The Care of Women Requesting Induced Abortion" (PDF). Royal College of Obstetricians and Gynaecologists. p. 9. Archived from the original (PDF) on 27 July 2013. Retrieved 29 June 2008.
Induced abortion is not associated with an increase in breast cancer risk.
- American Congress of Obstetricians and Gynecologists: "ACOG Finds No Link Between Abortion and Breast Cancer Risk". American Congress of Obstetricians and Gynecologists. 31 July 2003. Archived from the original on 2 January 2011. Retrieved 11 January 2011.
- ↑ Gordon L (2002). The Moral Property of Women. University of Illinois Press. ISBN 0-252-02764-7.
- ↑ Solinger R (1998). "Introduction". In Solinger R (ed.). Abortion Wars: A Half Century of Struggle, 1950–2000. University of California Press. pp. 1–9. ISBN 978-0-520-20952-7.
- ↑ Bates JE, Zawadzki ES (1964). Criminal Abortion: A Study in Medical Sociology. Charles C. Thomas. ISBN 978-0-398-00109-4.
- ↑ Keller A (1981). Scandalous Lady: The Life and Times of Madame Restell. Atheneum. ISBN 978-0-689-11213-3.
- ↑ Taussig FJ (1936). Abortion Spontaneous and Induced: Medical and Social Aspects. C.V. Mosby.
- 1 2 3 4 Horvath S, Schreiber CA (September 2017). "Unintended Pregnancy, Induced Abortion, and Mental Health". Current Psychiatry Reports. 19 (11): 77. doi:10.1007/s11920-017-0832-4. PMID 28905259. S2CID 4769393.
- 1 2 "APA Task Force Finds Single Abortion Not a Threat to Women's Mental Health" (Press release). American Psychological Association. 12 August 2008. Archived from the original on 6 September 2011. Retrieved 7 September 2011.
- ↑ "Report of the APA Task Force on Mental Health and Abortion" (PDF). Washington, DC: American Psychological Association. 13 August 2008. Archived (PDF) from the original on 15 June 2010.
- ↑ Coleman PK (September 2011). "Abortion and mental health: quantitative synthesis and analysis of research published 1995-2009". The British Journal of Psychiatry. 199 (3): 180–186. doi:10.1192/bjp.bp.110.077230. PMID 21881096.
- ↑ "Mental Health and Abortion". American Psychological Association. 2008. Archived from the original on 19 April 2012. Retrieved 18 April 2012.
- ↑ Steinberg JR (2011). "Later abortions and mental health: psychological experiences of women having later abortions--a critical review of research". Women's Health Issues. 21 (3 Suppl): S44–S48. doi:10.1016/j.whi.2011.02.002. PMID 21530839.
- ↑ Kelly K (February 2014). "The spread of 'Post Abortion Syndrome' as social diagnosis". Social Science & Medicine. 102: 18–25. doi:10.1016/j.socscimed.2013.11.030. PMID 24565137.
- ↑ Rocca CH, Samari G, Foster DG, Gould H, Kimport K (March 2020). "Emotions and decision rightness over five years following an abortion: An examination of decision difficulty and abortion stigma". Social Science & Medicine. 248: 112704. doi:10.1016/j.socscimed.2019.112704. PMID 31941577.
- ↑ Okonofua F (November 2006). "Abortion and maternal mortality in the developing world" (PDF). Journal of Obstetrics and Gynaecology Canada. 28 (11): 974–979. doi:10.1016/S1701-2163(16)32307-6. PMID 17169222. Archived from the original (PDF) on 11 January 2012.
- ↑ Haddad LB, Nour NM (2009). "Unsafe abortion: unnecessary maternal mortality". Reviews in Obstetrics & Gynecology. 2 (2): 122–126. PMC 2709326. PMID 19609407.
- 1 2 3 Shah I, Ahman E (December 2009). "Unsafe abortion: global and regional incidence, trends, consequences, and challenges" (PDF). Journal of Obstetrics and Gynaecology Canada. 31 (12): 1149–1158. doi:10.1016/s1701-2163(16)34376-6. PMID 20085681. S2CID 35742951. Archived from the original (PDF) on 16 July 2011.
- ↑ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–2128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253. Archived from the original on 19 May 2020. Retrieved 14 March 2020.
- ↑ Speroff L, Darney PD (2010). A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 406. ISBN 978-1-60831-610-6.
- ↑ World Health Organisation (2011). Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008 (PDF) (6th ed.). World Health Organisation. p. 27. ISBN 978-92-4-150111-8. Archived (PDF) from the original on 28 March 2014.
- ↑ Berer M (2000). "Making abortions safe: a matter of good public health policy and practice". Bulletin of the World Health Organization. 78 (5): 580–592. PMC 2560758. PMID 10859852.
- ↑ Jewkes R, Rees H, Dickson K, Brown H, Levin J (March 2005). "The impact of age on the epidemiology of incomplete abortions in South Africa after legislative change". BJOG. 112 (3): 355–359. doi:10.1111/j.1471-0528.2004.00422.x. PMID 15713153. S2CID 41663939.
- ↑ Bateman C (December 2007). "Maternal mortalities 90% down as legal TOPs more than triple". South African Medical Journal = Suid-Afrikaanse Tydskrif vir Geneeskunde. 97 (12): 1238–1242. PMID 18264602. Archived from the original on 30 August 2017.
- ↑ Conti JA, Brant AR, Shumaker HD, Reeves MF (December 2016). "Update on abortion policy". Current Opinion in Obstetrics & Gynecology. 28 (6): 517–521. doi:10.1097/GCO.0000000000000324. PMID 27805969. S2CID 26052790.
- ↑ New MJ (15 February 2011). "Analyzing the Effect of Anti-Abortion U.S. State Legislation in the Post-Casey Era". State Politics & Policy Quarterly. 11 (1): 28–47. doi:10.1177/1532440010387397. S2CID 53314166.
- ↑ Medoff MH, Dennis C (21 July 2014). "Another Critical Review of New's Reanalysis of the Impact of Antiabortion Legislation". State Politics & Policy Quarterly. 14 (3): 269–76. doi:10.1177/1532440014535476. S2CID 155464018.
- ↑ "Facts on Investing in Family Planning and Maternal and Newborn Health" (PDF). Guttmacher Institute. 2010. Archived from the original (PDF) on 24 March 2012. Retrieved 24 May 2012.
- ↑ Grimes DA, Benson J, Singh S, Romero M, Ganatra B, Okonofua FE, Shah IH (November 2006). "Unsafe abortion: the preventable pandemic". Lancet. 368 (9550): 1908–1919. doi:10.1016/S0140-6736(06)69481-6. PMID 17126724. S2CID 6188636. Archived from the original on 5 March 2014. Retrieved 16 January 2010.
- ↑ Nations MK, Misago C, Fonseca W, Correia LL, Campbell OM (June 1997). "Women's hidden transcripts about abortion in Brazil". Social Science & Medicine. 44 (12): 1833–1845. doi:10.1016/s0277-9536(96)00293-6. PMID 9194245.
- ↑ Maclean G (2005). "XI. Dimension, Dynamics and Diversity: A 3D Approach to Appraising Global Maternal and Neonatal Health Initiatives". In Balin RE (ed.). Trends in Midwifery Research. Nova Publishers. pp. 299–300. ISBN 978-1-59454-477-4. Archived from the original on 15 March 2015.
- ↑ Salter C, Johnson HB, Hengen N (1997). "Care for Postabortion Complications: Saving Women's Lives". Population Reports. Johns Hopkins School of Public Health. 25 (1). Archived from the original on 7 December 2009.
- ↑ "Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (PDF). World Health Organization. 2007. Archived (PDF) from the original on 16 February 2011. Retrieved 7 March 2011.
- ↑ UNICEF, UNFPA, WHO, World Bank (2010). "Packages of interventions: Family planning, safe abortion care, maternal, newborn and child health". Archived from the original on 9 November 2010. Retrieved 31 December 2010.
- ↑ "Facts on Induced Abortion Worldwide" (PDF). World Health Organization. January 2012. Archived (PDF) from the original on 9 March 2021. Retrieved 9 May 2021.
- ↑ Sedgh G, Henshaw S, Singh S, Ahman E, Shah IH (October 2007). "Induced abortion: estimated rates and trends worldwide". Lancet. 370 (9595): 1338–1345. CiteSeerX 10.1.1.454.4197. doi:10.1016/S0140-6736(07)61575-X. PMID 17933648. S2CID 28458527.
- 1 2 Rosenthal E (12 October 2007). "Legal or Not, Abortion Rates Compare". The New York Times. Archived from the original on 28 August 2011. Retrieved 18 July 2011.
- ↑ Shah I, Ahman E (December 2009). "Unsafe abortion: global and regional incidence, trends, consequences, and challenges". Journal of Obstetrics and Gynaecology Canada. 31 (12): 1149–1158. doi:10.1016/s1701-2163(16)34376-6. PMID 20085681. S2CID 35742951.
However, a woman's chance of having an abortion is similar whether she lives in a developed or a developing region: in 2003 the rates were 26 abortions per 1,000 women aged 15 to 44 in developed areas and 29 per 1,000 in developing areas. The main difference is in safety, with abortion being safe and easily accessible in developed countries and generally restricted and unsafe in most developing countries.
- ↑ "Facts on Investing in Family Planning and Maternal and Newborn Health" (PDF). Guttmacher Institute. November 2010. Archived from the original (PDF) on 20 October 2011. Retrieved 24 October 2011.
- ↑ Sedgh G, Singh S, Henshaw SK, Bankole A (September 2011). "Legal abortion worldwide in 2008: levels and recent trends". Perspectives on Sexual and Reproductive Health. 43 (3): 188–198. doi:10.1363/4318811. PMID 21884387. Archived from the original on 7 January 2012.
- ↑ "Populație". Romanian Statistical Yearbook (PDF). National Institute of Statistics. 15 May 2011. p. 62. Archived from the original (PDF) on 15 May 2011. Retrieved 16 February 2023.
- ↑ Jones RK, Darroch JE, Henshaw SK (2002). "Contraceptive use among U.S. women having abortions in 2000-2001" (PDF). Perspectives on Sexual and Reproductive Health. 34 (6): 294–303. doi:10.2307/3097748. JSTOR 3097748. PMID 12558092. Archived (PDF) from the original on 15 June 2006.
- ↑ Cohen SA (2008). "Abortion and Women of Color: The Bigger Picture". Guttmacher Policy Review. 11 (3). Archived from the original on 15 September 2008.
- ↑ Pettus EW, Willingham L (1 February 2022). "Minority women most affected if abortion is banned, limited". Associated Press. Archived from the original on 1 February 2022. Retrieved 1 February 2022.
- ↑ Kortsmit, et al. (2021). "Abortion Surveillance — United States, 2019". MMWR. Surveillance Summaries. 70 (9): 1–29. doi:10.15585/mmwr.ss7009a1. ISSN 1546-0738. PMC 8654281. PMID 34818321.
- ↑ Strauss LT, Gamble SB, Parker WY, Cook DA, Zane SB, Hamdan S (November 2006). "Abortion surveillance--United States, 2003". Morbidity and Mortality Weekly Report. Surveillance Summaries. 55 (11): 1–32. PMID 17119534. Archived from the original on 2 June 2017.
- ↑ Finer LB, Henshaw SK (2003). "Abortion incidence and services in the United States in 2000". Perspectives on Sexual and Reproductive Health. 35 (1): 6–15. doi:10.1363/3500603. PMID 12602752. Archived from the original on 22 January 2016.
- ↑ Department of Health (2007). "Abortion statistics, England and Wales: 2006". Archived from the original on 6 December 2010. Retrieved 12 October 2007.
- ↑ Cheng L (1 November 2008). "Surgical versus medical methods for second-trimester induced abortion: RHL commentary". The WHO Reproductive Health Library. Geneva: World Health Organization. Archived from the original on 15 February 2009. Retrieved 10 February 2009. commentary on:
Lohr PA, Hayes JL, Gemzell-Danielsson K (January 2008). "Surgical versus medical methods for second trimester induced abortion". The Cochrane Database of Systematic Reviews (1): CD006714. doi:10.1002/14651858.CD006714.pub2. PMID 18254113. S2CID 205184764. - 1 2 3 4 5 6 "Abortions Later in Pregnancy". KFF (Kaiser Family Foundation). 5 December 2019.
- ↑ Vaughn L (2023). Bioethics: Principles, Issues, and Cases (5th ed.). Oxford University Press. p. 328. ISBN 978-0-19-760902-6.
- ↑ Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM (September 2005). "Reasons U.S. women have abortions: quantitative and qualitative perspectives". Perspectives on Sexual and Reproductive Health. 37 (3): 110–118. doi:10.1111/j.1931-2393.2005.tb00045.x. PMID 16150658. Archived from the original on 7 January 2012.
- ↑ Copelon R (1990). "From Privacy to Autonomy: The Conditions for Reproductive and Sexual Freedom". In Fried MG (ed.). From Abortion to Reproductive Freedom: Transforming a Movement. South End Press. pp. 27–43. ISBN 9780896083875. Archived from the original on 26 January 2021. Retrieved 29 October 2020.
The prevalence of economically influenced abortions and the sterilization campaigns against poor, minority, and disabled women show us that autonomy is impossible without eradication of discrimination and poverty. Racism, sexism, and poverty can make the difference between abortions that reflect choice and those reflecting bitter necessity.
- 1 2 Oster E (September 2005). "Explaining Asia's "Missing Women": A New Look at the Data". Population and Development Review. 31 (3): 529–535. doi:10.1111/j.1728-4457.2005.00082.x. Archived from the original on 7 February 2019. Retrieved 5 February 2019.
Households have variously resorted to female infanticide and postnatal withholding of health care; and since the mid-1980s, when technology permitting fairly low-cost determination of the sex of fetuses became available, there has been a shift toward prenatal sex selection by means of induced abortion.
- ↑ George J. Annas and Sherman Elias. "Legal and Ethical Issues in Obstetrical Practice". Chapter 54 in Obstetrics: Normal and Problem Pregnancies, 6th edition. Eds. Steven G. Gabbe, et al. 2012 Saunders, an imprint of Elsevier. ISBN 978-1-4377-1935-2
- ↑ Doan 2007, p. 57.
- 1 2 Weisz B, Schiff E, Lishner M (2001). "Cancer in pregnancy: maternal and fetal implications". Human Reproduction Update. 7 (4): 384–393. doi:10.1093/humupd/7.4.384. PMID 11476351.
- ↑ Mayr NA, Wen BC, Saw CB (June 1998). "Radiation therapy during pregnancy". Obstetrics and Gynecology Clinics of North America. 25 (2): 301–321. doi:10.1016/s0889-8545(05)70006-1. PMID 9629572.
- ↑ Fenig E, Mishaeli M, Kalish Y, Lishner M (February 2001). "Pregnancy and radiation". Cancer Treatment Reviews. 27 (1): 1–7. doi:10.1053/ctrv.2000.0193. PMID 11237773.
- ↑ Li WW, Yau TN, Leung CW, Pong WM, Chan MY (February 2009). "Large-cell neuroendocrine carcinoma of the uterine cervix complicating pregnancy". Hong Kong Medical Journal = Xianggang Yi Xue Za Zhi. 15 (1): 69–72. PMID 19197101.
- ↑ Mould RF (1996). Mould's Medical Anecdotes. CRC Press. p. 406. ISBN 978-0-85274-119-1.
- ↑ Himes NE (1963). Medical History of Contraception. Gamut Press. pp. 109–110.
- ↑ Misra P (2006). Domestic Violence Against Women: Legal Control and Judicial Response. Deep & Deep Publications. pp. 79–80. ISBN 978-81-7629-896-4. Archived from the original on 9 July 2021. Retrieved 5 July 2021.
References in Atharva Veda show that abortion was known in the Vedic age.
- ↑ Schenker JG (June 2008). "The beginning of human life : status of embryo. Perspectives in Halakha (Jewish Religious Law)". Journal of Assisted Reproduction and Genetics. 25 (6): 271–276. doi:10.1007/s10815-008-9221-6. PMC 2582082. PMID 18551364.
- ↑ Rosner F (2001). Biomedical Ethics and Jewish Law. KTAV Publishing House. ISBN 978-0881257014. Archived from the original on 24 January 2023. Retrieved 27 July 2022 – via Google Books. Reprinted as Rosner F (7 June 2015). "The Beginning of Life in Judaism". My Jewish Learning. Archived from the original on 7 June 2015. Retrieved 27 July 2022.
- ↑ Milgram G (23 January 2022). "When Does Life Begin? A Jewish View". Reclaiming Judaism. Archived from the original on 3 August 2022. Retrieved 30 June 2022.
- ↑ "Judaism and Abortion" (PDF). National Council of Jewish Women. May 2019. Archived (PDF) from the original on 9 October 2022. Retrieved 27 July 2022.
- ↑ Kestler-D'Amours J (17 June 2022). "Religious freedom: The next battleground for US abortion rights?". Al Jazeera. Archived from the original on 1 August 2022. Retrieved 27 July 2022.
- 1 2 3 4 5 Georgian E (1 July 2022). "The End of Roe in Historical Perspective". Clio and the Contemporary. Archived from the original on 27 July 2022. Retrieved 27 July 2022.
- ↑ "Religions – Islam: Abortion". BBC. 9 July 2009. Archived from the original on 9 October 2011. Retrieved 10 December 2011.
- ↑ Dabash R, Farzaneh RF (2008). "Abortion in the Middle East and North Africa" (PDF). Population Research Bureau. Archived (PDF) from the original on 6 October 2011.
- ↑ Miles SH (2005). The Hippocratic Oath and the Ethics of Medicine. Oxford University Press. ISBN 978-0-19-518820-2.
- ↑ Soranus (1991). Soranus' Gynecology. Translated by Temkin O, Eastman NJ, Edelstein L, Guttmacher AF. Johns Hopkins University Press. p. I, 19, 60. ISBN 978-0-8018-4320-4. Archived from the original on 15 October 2015. Retrieved 6 October 2015.
{{cite book}}: CS1 maint: overridden setting (link) - ↑ "Scribonius Largus and the Oath of Hippocrates". Encyclopaedia Romana. University of Chicago. Retrieved 27 July 2022.
- ↑ Carrick P (2001). Medical Ethics in the Ancient World. Georgetown University Press. ISBN 978-0-87840-849-8.
- ↑ Meyer HS (17 April 2002). "Ancient Ethics: Medical Ethics in the Ancient World". JAMA. American Medical Association. 287 (15): 2005–2006. doi:10.1001/jama.287.15.2005-JBK0417-3-1. S2CID 240484236.
- ↑ Aristotele (1944). Aristotle, Politics. Translated by Rackham H. Harvard University Press. Archived from the original on 22 June 2011. Retrieved 21 June 2011 – via Perseus.
- 1 2 Noonan JT (1986). Contraception: A History of Its Treatment by the Catholic Theologians and Canonists (2nd ed.). Harvard University Press.
- ↑ "Didache" (PDF). Legacy Icons. 9 September 2016. Archived (PDF) from the original on 8 November 2020. Retrieved 16 May 2022.
- ↑ Joan Cadden, "Western medicine and natural philosophy", in Vern L. Bullough and James A. Brundage, eds., Handbook of Medieval Sexuality, Garland, 1996, pp. 51–80.
- ↑ Cyril C. Means Jr., "A historian's view", in Robert E. Hall, ed., Abortion in a Changing World, vol. 1, Columbia University Press, 1970, pp. 16–24.
- ↑ John M. Riddle, "Contraception and early abortion in the Middle Ages", in Vern L. Bullough and James A. Brundage, eds., Handbook of Medieval Sexuality, Garland, 1996, pp. 261–277, ISBN 978-0-8153-1287-1.
- ↑ Pope Sixtus V (1588). "Effraenatam". Archived from the original on 26 May 2021. Retrieved 26 May 2021 – via The Embryo Project Encyclopedia.
- ↑ Gershon L (13 February 2018). "What a 16th-Century Abortion Ban Revealed". JSTOR Daily. Archived from the original on 26 May 2021. Retrieved 26 May 2021.
- ↑ "Apostolicae Sedis Moderationi". New Advent. Archived from the original on 16 May 2022. Retrieved 16 May 2022.
- ↑ "Catechism of the Catholic Church – The fifth commandment". Vatican. 1992. Archived from the original on 14 May 2011. Retrieved 4 December 2019.
- ↑ Masci D (30 May 2020). "Where major religious groups stand on abortion". Pew Research Center. Archived from the original on 22 January 2023. Retrieved 22 January 2023.
- ↑ Jerman J, Jones RK, Onda T (10 May 2016). Characteristics of U.S. Abortion Patients in 2014 and Changes Since 2008 (Report). Guttmacher. Archived from the original on 24 February 2021. Retrieved 25 February 2021.
- ↑ "8 key findings about Catholics and abortion". Pew Research Center. Archived from the original on 15 May 2022. Retrieved 15 May 2022.
- ↑ Hull NE, Hoffer W, Hoffer PC, eds. (2004). The abortion rights controversy in America : a legal reader. Chapel Hill: University of North Carolina Press. p. 17. ISBN 0-8078-2873-4. OCLC 53993049.
- ↑ Reagan LJ (2022) [1997]. When Abortion Was a Crime: Women, Medicine and the Law in the United States, 1867–1973 (1st ed.). Berkeley: University of California Press. ISBN 978-0520387416.
- ↑ Blakemore E (22 May 2022). "The complex early history of abortion in the United States". National Geographic. Archived from the original on 26 July 2022. Retrieved 26 July 2022.
But that view of history is the subject of great dispute. Though interpretations differ, most scholars who have investigated the history of abortion argue that terminating a pregnancy wasn't always illegal—or even controversial.
- 1 2 3 Hardin G (December 1978). "Abortion in America. The Origins and Evolution of National Policy, 1800–1900. James C. Mohr". The Quarterly Review of Biology. 53 (4): 499. doi:10.1086/410954.
The long silence had led us to assume that opposition to abortion had existed from time immemorial. Not so: most of the opposition to, and all of the laws against, abortion arose in the 19th century. Historian Mohr amply documents the earlier acceptance of abortion. ... In the 19th century even many of the feminists expressed horror at abortion, urging abstinence instead. Not so in the 20th century. In the 19th century the medical profession was fairly united against abortion; Mohr argues that this arose from the commercial competition between the 'regulars' (men with M.D.'s) and the irregulars (women without M.D.'s). ... A key role in generating prohibition laws was played by the press, ... . By 1900 the abortion-prohibition laws were immune to questioning, as they remained until the 1960's when feminists and a new breed of physicians combined to arouse the public to the injustice of the law. ... the Roe v. Wade decision of the Supreme Court ... essentially returned the practice of abortion to the permissive state ante 1820.
- ↑ Acevedo ZP (Summer 1979). "Abortion in early America". Women Health. 4 (2): 159–167. doi:10.1300/J013v04n02_05. PMID 10297561.
This piece describes abortion practices in use from the 1600s to the 19th century among the inhabitants of North America. The abortive techniques of women from different ethnic and racial groups as found in historical literature are revealed. Thus, the point is made that abortion is not simply a 'now issue' that effects select women. Instead, it is demonstrated that it is a widespread practice as solidly rooted in our past as it is in the present.
- 1 2 3 Alford S (2003). "Is Self-Abortion a Fundamental Right?". Duke Law Journal. 52 (5): 1011–1029. JSTOR 1373127. PMID 12964572.
- ↑ Dine R (8 August 2013). "Scarlet Letters: Getting the History of Abortion and Contraception Right". Center for American Progress. Archived from the original on 28 July 2022. Retrieved 26 July 2022.
- ↑ Reagan LJ (2 June 2022). "What Alito Gets Wrong About the History of Abortion in America". Politico. Archived from the original on 23 June 2022. Retrieved 26 July 2022.
- ↑ Root D (23 June 2022). "Alito's Leaked Abortion Opinion Misunderstands Unenumerated Rights". Reason. Archived from the original on 27 July 2022. Retrieved 27 July 2022.
- ↑ Mohr JC (1978). Abortion in America: The Origins and Evolution of National Policy. Oxford University Press. pp. 35–36. ISBN 978-0195026160.
- ↑ Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD, Joffe C (2009). "Abortion and Medicine: A Sociopolitical History" (PDF). Management of Unintended and Abnormal Pregnancy (1st ed.). Oxford: John Wiley & Sons. ISBN 978-1-4443-1293-5. OL 15895486W. Archived (PDF) from the original on 19 January 2012.
- ↑ Dannenfelser M (4 November 2015). "The Suffragettes Would Not Agree With Feminists Today on Abortion". Time. Archived from the original on 6 November 2015. Retrieved 4 November 2015.
- 1 2 Samuels A, Potts M (25 July 2022). "How The Fight To Ban Abortion Is Rooted In The 'Great Replacement' Theory". FiveThirtyEight. Archived from the original on 25 July 2022. Retrieved 26 July 2022.
- 1 2 Abdeltath R, Arablouei R, Caine J, Kaplan-Levenson L, Wu L, Yvellez V, et al. "Before Roe: The Physicians' Crusade". Throughline. NPR. Archived from the original on 26 July 2022. Retrieved 26 July 2022.
- ↑ Poole WS (2009). Satan in America: The Devil We Know. Rowman & Littlefield. p. 86. ISBN 978-0742561717. Retrieved 20 March 2023.
- ↑ Wilson C (2 November 2020). "Nostalgia, Entitlement and Victimhood: The Synergy of White Genocide and Misogyny". Terrorism and Political Violence. Routledge. 34 (8): 1810–1825. doi:10.1080/09546553.2020.1839428. S2CID 228837398. Storer is cited at p. 4.
- ↑ Lee CA (1838). "Report of a Trial for Murder". American Journal of the Medical Sciences. XXII: 351–353.
- ↑ Benjamin Bailey, "Induction of abortion and premature labor", North American Journal of Homeopathy, vol. XI, no. 3 (1896), pp. 144–150.
- ↑ Keith Simpson, Forensic Medicine, Edward Arnold Publishers, 1969 [first published 1947], pp. 173–174.
- ↑ Bullough V (2001). Encyclopedia of Birth Control. ABC-CLIO E-Books. ABC-CLIO. p. 5. ISBN 978-1-57607-181-6. Archived from the original on 24 January 2023. Retrieved 19 October 2022.
- ↑ Raphael D (2011). Being Female: Reproduction, Power, and Change. World Anthropology. De Gruyter. p. 30. ISBN 978-3-11-081312-8. Archived from the original on 24 January 2023. Retrieved 19 October 2022.
- ↑ "Abortion Law, History & Religion". Childbirth By Choice Trust. Archived from the original on 8 February 2008. Retrieved 23 March 2008.
- ↑ For sources describing abortion policy in Nazi Germany, see:
- Friedlander H (1995). The origins of Nazi genocide: from euthanasia to the final solution. Chapel Hill: University of North Carolina Press. p. 30. ISBN 978-0-8078-4675-9. OCLC 60191622. Archived from the original on 29 July 2016.
- Proctor RN (1988). Racial Hygiene: Medicine Under the Nazis. Harvard University Press. pp. 122–123, 366. ISBN 978-0-674-74578-0. OCLC 20760638.
- Arnot ML, Usborne C (1999). Gender and Crime in Modern Europe. New York: Routledge. p. 231. ISBN 978-1-85728-745-5. OCLC 186748539.
- DiMeglio PM (1999). "Germany 1933–1945 (National Socialism)". In Tierney H (ed.). Women's Studies Encyclopedia. Westport, Connecticut: Greenwood Press. p. 589. ISBN 978-0-313-31072-0. OCLC 38504469. Archived from the original on 15 October 2015.
- ↑ Ye Hee Lee M (14 June 2022). "In Japan, Abortion is Legal -- But Most Women Need Their Husband's Consent". Retrieved 16 March 2023.
- ↑ Wingfield-Hayes R (31 August 2022). "Abortion pill: Why Japanese women will need their partner's consent to get a tablet". BBC News. Retrieved 15 March 2023.
It was actually one of the first countries in the world to pass an abortion law, back in 1948. But it was part of the Eugenics Protection Law - yes, it really was called that. It had nothing to do with giving women more control over their reproductive health. Rather, it was about preventing "inferior" births. ... So, to this day, women who want an abortion must get written permission from their husband, partner, or in some cases their boyfriend. ... Unlike the US, Japanese views on abortion are not driven by religious belief. Instead, they derive from a long history of patriarchy and deeply traditional views on the role of women and motherhood.
- ↑ Farrell C (2010). Abortion Debate. ABDO Publishing Company. pp. 6–7. ISBN 978-1-61785-264-0.
- ↑ "WMA Declaration on Therapeutic Abortion". World Medical Association. Archived from the original on 28 October 2015. Retrieved 28 October 2015.
- ↑ Farrell, p. 8
- ↑ Joyce TJ, Henshaw SK, Dennis A, Finer LB, Blanchard K (April 2009). "The Impact of State Mandatory Counseling and Waiting Period Laws on Abortion: A Literature Review" (PDF). Guttmacher Institute. Archived from the original (PDF) on 16 March 2012. Retrieved 31 December 2010.
- ↑ Phillips T (29 October 2015). "China ends one-child policy after 35 years". The Guardian. ISSN 0261-3077. Archived from the original on 1 December 2016. Retrieved 30 November 2016.
- ↑ Buckley C (29 October 2015). "China Ends One-Child Policy, Allowing Families Two Children". The New York Times. ISSN 0362-4331. Archived from the original on 24 November 2016. Retrieved 30 November 2016.
- ↑ "China to end one-child policy and allow two". BBC News. 29 October 2015. Archived from the original on 21 November 2016. Retrieved 30 November 2016.
- ↑ Restivo SP, ed. (2005). Science, Technology, and Society: An Encyclopedia. Oxford University Press. p. 2. ISBN 978-0-19-514193-1. Archived from the original on 15 March 2015.
- ↑ "European delegation visits Nicaragua to examine effects of abortion ban". Ipas. 26 November 2007. Archived from the original on 17 April 2008. Retrieved 15 June 2009.
More than 82 maternal deaths had been registered in Nicaragua since the change. During this same period, indirect obstetric deaths, or deaths caused by illnesses aggravated by the normal effects of pregnancy and not due to direct obstetric causes, have doubled.
- ↑ "Nicaragua: 'The Women's Movement Is in Opposition'". Montevideo: Inside Costa Rica. IPS. 28 June 2008. Archived from the original on 6 June 2011.
- ↑ "Surgical Abortion: History and Overview". National Abortion Federation. Archived from the original on 22 September 2006. Retrieved 4 September 2006.
- ↑ Nations MK, Misago C, Fonseca W, Correia LL, Campbell OM (June 1997). "Women's hidden transcripts about abortion in Brazil". Social Science & Medicine. 44 (12): 1833–1845. doi:10.1016/s0277-9536(96)00293-6. PMID 9194245.
Two folk medical conditions, "delayed" (atrasada) and "suspended" (suspendida) menstruation, are described as perceived by poor Brazilian women in Northeast Brazil. Culturally prescribed methods to "regulate" these conditions and provoke menstrual bleeding are also described ...
- ↑ Henshaw SK (1991). "The accessibility of abortion services in the United States" (PDF). Family Planning Perspectives. 23 (6): 246–52, 263. CiteSeerX 10.1.1.360.6115. doi:10.2307/2135775. JSTOR 2135775. PMID 1786805. Archived (PDF) from the original on 24 March 2016. Retrieved 25 October 2017.
- ↑ Bloom M (25 February 2008). "Need Abortion, Will Travel". RH Reality Check. Archived from the original on 30 November 2008. Retrieved 15 June 2009.
- ↑ Gomperts R (May 2002). "Women on waves: where next for the abortion boat?". Reproductive Health Matters. 10 (19): 180–183. doi:10.1016/S0968-8080(02)00004-6. PMID 12369324.
- ↑ Best A (2005). "Abortion Rights along the Irish-English Border and the Liminality of Women's Experiences". Dialectical Anthropology. 29 (3–4): 423–37. doi:10.1007/s10624-005-3863-x. ISSN 0304-4092. S2CID 145318165.
- ↑ Lambert-Beatty C (2008). "Twelve miles: Boundaries of the new art/activism". Signs: Journal of Women in Culture and Society. 33 (2): 309–27. doi:10.1086/521179. S2CID 147307705.
- ↑ Banister, Judith. (16 March 1999). Son Preference in Asia – Report of a Symposium Archived 16 February 2006 at the Wayback Machine. Retrieved 12 January 2006.
- ↑ Reaney P. "Selective abortion blamed for India's missing girls". Reuters. Archived from the original on 20 February 2006. Retrieved 3 December 2008.
- ↑ Sudha S, Irudaya RS (July 1999). "Female demographic disadvantage in India 1981-1991: sex selective abortions and female infanticide". Development and Change. 30 (3): 585–618. doi:10.1111/1467-7660.00130. PMID 20162850. S2CID 33446683. Archived from the original on 1 January 2003. Retrieved 3 December 2008.
- ↑ "Sex Selection & Abortion: India". Library of Congress. 4 April 2011. Archived from the original on 27 September 2011. Retrieved 18 July 2011.
- ↑ "China Bans Sex-selection Abortion". www.china.org.cn. Xinhua News Agency. 22 March 2003. Retrieved 16 February 2023.
- ↑ Graham MJ, Larsen U, Xu X (June 1998). "Son Preference in Anhui Province, China". International Family Planning Perspectives. 24 (2): 72–77. doi:10.2307/2991929. JSTOR 2991929. Archived from the original on 6 January 2012.
- 1 2 3 "Preventing gender-biased sex selection" (PDF). UNFPA. Archived (PDF) from the original on 11 October 2011. Retrieved 1 November 2011.
- ↑ "Prenatal sex selection" (PDF). Parliamentary Assembly of the Council of Europe. Archived from the original (PDF) on 3 October 2011. Retrieved 17 November 2015.
- ↑ Das Gupta M (2019). "Is banning sex-selection the best approach for reducing prenatal discrimination?". Asian Population Studies. 15 (3): 319–336. doi:10.1080/17441730.2019.1671015. PMC 8153244. PMID 34046078.
- ↑ Smith GD (1998). "Single Issue Terrorism Commentary". Canadian Security Intelligence Service. Archived from the original on 15 October 2007. Retrieved 1 September 2011.
- ↑ Wilson M, Lynxwiler J (1988). "Abortion clinic violence as terrorism". Terrorism. 11 (4): 263–273. doi:10.1080/10576108808435717. PMID 11618209.
- ↑ National Abortion Federation (2017). "2017 violence and disruption statistics" (PDF). Archived (PDF) from the original on 28 July 2020. Retrieved 26 May 2019.
- ↑ "The Death of Dr. Gunn". The New York Times. 12 March 1993. Archived from the original on 10 November 2016.
- ↑ "Incidence of Violence & Disruption Against Abortion Providers in the U.S. & Canada" (PDF). National Abortion Federation. 2009. Archived (PDF) from the original on 13 June 2010. Retrieved 9 February 2010.
- ↑ Borger J (3 February 1999). "The bomber under siege". The Guardian. London. Archived from the original on 22 February 2017.
- 1 2 Doan 2007, p. 2.
- ↑ Spencer JB (1908). Sheep Husbandry in Canada. p. 114. OCLC 798508694.
- ↑ "Beef cattle and Beef production: Management and Husbandry of Beef Cattle". Encyclopaedia of New Zealand. 1966. Archived from the original on 1 January 2009.
- ↑ Myers B, Beckett J (2001). "Pine needle abortion" (PDF). Animal Health Care and Maintenance. Tucson: Arizona Cooperative Extension, University of Arizona. pp. 47–50. Archived from the original (PDF) on 28 July 2015. Retrieved 10 April 2013.
- ↑ Kim IH, Choi KC, An BS, Choi IG, Kim BK, Oh YK, Jeung EB (July 2003). "Effect on abortion of feeding Korean pine needles to pregnant Korean native cows". Canadian Journal of Veterinary Research. Canadian Veterinary Medical Association. 67 (3): 194–197. PMC 227052. PMID 12889725.
- 1 2 Njaa BL, ed. (2011). Kirkbride's Diagnosis of Abortion and Neonatal Loss in Animals. John Wiley & Sons. ISBN 978-0-470-95852-0.
- ↑ Overton R (March 2003). "By a Hair" (PDF). Paint Horse Journal. Archived from the original (PDF) on 18 February 2013. Retrieved 19 December 2012.
- ↑ Adams KR, Fetterplace LC, Davis AR, Taylor MD, Knott NA (January 2018). "Sharks, rays and abortion: The prevalence of capture-induced parturition in elasmobranchs". Biological Conservation. 217: 11–27. Bibcode:2018BCons.217...11A. doi:10.1016/j.biocon.2017.10.010. S2CID 90834034. Archived from the original on 23 February 2019. Retrieved 30 July 2019.
- ↑ "Herpesvirus in dog pups". petMD. Archived from the original on 9 November 2013. Retrieved 18 December 2012.
- ↑ "Spaying Pregnant Females". Carol's Ferals. Archived from the original on 18 November 2012. Retrieved 17 December 2012.
- ↑ Coates J (7 May 2007). "Feline abortion: often an unnerving necessity". petMD. Archived from the original on 21 January 2012. Retrieved 18 December 2012.
- ↑ Khuly P (1 April 2011). "Feline abortion: often an unnerving necessity (Part 2)". petMD. Archived from the original on 18 November 2012. Retrieved 18 December 2012.
- ↑ Schwagmeyer PL (1979). "The Bruce Effect: An Evaluation of Male/Female Advantages". The American Naturalist. 114 (6): 932–938. doi:10.1086/283541. JSTOR 2460564. S2CID 85097151.
- ↑ McKinnon AO, Voss JL (1993). Equine Reproduction. Wiley-Blackwell. p. 563. ISBN 0-8121-1427-2. Archived from the original on 15 March 2015.
- ↑ Berger J (5 May 1983). "Induced abortion and social factors in wild horses". Nature. 303 (5912): 59–61. Bibcode:1983Natur.303...59B. doi:10.1038/303059a0. PMID 6682487. S2CID 4259800.
- ↑ Pluhácek J, Bartos L (April 2000). "Male infanticide in captive plains zebra, Equus burchelli" (PDF). Animal Behaviour. 59 (4): 689–694. doi:10.1006/anbe.1999.1371. PMID 10792924. S2CID 10961845. Archived from the original (PDF) on 18 July 2011.
- ↑ Pluhacek J, Bartoš L (2005). "Further evidence for male infanticide and feticide in captive plains zebra, Equus burchelli" (PDF). Folia Zoologica. 54 (3): 258–262. Archived from the original (PDF) on 22 February 2012. Retrieved 12 April 2009.
- ↑ Kirkpatrick JF, Turner JW (1991). "Changes in Herd Stallions among Feral Horse Bands and the Absence of Forced Copulation and Induced Abortion". Behavioral Ecology and Sociobiology. 29 (3): 217–19. doi:10.1007/BF00166404. JSTOR 4600608. S2CID 32756929.
- ↑ Agoramoorthy G, Mohnot SM, Sommer V, Srivastava A (1988). "Abortions in free ranging Hanuman langurs (Presbytis entellus) – a male induced strategy?". Human Evolution. 3 (4): 297–308. doi:10.1007/BF02435859. S2CID 84849590.
Bibliography
- Coppens C (1907). . In Herbermann C (ed.). Catholic Encyclopedia. Vol. 1. New York: Robert Appleton Company.
- Devereux G (1976). A Study of Abortion in Primitive Societies. International Universities Press. ISBN 978-0-8236-6245-6.
- Doan AE (2007). Opposition and Intimidation: The abortion wars and strategies of political harassment. University of Michigan.
- Ganatra B, Tunçalp Ö, Johnston HB, Johnson BR, Gülmezoglu AM, Temmerman M (March 2014). "From concept to measurement: operationalizing WHO's definition of unsafe abortion". Bulletin of the World Health Organization. 92 (3): 155. doi:10.2471/BLT.14.136333. PMC 3949603. PMID 24700971.
- Hartmann B (1995). Reproductive Rights and Wrongs: The Global Politics of Population Control. South End Press. ISBN 978-0-89608-491-9.
- Koblitz AH (2014). Sex and Herbs and Birth Control: Women and Fertility Regulation Through the Ages. Kovalevskaia Fund. ISBN 978-0-9896655-0-6.
- Riddle JM (1997). Eve's Herbs: A History of Contraception and Abortion in the West. Harvard University Press.
- Sedgh G, Bearak J, Singh S, Bankole A, Popinchalk A, Ganatra B, et al. (July 2016). "Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends". Lancet. 388 (10041): 258–267. doi:10.1016/S0140-6736(16)30380-4. PMC 5498988. PMID 27179755.
- UN (2002). Abortion Policies: A Global Review 3 vols. Population Division, Department of Economic and Social Affairs, United Nations. Archived from the original on 11 January 2005. Retrieved 28 June 2017.
- WHO (2005). The World Health Report 2005: Make every mother and child count. Geneva: World Health Organization. ISBN 92-4-156290-0. Archived from the original on 13 April 2005.
- WHO (2012). Safe abortion: technical and policy guidance for health systems (PDF) (2nd ed.). Geneva: World Health Organization. ISBN 978-92-4-154843-4. Archived (PDF) from the original on 16 January 2015. Retrieved 2 November 2014.
- WHO (2016). "Health worker roles in providing safe abortion care and post-abortion contraception". Archived from the original on 29 March 2019. Retrieved 8 January 2017.
External links
| Library resources about Abortion |
- WHO fact sheet on abortion
- Safe abortion: Technical & policy guidance for health systems, World Health Organization (2015)
- First-trimester abortion in women with medical conditions. US Department of Health and Human Services